Anorectal: Abscess & Fistula Procedures
Anorectal/Perirectal Abscess Drainage Procedures
Incision and Drainage (I&D)
- Positioning:
- Bedside: Lateral Decubitus
- OR: Prone Jack-Knife
- Inject Local Anesthetic
- Incision Over the Abscess
- Semilunar or Cruciate (Cross)
- Oriented Radially
- Orient Over the Side Closest to the Anal Verge
- Not Over the Area of Greatest Fluctuance or Area Furthest from Verge
- Subsequent Fistula are Shorter and More Simple
- For Large Cavities (> 5 cm): Consider Ipsilateral Counter-Incisions to Avoid an Unnecessarily Large Single Incision
- Bluntly Probe the Cavity to Break All Loculations and Drain All Fluid Pockets
- Avoid Over-Aggressive Disruption – Risk for Sphincter or Pudendal Nerve Injury
- Finish Options:
- May Consider Packing with Daily Changes
- Most Common Although No High-Quality Evidence of Any Benefit
- Excise ≥ 1 cm Segment of Skin to Prevent Premature Closure without Packing
- May Consider Packing with Daily Changes
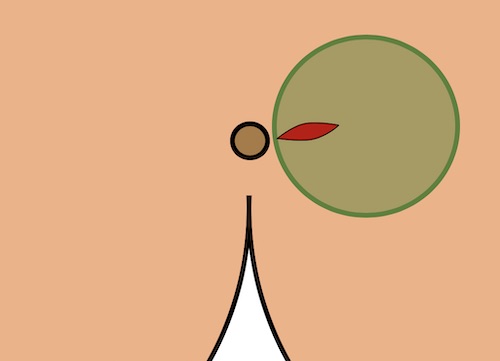
I&D
Hanley Procedure
- For Horseshoe Abscess
- Traditional Hanley Procedure: 3 Incisions
- Counter Incisions Over Each Bilateral Ileoanal Fossa
- Deep Space: Posterior Incision Between Coccyx & Anus or Through the Internal Anal Sphincter
- Counter Drains Placed Through Each Lateral Extension – Removed After 2-4 Weeks
- *High Risk for Anorectal Incontinence – Divided Posterior Sphincter Mechanism
- Modified Hanley Procedure: 2 Incisions with a Cutting Seton
- Counter Incisions Over Each Bilateral Ileoanal Fossa
- A Cutting Seton Over the Posterior Sphincter Mechanism is Serially Tightened Over Months
- *Posterior Sphincter is Replaced by Tethered Scar Tissue – Decreases Risk of Incontinence
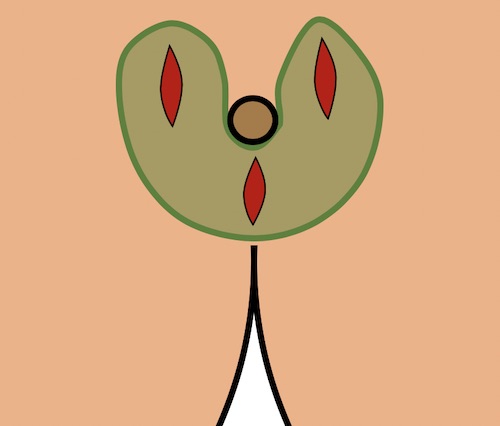
Hanley Procedure
Fistulotomy
Basics
- Fistula is Opened to Allow Drainage and Healing by Secondary Intention
Procedure
- Define the Fistula Tract
- Anoscopy to Identify the Internal Opening
- Insert a Fistula Probe Through the External Opening
- Direct Towards the Internal Opening
- Avoid Creating a False Passage
- Options if Unable to Identify:
- Inject Dilute Hydrogen Peroxide Through an Angiocatheter into the External Opening to Identify
- Using a Curved Fistula Probe Attempt to Identify the Tract from the Internal Opening to Identify
- Partial Fistulectomy
- Cannulate the Fistula with a Probe
- Divide the Tissue Overlying the Probe with Electrocautery
Outcomes
- Success Rate: > 90%
- Risk of Fecal Incontinence: 0-40% (Increased if Complex)
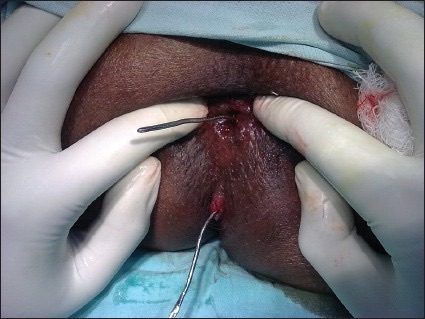
Fistula Probe 1
Setons
Basics
- Seton Material:
- Vessel Loop
- Thin Silastic Band
- Silk Suture
- Types:
- Noncutting/Draining Seton – Loose Connection at Skin Level
- Allows Continued Drainage & Promotes Fibrosis/Maturation
