Vascular: Aortic Dissection
Aortic Dissection
Basics
- Intimal Disruption Allows Blood Extravasation Between the Layers of the Wall
- Origination
- Ascending Aorta (50-65% – Most Common)
- Descending Aorta (20-30%)
- Aortic Arch (< 10%)
- High Mortality
- Ascending Dissection – From Cardiac Failure (Tamponade, Regurgitation/Insufficiency or Coronary Occlusion)
- Most Common Cause of Death: Cardiac Failure
- Descending Dissection – From End Organ Failure by Vessel Obstruction
- Ascending Dissection – From Cardiac Failure (Tamponade, Regurgitation/Insufficiency or Coronary Occlusion)
Pathophysiology
- Initial Lesion: Intimal Tear
- Blood Extravasation Between the Layers of the Vessel Wall
- Typically Spreads Antegrade but Can Spread Retrograde
- “False Lumen” Created Between “Intimal Flap” & Remaining Wall
- May Have Distal Fenestrations (Intimal Connections) to Maintain Patency
- Malperfusion Syndrome
- Occurs When Branch Occlusion Causes End-Organ Ischemia
- Dynamic Obstruction
- More Common (80%)
- Etiologies:
- Insufficient Flow Through the True Lumen – Varies with Vessel Circumference, Blood Pressure, Heart Rate and Peripheral Resistance
- Mobile Intimal Flap Prolapse Occluding Branch Vessel Ostium
- Obstruction is Intermittent in Nature & Responds Better to Beta-Blocker Management
- Static Obstruction
- Etiology: Narrowing/Occlusion of Branch Vessels from False Lumen Protrusion into the Branch Vessel with Associated Thrombosis
- Obstruction is Consistent
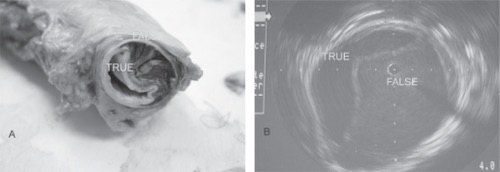
Aortic Dissection Specimen and Intravascular Imaging 1
Classification
- DeBakey Classification Mn
- Type I: Both – Tear Originates in Ascending & Extends to Descending
- Type II: Ascending – Tear Originates in Ascending & Confined to Ascending
- Type III: Descending – Tear Originates in Descending
- IIIa: Confined to Thoracic Aorta
- IIIb: Originates in Thoracic Aorta & Extends to the Abdominal Aorta
- Stanford Classification Mn
- Type A Aortic Dissection (TAAD): Originates in the Ascending Aorta
- Includes DeBakey Type I & II
- Type B Aortic Dissection (TBAD): Originates in the Descending Aorta
- Includes DeBakey Type III
- Type A Aortic Dissection (TAAD): Originates in the Ascending Aorta
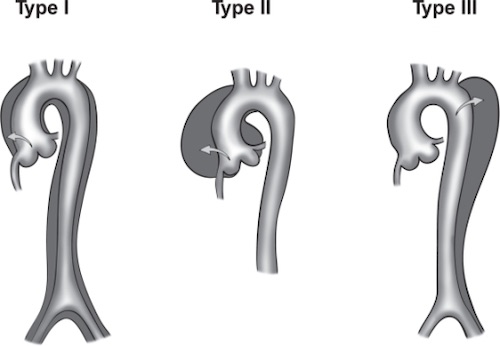
DeBakey Classification 1
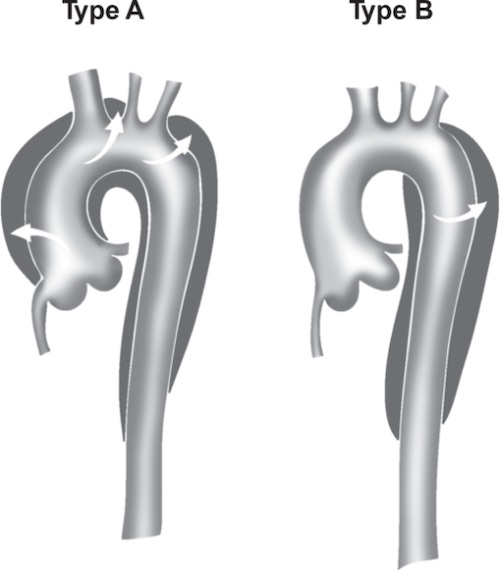
Stanford Classification 1
Risk Factors
- Hypertension (70%)
- Male Sex (4:1)
- Aortic Wall Abnormality (Bicuspid Aortic Valve, Coarctation)
- Cystic Medial Necrosis
- Connective Tissue Disorders (Marfan & Ehlers-Danlos)
- Pregnancy
- Cocaine
- Trauma
Presentation
- Pain (Back/Chest/Abdomen) – Most Common
- Pulse Deficit
- Limb Ischemia
- Mesenteric Ischemia
- Cardiac Tamponade
- Aortic Insufficiency
- Myocardial Infarction
- Syncope/Stroke
Diagnosis
- Gold Standard: CTA
- Highest Sensitivity: TEE

Aortic Dissection on CTA 1
Aortic Dissection – Treatment
Initial Management
- Initial Tx: β-Blockers & Vasodilator (Sodium Nitroprusside)
- Reduce Systolic Blood Pressure & Pulsatile Load/Aortic Stress (dP/dt – Derivative of Pressure/Time from Left Ventricle)
- Give β-Blockers Before Vasodilator – Avoid Reflex Sympathetic Stimulation
- Agent of Choice: Esmolol for Goal Systolic Blood Pressure < 120 mmHg within 20 Minutes
Type A
- Repair All Type A Aortic Dissections Mn
- Access: Median Sternotomy
- May Need Cervical/Supraclavicular Incisions to Visualize Great Vessels
- Procedure: Excision with Interposition Synthetic/Dacron Graft
- May Also Require Aortic Valve Replacement/Repair
Type B
- Uncomplicated: Medical Management
- *Role of Endovascular Stenting in Uncomplicated Patient’s is Evolving
- Complicated: Thoracic Endovascular Aortic Repair (TEVAR)
- Indications:
- Malperfusion Syndrome
- Refractory Severe Hypertension
- Refractory Severe Chest Pain
- Progression/Expansion
- Impending Rupture
- Indications:
- Ruptured: Open Surgical Repair
- Access: Left Posterolateral Thoracotomy
- May Need Thoracoabdominal Incision
- Access: Left Posterolateral Thoracotomy
Postoperative Complications
- Aortic Aneurysm
- Risk: 30%
- Paraplegia
- From Intercostal Artery Occlusion
- Recurrent Dissection
- Most Common in Marfan Syndrome
- “Bird’s Beaking” of Endograft
- Proximal Edge Pulled Away from Aortic Wall
- Allows for Recurrent Dissection
- Risks Graft Migration, Collapse or Occlusion
Mnemonics
DeBakey Classification
- Dissections are B.A.D.
- 1 – Both
- 2 – Ascending
- 3 – Descending
Stanford Classification
- A-A: Type A – Ascending
Repair of Aortic Dissections
- A-A: All Ascending Are Repaired
References
- Tran TP, Khoynezhad A. Current management of type B aortic dissection. Vasc Health Risk Manag. 2009;5(1):53-63. (License: CC BY-NC-3.0)