Vascular: AAA Repair
Open AAA Repair
Selection of Approach
- Transperitoneal Approach:
- More Rapid Access (Best in Emergencies)
- Better Access to Right Renal Artery
- Better Access to Iliac/Femoral Arteries
- Retroperitoneal Approach:
- Better Access to Visceral & Supraceliac Aorta
- Better Access to Left Renal Artery
- Avoids Adhesions from Prior Operations
- Controversy if Equivalent or Lower Complications with Retroperitoneal Approach
Transperitoneal Approach
- Position: Supine & Arms Abducted
- Exposure:
- Midline Incision
- Retract Transverse Colon Cephalad
- Retract Small Bowel to the Right
- Divide the Ligament of Treitz & Retract Duodenum to the Right
- Avoid Injury to IMV
- Incise Posterior Peritoneum from Ligament of Treitz Down to the Extent Necessary for Repair
- Angle to the Right of Aortic Midline to Avoid Injury to IMA
- If Suprarenal Clamp Needed – Open Posterior Peritoneum Up to the Level of the Renal Veins
- May Require Renal Vein Division (Divide Close to IVC to Allow Collateral Drainage Through Gonadal, Adrenal & Lumbar Veins)
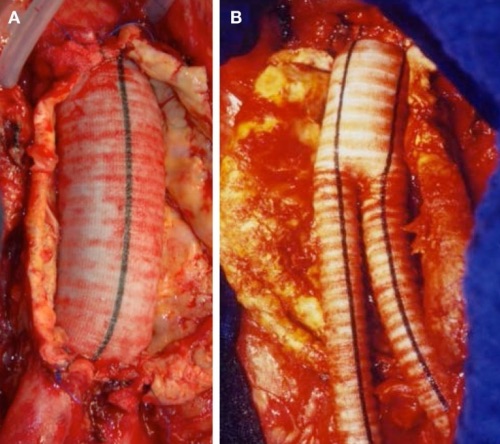
- Repair:
- Systemic Heparinization
- Clamp Iliacs Distally & Proximal Aorta
- Distal First to Prevent Thrombus Embolization from Proximal Clamp)
- Incise an Aortotomy Longitudinally with a T-Shape on Either End
- Preform Proximal End-to-End Anastomosis
- First Clear Anastomotic Sites of Thrombus
- Clear Thrombus from the Aneurysmal Sac
- Preform Distal End-to-End Anastomoses
- First Clear Anastomotic Sites of Thrombus
- Allow Flushing of Graft & Back-Bleeding Before Completing the Anastomoses
- Closure:
- Achieve Hemostasis
- Close Aneurysmal Sac Over the Graft
- Close Posterior Peritoneum
- Use Omentum to Separate Graft from Bowel if Unable to Close Sac or Peritoneum
- Prevents Future Aortoenteric Fistula
- Close Abdominal Wall
Retroperitoneal Approach
- Position: Right Lateral Decubitus
- Exposure:
- Curved Skin Incision
- Start Along the 10th Intercostal Space at the Posterior Axillary Line
- Run onto the Abdomen Lateral to the Lateral Border of the Rectus Muscle
- Bluntly Dissect Peritoneum Off the Abdominal Wall
- Identify Left Psoas Muscle Retract Peritoneal/Retroperitoneal Contents Anteromedially
- Identify & Protect Left Ureter
- May Divide Left Diaphragmatic Crus to Better Access Supraceliac Aorta
- Curved Skin Incision
- Repair:
- Systemic Heparinization
- Clamp Iliacs Distally & Proximal Aorta
- Distal First to Prevent Thrombus Embolization from Proximal Clamp)
- Incise an Aortotomy Longitudinally with a T-Shape on Either End
- Resect the Left Renal Artery with a Small Portion of Surrounding Aorta for Later
