Abdominal Wall Reconstruction/Component Separation
David Ray Velez, MD
The Operative Review of Surgery. 2023; 1:197-203.
Table of Contents
Definitions
Definitions
- Component Separation Techniques (CST): Techniques to Separate the Muscular/Fascial Components of the Abdominal Wall to Decrease Tension on the Midline Closure
- Anterior Component Separation (ACS): Isolation and Division of the External Oblique Muscle
- Perforator-Preserving Techniques (PP-ACS): Modified ACS Techniques that Allow Preservation of the Deep Epigastric Perforating Vessels
- Posterior Component Separation (PCS): Separation of the Transversus Abdominis from the Internal Oblique Muscle
- Required Division of the Neurovascular Bundle with Denervation of Rectus Abdominis
- Transversus Abdominis Release (TAR): Isolation and Division of the Transversus Abdominis Muscle – Generally Done as a Modification to a PCS (PCS-TAR)
Goals of Surgery
- Generally Performed as Part of a Retrorectus Ventral Hernia Repair
- The Primary Goal of Component Separation is to Relieve Tension on the Midline Fascia and Promote Closure
- Can Also Facilitate Placement of a Large Retrorectus Mesh
Release
- Releases 7-10 cm Per Side (Total of Up to 20 cm After Both Sides Released) 1,2
- 5 cm in the Upper Abdomen
- 8-10 cm in the Middle Abdomen
- 3-6 cm in the Lower Abdomen
- Exact Length of Release is Debated and Similar Lengths are Generally Reported
- Some Believe Anterior Component Separation to Create More Medialization of the Fascia
Anterior Component Separation (ACS)
Technique
- Generally Performed as Part of a Ventral Hernia Repair After Hernia Reduction and Lysis of Adhesions
- Step 1. Create Subcutaneous Flaps
- Extend Flaps Laterally to the Anterior Axillary Line (Lateral to the External Oblique Insertion)
- Avoid Excessively Large Flaps – The Largest Source of Morbidity
- Step 2. Incise the External Oblique Aponeurosis
- Start 2 cm Lateral to Semilunar Line/Rectus Sheath
- Extend from the Costal Margin to the Pubis
- Step 3. Free the External Oblique from the Internal Oblique
- Extend as Far Laterally as Possible
Reconstruction
- Generally Reinforced with Placement of Mesh – Most Often in the Retrorectus Position
- Reapproximate the Anterior Rectus Sheath to the Midline
- Consider Closed-Suction Drain Placement (Debated)
- Close Skin
Modifications
- Posterior Rectus Sheath Division
- Incision of the Posterior Rectus Sheath Above the Arcuate Line Can Provide Additional Length if Needed
- Adds an Additional 2-4 cm of Length
- Perforator-Preserving Techniques
- Various Techniques: *See Below
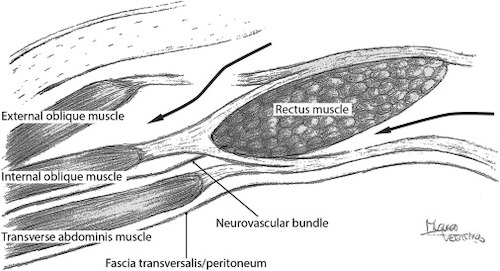
Anterior Component Separation with a Retrorectus Hernia Repair 1
Perforator-Preserving Techniques
Definition
- Anterior Component Separation (ACS) Techniques that Allow Preservation of the Deep Epigastric Perforating Vessels
- Various Techniques:
- Open Release with Preservation of Periumbilical Perforators
- Open Release with Additional Inguinal Incisions for Fascial Release
- Open Release with Additional Subcostal Incisions for Fascial Release
- Endoscopic Technique
- Minimally Invasive Component Separation (MICS)
- Decreases Rates of Wound Complication 3-5
Open Release with Preservation of Periumbilical Perforators
- A Superior Subcutaneous Flap is Created Above the Umbilicus and then Carried Out Laterally
- A Second Inferior Subcutaneous Flap is Created Below the Umbilicus and Carried Out Laterally
