Trauma: Abdominal/Pelvic Vascular Trauma
Abdominal/Pelvic Vascular Injury
AAST Abdominal Vascular Injury Scale
- *See AAST
- Injury Scale is Under Copyright
Retroperitoneal Hematoma Management
- Zone I (Central): Mandatory Exploration
- *Between Kidneys from Diaphragm to IVC Bifurcation
- Associated with Pancreaticoduodenal & Major Vascular Injury
- Zone II (Lateral):
- Penetrating: Selective Exploration
- Blunt: Open Only if Expanding, Pulsatile or with Active Hemorrhage
- *First Step: Palpate Contralateral Kidney to Assess Size & Determine Need for Heroic Measures to Save Ipsilateral Kidney
- Zone III (Pelvis):
- Penetrating: Mandatory Exploration
- Blunt: Open Only if Expanding, Pulsatile or with Active Hemorrhage
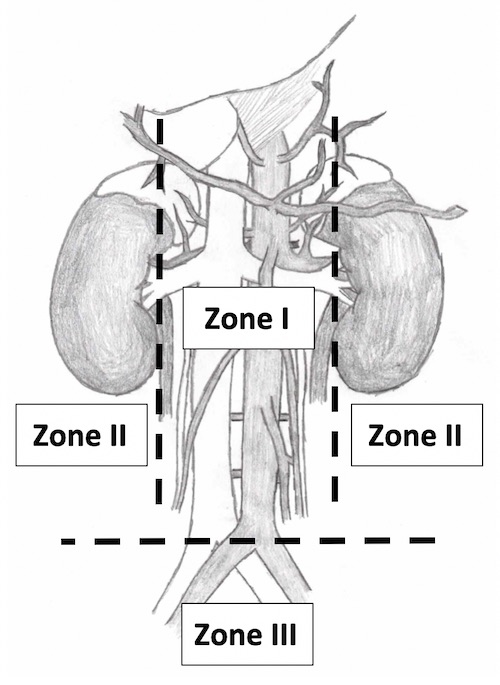
Retroperitoneal Zones
Aorta Injury
- Small: Lateral Aortorrhaphy with Permanent Suture
- Connect Multiple Wounds if Close to Each Other
- Large or Significant Narrowing: Patch Angioplasty
- Consider Interposition Graft if Infrarenal
IVC Injury
- Retrohepatic IVC Injury
- Infrahepatic IVC Injury
- Stable:
- < 50% Diameter: Primary Repair (Venorrhaphy)
- > 50% Diameter: Patch (Saphenous Vein or Synthetic)
- Unstable: Infrarenal Ligation
- Monitor for Compartment Syndrome
- Considerations:
- Apply Pressure to Stop Bleeding
- Do Not Clamp (Will Tear Easily)
- Posterior Wall Injury: Cut Through Anterior Wall to Access
- May Require Right Common Iliac Division to Visualize Distal IVC or Bifurcation
- Primary Repair Artery Later
- Apply Pressure to Stop Bleeding
- Stable:
Arterial Branch Injuries
Celiac Axis
- Simple: Arteriorrhaphy
- Complex: Ligate (Good Collaterals)
- Gallbladder Has Poor Collaterals – Cholecystectomy Indicated
Common Hepatic Artery
Renal Artery
- Small: Lateral Arteriorrhaphy
- Large: Interposition Graft (Saphenous or PTFE)
- Damage Control: Nephrectomy
- Only if Contralateral Kidney Palpated as Normal