- May Preform Endarterectomy or Deploy Stent in Stenosed Celiac or SMA
- Preform Proximal End-to-End Anastomosis
- Proximal End Must Be Beveled to Include the Celiac, SMA and Right Renal Artery
- First Clear Anastomotic Sites of Thrombus
- Anastomose Left Renal Artery Back to a Side-Branch of the Graft
- Migrate Proximal Clamp Below the Renal Arteries to Minimize Ischemia Time
- Clear Thrombus from the Aneurysmal Sac
- Preform Distal End-to-End Anastomoses
- First Clear Anastomotic Sites of Thrombus
- Allow Flushing of Graft & Back-Bleeding Before Completing the Anastomoses
- Closure:
- Achieve Hemostasis
- Return Peritoneal Sac to Normal Configuration
- Close Abdominal Wall
Specific Vessel Considerations
- IMA Reimplantation Indications:
- SMA Stenosis
- Large IMA
- Backpressure < 40 mmHg (Poor Collaterals)
- Previous Colectomy (Risk Injury to Collaterals)
- Lumbar Arteries:
- Ligate if Bleeding
Open AAA Repair 1
Endovascular Aneurysm Repair (EVAR)
Anatomic Requirements
- Aortic Neck (Area Below Renal Arteries & Proximal to Aneurysmal Sac)
- Diameter < 32 mm (To Allow the Largest Available Graft)
- Length ≥ 10-15 mm
- Angulation < 60 Degrees
- Iliacs
- External Iliac Diameter ≥ 7 mm
- Normal Common Iliac Length ≥ 10-20 mm (Allow Adequate Seal)
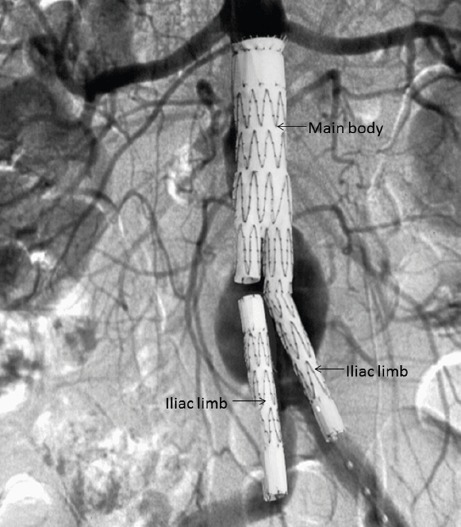
EVAR Components 2
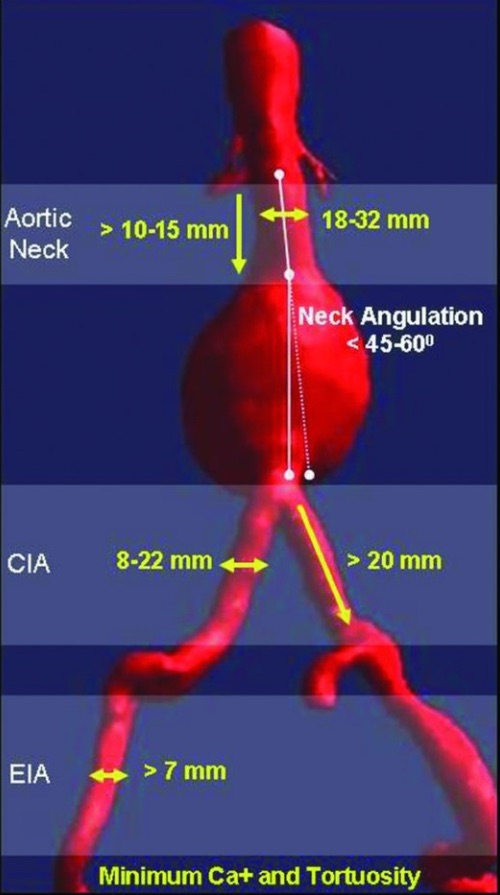
EVAR Requirements 3
Complications
Endoleak
- Definition: Persistent Blood Flow into the Aneurysmal Sac After Graft Placement
- Types: Mn
- Type I: Incompetent Seal at Attachment Sites
- Ia: Proximal End
- Ib: Distal End
- Type II: From Collaterals (IMA, Lumbars or Accessory Renals) – Most Common (76%)
- Type III: From Overlap Sites or Tear
- IIIa: Module Disconnection
- IIIb: Fabric Disruption
- Type IV: From Porous Graft Wall or Suture Holes
- Type V: Endotension (Expansion Without Defined Leak)
- Type I: Incompetent Seal at Attachment Sites
- Treatment:
- Type I: Repeat Balloon Dilation or Additional Stents to Cover
- Type II: Observe (Often Resolves Spontaneously)
- Transarterial Embolization (TAE) if Expands > 5 mm in Follow Up
- Type III: Additional Stents to Cover
- Type IV: Observe (Typically Resolve After 24-Hours with Anticoagulation Reversal)
- Type V: Repeat Endovascular Repair with New Lower-Porosity Graft
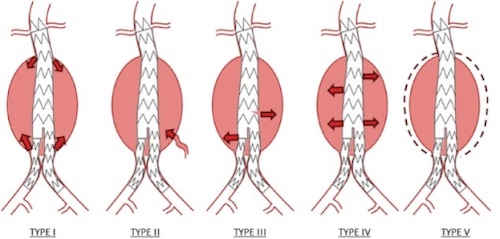
Endoleak Types 2
Mortality
- Most Common Early Cause of Death: MI
- Most Common Late Cause of Death: Renal Failure
Renal Failure
- #1 Risk Factor of Any Complication: Cr > 1.8
- Rates:
- Acute Renal Failure: 15-20%
- Dialysis-Dependent Renal Failure: 2.5%
- Risk Factors:
- Preoperative Hypotension #1
