Trauma: Approach to Abdominal Trauma
Blunt Abdominal Trauma (BAT)
Mechanism of Injury
- Crushing Force – Direct Compression Causing Injury
- Shearing Force – Tearing from Acceleration/Deceleration Around Fixed Attachments
- Bursting Force – Force Causing Acutely Increased Intraluminal Pressure within Hollow Organs Leading to Rupture
Injury Patterns
- Spleen (40-55%)
- Most Common Injury Requiring Intervention
- *Most Common Injured Organ Overall in Blunt Trauma Remains Controversial – Reports Vary Between Spleen & Liver
- Liver (35-45%)
- Small Bowel (5-10%)
- The Most Common Missed Abdominopelvic Injury on CT in Trauma
Approach to BAT
- Peritonitis/Evisceration: Laparotomy
- Unstable: FAST vs DPL
- Positive: Laparotomy
- Negative: CT
- Stable: CT
Penetrating Abdominal Trauma (PAT)
Mechanism of Injury
- Direct Injury – Tearing & Crushing Force Through Tissue Along the Trajectory of the Projectile & its Fragments
- Gunshot Wounds Have an Additional Dissipation of Kinetic Energy That Causes Further Damage
- Cavitation – As a High Energy Projectile Moves Through Tissue Energy Causes a Radial Stretching, Forming a Temporary Cavity with Additional Tissue Damage
- Higher Energy Projectiles Create Larger Cavities & Cause More Damage
- Shock Wave – The Projectile Creates Rapid Changes in Pressure & Temperature that Propagate Through Tissue Causing Additional Injury
Injury Patterns
- Small Bowel (50%) – Most Common
- Colon (40%)
- Liver (30%)
- Some Older Texts Report as the Most Common
- Vascular Injury (25%)
Approach to PAT
- Peritonitis/Evisceration: Laparotomy
- Unstable: Laparotomy
- Stable:
- Anterior Abdomen: Local Wound Exploration (Evaluating Fascial Violation)
- No Fascial Violation: Discharge Home
- Fascial Violation: FAST/DPL vs CT vs Diagnostic Laparoscopy
- No Peritoneal Violation: 24-Hour Serial Exams
- Peritoneal Violation: Laparotomy vs Diagnostic Laparoscopy
- *Consider Laparoscopy in Stable Penetrating Abdominal Trauma (Avoids Nontherapeutic Laparotomy)
- Flank/Back: CT
- Anterior Abdomen: Local Wound Exploration (Evaluating Fascial Violation)
- In Stab Wounds:
- 50-70% Penetrate Peritoneum
- Of Those 50% Require Repair of Intraabdominal Injury
Advanced Bedside Evaluation
Focused Assessment with Sonography for Trauma (FAST)
- Rapid Bedside US to Evaluate for Free Intraperitoneal Fluid & Pericardial Effusion