Superior Mesenteric Artery
- Fullen Classification
- Zone I – Proximal to First Branch (Inferior Pancreaticoduodenal)
- Zone II – Distal to First Branch
- Zone III – Distal to Middle Colic
- Zone IV – Segmental Branches
- Proximal (Zone I/II):
- Stable: Primary Repair vs Bypass Graft to Distal Infrarenal Aorta
- Cover Graft with Retroperitoneal Fat or Omentum to Prevent Aortoenteric Fistula
- Unstable: Primary Repair vs Ligation
- Consider Intraluminal Shunt in Damage Control to Avoid Ligation
- Collaterals Often Inadequate for Ligation if Unstable
- Distal (Zone III/IV): Primary Repair vs Ligation
- Ligation Poorly Tolerated Since Distal to Collaterals
- Stable: Primary Repair vs Bypass Graft to Distal Infrarenal Aorta
Inferior Mesenteric Artery
- < 50% Diameter: Primary Repair
- > 50% Diameter: Ligate
Iliac Arteries
- Common or External Iliac: Repair
- Options:
- Lateral Arteriorrhaphy
- Grafting
- Replace with Mobilized Ipsilateral Internal Iliac
- Transposition to Contralateral Iliacs if at Bifurcation
- Consider Extra-Anatomic Bypass if Significant Contamination Present
- Options:
- Internal Iliac: Can Ligate Both with Impunity
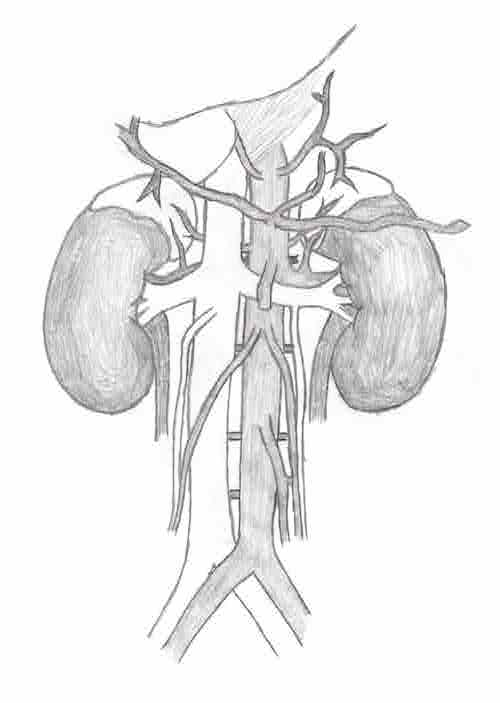
Abdominal Vasculature
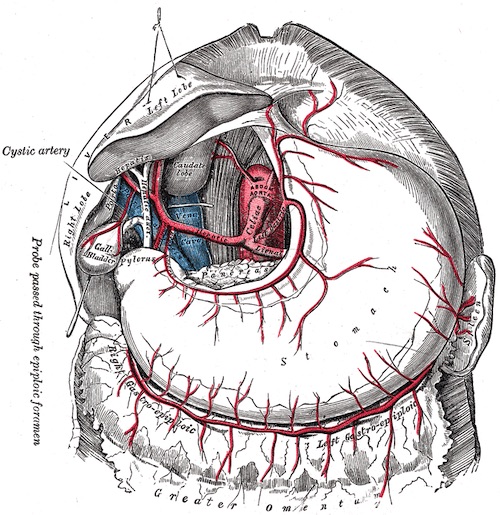
Celiac Artery 1
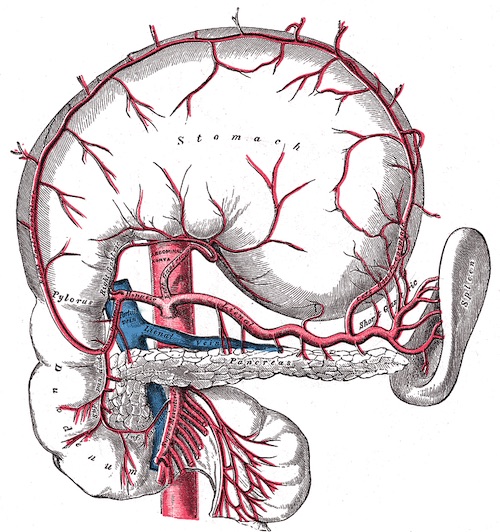
Celiac Artery 1
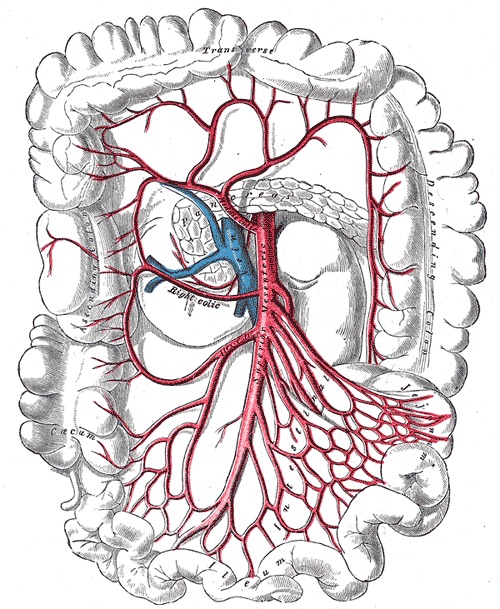
SMA 1
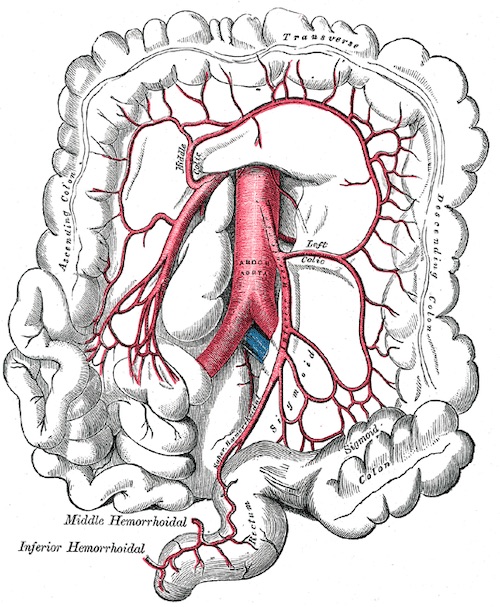
IMA 1
Venous Injuries
Other Venous Injury
- Can Ligate Any Vein Distal to Renals If Necessary
Superior Mesenteric Vein
- Repair vs Ligation
Portal Vein Injury
Renal Veins
- Left Renal Vein
- Good Collaterals (Adrenal/Gonadal)
- Tx: Lateral Venorrhaphy
- If Unable or Damage Control: Ligate Near IVC
- Right Renal Vein
- Shorter Than Left, Poor Collaterals
- Tx: Lateral Venorrhaphy
- If Forced to Ligate Preform Nephrectomy Also
References
- Gray H. Anatomy of the Human Body (1918). Public Domain.