- Often Requires a Second-Stage Procedure Once Mature
- Procedures: Fistulotomy, LIFT or Advancement Flap
- Timing: After 6-10 Weeks
- May Wait 3-4 Months if More Complex
- May Be Definitive Treatment in Crohn’s or High-Risk Patients
- Cutting/Snug Seton – Tight Connection at Skin Level
- Slowly Tightened Every 4-6 Weeks
- Must Incise Skin Surface at Initial Placement – Cutting Seton on Skin is Painful
- Mostly Abandoned Due to High Risk of Fecal Incontinence
- Noncutting/Draining Seton – Loose Connection at Skin Level
Placement
- Define the Fistula Tract (Similar to Fistulotomy)
- A Seton is Passed Through the Fistula Tract & Secured to Itself in a Loop or Omega Shape
Outcomes
- Success Rate:
- Noncutting: 62-100%
- Cutting: 82-100%
- Risk of Fecal Incontinence:
- Noncutting: Rare
- Cutting: 30%

Seton 2
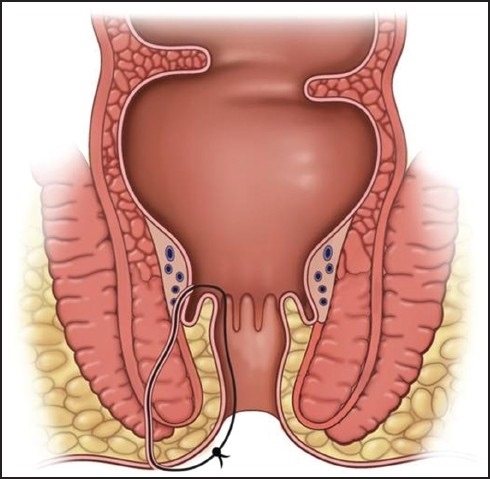
Seton Diagram 3
Ligation of Internal Fistula Tract (LIFT Procedure)
Basics
- Typically Preformed After Tract is Matured
- Fistula Tract is Divided in the Intersphincteric Space
Procedure
- Cannulate the Tract with a Fistula Probe
- Make a Skin Incision Over the Intersphincteric Groove
- Dissect Down the Intersphincteric Space to the Deep Fistula Tract
- Bluntly Define & Isolate the Tract Circumferentially
- Remove Probe
- Suture Ligate the Intersphincteric Tract & Sharply Divide
- Close the Skin
Outcomes
- Success Rate: 61-95%
- Risk of Fecal Incontinence: Rare
Endoanal/Endorectal Advancement Flap
Basics
- Resect Mucosa Around the Internal Opening and Pull-Down Rectal/Anal Mucosa to Cover
- Dermal Advancement Flap
- Pulls Up Skin Instead
- Preferred if Below Dentate Line to Prevent Mucosal Ectropion with Pruritis & Mucosal Drainage
Procedure
- Create a Flap of Mucosal Tissue Proximal to the Internal Opening
- Include Mucosa Around the Internal Opening
- Must Be Wide-Based (Width ≥ 2-3x Length) – Ensure Good Perfusion
- Excise Flap Tip Containing the Internal Mucosal Opening
- Manage the Tract
- Debride the Tract with a Curette
- Close Internal Opening with Suture
- Widen the External Opening to Ensure Good Drainage
- Pull Flap Distally and Reapproximate the Mucosal Edges
Outcomes
- Success Rate: 60-100%
- Risk of Fecal Incontinence: 0-12.5%
References
- Dutta G, Bain J, Ray AK, Dey S, Das N, Das B. Comparing Ksharasutra (Ayurvedic Seton) and open fistulotomy in the management of fistula-in-ano. J Nat Sci Biol Med. 2015 Jul-Dec;6(2):406-10. (License: CC BY-NC-SA-3.0)
- Tanner NC, Maw A. A novel technique for negotiation of a complex fistula-in-ano using a flexible ureteral catheter. Ann R Coll Surg Engl. 2014 Jan;96(1):80. (License: CC BY-3.0)
- Kolar B, Speranza J, Bhatt S, Dogra V. Crohn’s disease: Multimodality Imaging of Surgical Indications, Operative Procedures, and Complications. J Clin Imaging Sci. 2011;1:37. (License: CC BY-NC-SA-3.0)