- Use Curvilinear Probe
- Can Visualize ≥ 250 cc Fluid
- For ≥ 1 L Fluid 84% Sensitive & 71% Specific
- Windows:
- Pericardial
- Should Be the First Area Viewed (Blood of Heart Allows Proper Gain Setting)
- Perihepatic (Morison’s Pouch)
- Most Sensitive Area for Free Intraperitoneal Fluid (Most Dependent Position When Supine)
- Perisplenic
- Pelvic/Perivesicular
- Pericardial
- Extended “E-FAST”
- Evaluates for Pneumothorax
- “Pleural Sliding” or “Comet Tail” Artifacts are Normally Seen – Lost in PTX
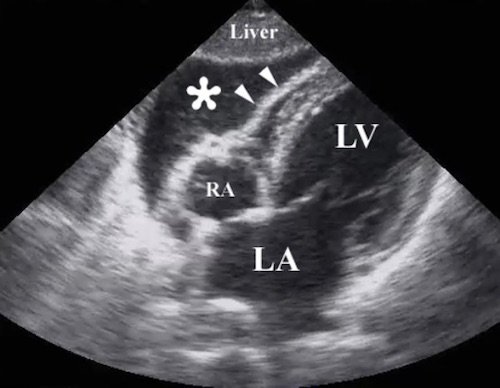
FAST: Pericardial Window (Positive) 1
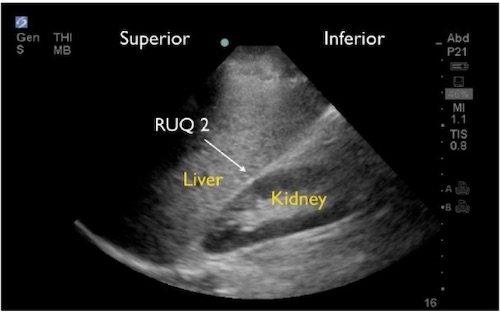
FAST: Perihepatic Window 2
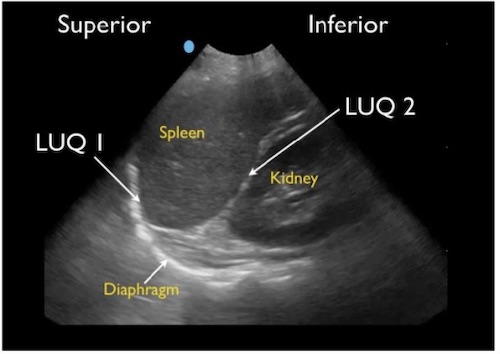
FAST: Perisplenic Window 2
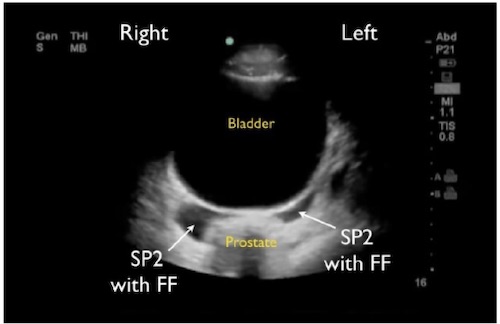
FAST: Pelvic Window (Positive) 2
Diagnostic Peritoneal Lavage (DPL)
- Bedside Evaluate for Occult Hemorrhage
- Procedure:
- First: NG & Foley to Decompress
- 2 cm Incision Made Above or Below Umbilicus to Expose Linea Alba
- Divide Fascia & Peritoneum
- PD Catheter Directed to Pelvis & Fascia Closed (Purse String)
- Aspirate Peritoneal Fluid
- Positives: 10 cc Blood, Bile or Succus
- If Negative – Lavage with 1 L Saline
- Secondarily Positive:
- > 100,000 RBC per mL
- 500 WBC per mL
- Gram Stain Positive
- Almost Entirely Replaced by FAST/CT
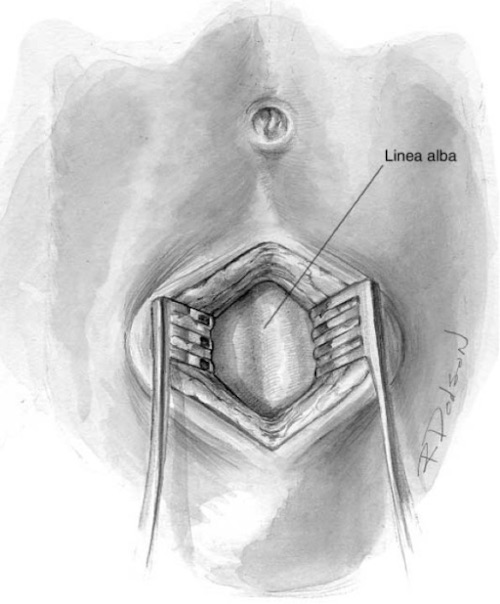
DPL: Expose Linea Alba 3
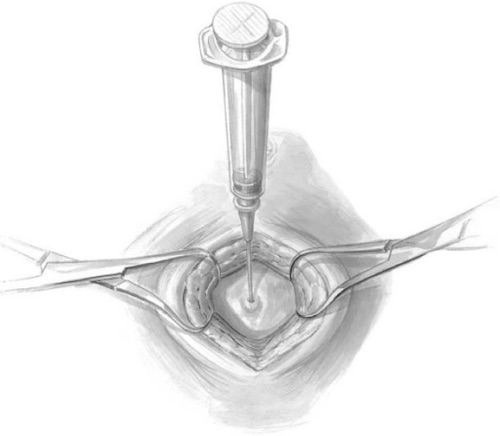
DPL: Access the Peritoneal Cavity 3
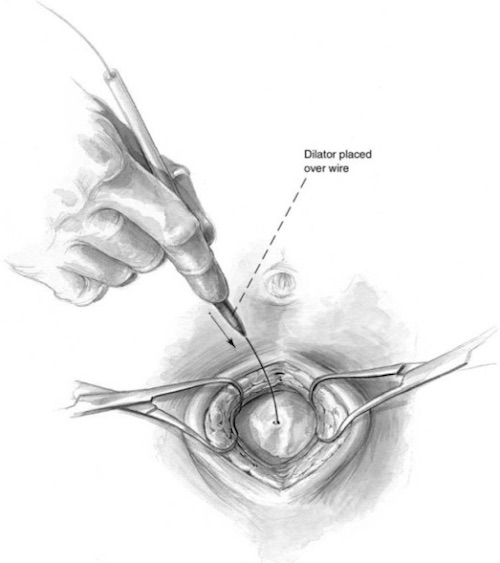
DPL: Place Catheter Over a Guidewire 3
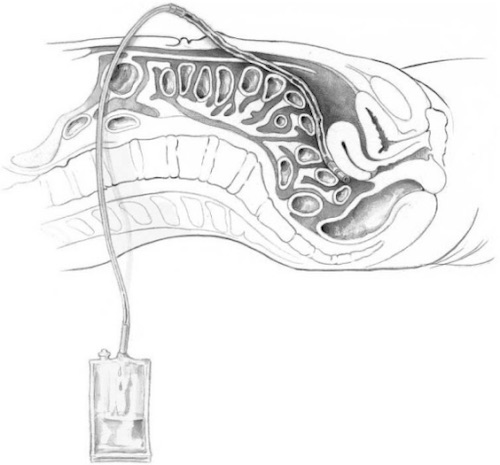
DPL: Instill Fluid & Collect Back 3
References
- Gillman LM, Ball CG, Panebianco N, Al-Kadi A, Kirkpatrick AW. Clinician performed resuscitative ultrasonography for the initial evaluation and resuscitation of trauma. Scand J Trauma Resusc Emerg Med. 2009 Aug 6;17:34. (License: CC BY-2.0)
- Lobo V, Hunter-Behrend M, Cullnan E, Higbee R, Phillips C, Williams S, Perera P, Gharahbaghian L. Caudal Edge of the Liver in the Right Upper Quadrant (RUQ) View Is the Most Sensitive Area for Free Fluid on the FAST Exam. West J Emerg Med. 2017 Feb;18(2):270-280. (License: CC BY-4.0)
- Whitehouse JS, Weigelt JA. Diagnostic peritoneal lavage: a review of indications, technique, and interpretation. Scand J Trauma Resusc Emerg Med. 2009 Mar 8;17:13. (License: CC BY-2.0)