- The Two Flaps are Connected Laterally, Taking Care to Spare the Periumbilical Perforating Vessels
- The External Oblique Aponeurosis is then Incised
Open Release with Additional Inguinal Incisions for Fascial Release
- Separate Inguinal Incisions are Made (Similar to an Inguinal Hernia Repair)
- A Balloon Dissector is Placed Between the Internal and External Obliques
- The Balloon Dissector is then Inflated to Create the Space
- Fascial Separation is Completed Through the Inguinal Incision
Open Release with Additional Subcostal Incisions for Fascial Release
- Transverse Subcostal Incisions are Made
- Fascial Separation is Completed Through these Subcostal Incisions
Endoscopic Technique
- A Small 1-2 cm Incision is Made Below the Costal Margin Lateral to the Rectus Abdominis
- The Incision is Carried Down Through the External Oblique
- The Space Between Internal and External Oblique is Opened Using a Balloon Dissector and then Insufflated
- Using Endoscope/Laparoscope and Two Additional Ports the Plane is Dissected and the Fascia of the External Oblique is Divided
- Procedure is then Repeated on the Other Side
- Hernia Repair is Then Performed in a Traditional Open Fashion
Minimally Invasive Component Separation (MICS)
- Hernia is Reduced in a Minimally Invasive Fashion
- A Small 1-2 cm Incision is Made Below the Costal Margin Lateral to the Rectus Abdominis
- An Incision is Made Through the External Oblique Aponeurosis
- A Yankauer Suction Device is Used to Create a Space Between the Internal and External Oblique
- The Fascia of the External Oblique is Then Divided (Division Extends Superiorly to 12 cm Above the Costal Margin and Inferiorly to the Inguinal Ligament)
Posterior Component Separation (PCS) and Transversus Abdominis Release (TAR)
Posterior Component Separation (PCS) Technique
- Generally Performed as Part of a Retrorectus Ventral Hernia Repair After Hernia Reduction and Lysis of Adhesions
- Step 1. Incise the Dorsal Aspect of the Posterior Rectus Sheath 1 cm from the Medial Edge of the Rectus Muscle
- Enter the Retrorectus Space and Dissect Laterally to the Semilunar Line
- Take Care to Protect the Neurovascular Bundle Laterally Near the Semilunar Line
- Step 2. Incise the Ventral Aspect of the Posterior Rectus Sheath at Lateral-Most Edge
- Exposes the Underlying Transversus Abdominis Muscle
- Do Not Penetrate Through the Transversalis Fascia/Peritoneum
- Step 3. Dissect the Plane Laterally Between the Internal Oblique and Transversus Abdominis
Transversus Abdominis Release (PCS-TAR) Technique
- Step 1/Step 2: Same as Traditional PCS
- Step 3: Incise the Transversus Abdominis Muscle Along its Length at the Medial Aspect to Enter the Preperitoneal Space
- Do Not Penetrate Through the Transversalis Fascia/Peritoneum
- Step 4: Dissect the Plane Laterally Between the Transversus Abdominis (Anterior) and Transversalis Fascia/Peritoneum (Posterior)
Reconstruction
- Reapproximate the Posterior Rectus Sheath to Midline
- Typically Place a Large Retrorectus Mesh
- Reapproximate the Anterior Rectus Sheath to Midline
- Consider Closed-Suction Drain Placement (Debated)
- Close Skin
Modifications
- Laparoscopic PCS
- Robotic PCS
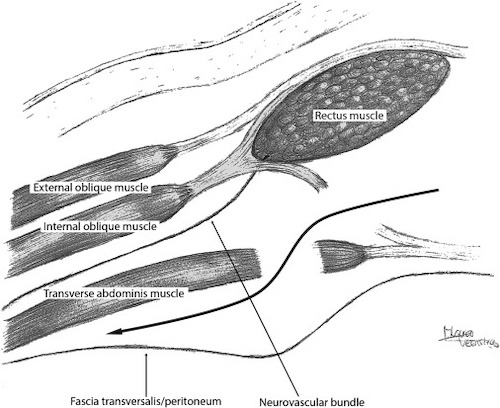
Posterior Component Separation with TAR 1
Complications
Hernia Recurrence Rates 6-14
- ACS: 12-15%
- PP-ACS: 7-11%
- PCS-TAR: 4-7%
- *ACS May Be Associated with Increased Rates of Recurrence Although the Exact Rates are Debated
Wound Complications 7-15
- Total Wound Complication Rates:
- ACS: 21-48%