- Age
- Prolonged Clamp Time
- Suprarenal Clamping
Colonic Ischemia
- Most Common Site: Left Colon (From IMA Injury)
- High Mortality (25-55%)
- Risk Factors:
- Preoperative Shock (Strongest Risk Factor)
- Perioperative Transfusion Requirement
- Ruptured Aneurysm
- Open Repair
- Proximal Extension
- Perioperative Renal Failure Requiring Dialysis
- Diabetes
- Female Gender
- *IMA Reimplantation Not Clearly Associated
- Presentation: Early Bloody Diarrhea
- Dx: Proctosigmoidoscopy (Friable Mucosa)
- *Anoscopy Viewing Rectum Alone is Not Sufficient (Has Collateral Blood Flow)
- Tx:
- Partial Thickness: Bowel Rest
- Full Thickness, Peritonitis or Uncertain: Laparotomy & Resection
Aortoenteric Fistula
- Graft Erodes into Duodenum (Third-Fourth Portions) at the Proximal Graft Site
- Sx: Herald Bleed with Hematemesis
- Dx: EGD (First to Rule Out Other Source of Bleeding), CT
- Tagged Nuclear WBC Scan if Others Negative
- If Unstable: Temporize with an Aortic Stent Graft Over the Fistula
- Definitive Tx Options: Excise All Synthetic Graft Material
- Classic Technique: Extra-Anatomic Axillobifemoral Bypass & Fistula Closure
- In Situ (Not Extra-Anatomic) Reconstruction Repair Options:
- Lower Extremity Deep Veins
- Cadaveric Human Aortic Homograft
- Antibiotic-Impregnated Synthetic Grafts
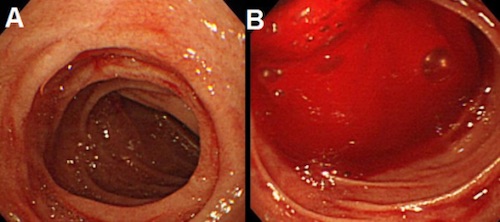
Aortoenteric Fistula on EGD 4
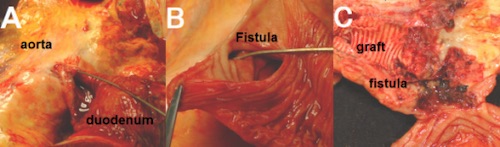
Aortoenteric Fistula 4
Other Complications
- Lower Extremity Ischemia
- Spinal Cord Ischemia
- Respiratory Failure & Pneumonia
- VTE
- Graft Infection
- Most Common Organisms: Staph #1 & E. coli #2
- Tx: Extra-Anatomic Bypass (Axillobifemoral)
- Chylous Ascites
- Major Vein Injury
- Impotence
- Pseudoaneurysm
- Atherosclerotic Occlusion
Mnemonics
Endoleak Types
- I – Basic Leak from Edges
- II – From ‘Secondary’ Vessels
- III – Envision a Tube (I) Within a Tube (II)
- IV – “Doors”/Pores
References
- Piechota-Polanczyk A, Jozkowicz A, Nowak W, Eilenberg W, Neumayer C, Malinski T, Huk I, Brostjan C. The Abdominal Aortic Aneurysm and Intraluminal Thrombus: Current Concepts of Development and Treatment. Front Cardiovasc Med. 2015 May 26;2:19. (License: CC BY-4.0)
- England A, Mc Williams R. Endovascular aortic aneurysm repair (EVAR). Ulster Med J. 2013 Jan;82(1):3-10. (License: CC BY-NC-SA-4.0)
- Schanzer A, Messina L. Two decades of endovascular abdominal aortic aneurysm repair: enormous progress with serious lessons learned. J Am Heart Assoc. 2012 Jun;1(3):e000075. (License: CC BY-2.5)
- Shitara K, Wada R. Gastrointestinal bleeding after aortic surgery: a case report. Cases J. 2009 Nov 23;2:9074. (License: CC BY-2.0)