- PP-ACS: 16-21%
- PCS-TAR: 15-25%
- Complications:
- Skin Flap Necrosis – Caused by Damage to the Perforating Vessels
- Surgical Site Infection (SSI)
- Skin Dehiscence
- Hematoma/Seroma
- Fistula Tract Formation
- *Generally Accepted that ACS Has Significantly Higher Rates of Skin Flap Necrosis and Total Wound Complications
- *PP-ACS and PCS-TAR are Generally Considered to Have Similar Rates of Wound Complications
Other Complications
- Abdominal Compartment Syndrome
- Massive Hernia Repairs with Loss of Domain May Result in Intraabdominal Hypertension
- Can Present as Pulmonary Complications
- *See Abdominal Compartment Syndrome
- Iatrogenic Spigelian Hernia
- Due to Disruption of the Linea Semilunaris
References
- Sneiders D, de Smet GHJ, den Hartog F, Verstoep L, Menon AG, Muysoms FE, Kleinrensink GJ, Lange JF. Medialization after combined anterior and posterior component separation in giant incisional hernia surgery, an anatomical study. Surgery. 2021 Dec;170(6):1749-1757. (License: CC BY 4.0)
- Heller L, McNichols CH, Ramirez OM. Component separations. Semin Plast Surg. 2012 Feb;26(1):25-8.
- Elhage SA, Marturano MN, Prasad T, Colavita PD, Kercher KW, Augenstein VA, Heniford BT. Impact of perforator sparing on anterior component separation outcomes in open abdominal wall reconstruction. Surg Endosc. 2021 Aug;35(8):4624-4631.
- Saulis AS, Dumanian GA. Periumbilical rectus abdominis perforator preservation significantly reduces superficial wound complications in “separation of parts” hernia repairs. Plastic and Reconstructive Surgery. 2002;109(7):2275-2280.
- Ghali S, Turza KC, Baumann DP, Butler CE. Minimally invasive component separation results in fewer wound-healing complications than open component separation for large ventral hernia repairs. Journal of the American College of Surgeons. 2012;214(6):981-989.
- Pauli EM, Rosen MJ. Open ventral hernia repair with component separation. Surg Clin North Am(2013) 93(5):1111–33.
- Switzer NJ, Dykstra MA, Gill RS, Lim S, Lester E, de Gara C, et al. Endoscopic versus open component separation: systematic review and meta-analysis. Surg Endosc(2015) 29(4):787–95.
- Cornette B, de Bacquer D, Berrevoet F. Component separation technique for giant incisional hernia: a systematic review. Am J Surg(2017):1–8.
- Carbonell AM, Cobb WS, Chen SM. Posterior components separation during retromuscular hernia repair. Hernia(2008) 12(4):359–62.
- Novitsky YW, Elliott HL, Orenstein SB, Rosen MJ. Transversus abdominis muscle release: a novel approach to posterior component separation during complex abdominal wall reconstruction. Am J Surg(2012) 204(5):709–16.
- Krpata DM, Blatnik JA, Novitsky YW, Rosen MJ. Posterior and open anterior components separations: a comparative analysis. Am J Surg(2012) 203(3):318–22.
- Novitsky YW, Fayezizadeh M, Majumder A, Neupane R, Elliott HL, Orenstein SB. Outcomes of posterior component separation with transversus abdominis muscle release and synthetic mesh sublay reinforcement. Ann Surg(2016) 264(2):226–32.
- Cornette B, de Bacquer D, Berrevoet F. Component separation technique for giant incisional hernia: a systematic review. Am J Surg(2017):1–8.
- Scheuerlein H, Thiessen A, Schug-Pass C, Köckerling F. What Do We Know About Component Separation Techniques for Abdominal Wall Hernia Repair? Front Surg. 2018 Mar 27;5:24.
- Clarke JM. Incisional hernia repair by fascial component separation: results in 128 cases and evolution of technique. Am J Surg(2010) 200(1):2–8.