Vascular: Arteriovenous (AV) Hemodialysis Access
Arteriovenous Hemodialysis Access
Arteriovenous Fistula (AVF)
- Best Survival of Dialysis Options
- Timing:
- Refer to Vascular Surgery One Creatinine Clearance < 25 mL/min
- Per National Kidney Foundation KDOQI Guidelines
- Ideally Create 6 Months Prior to Anticipated Need
- Reduced Risk of Sepsis/Death (Largely from CVC Use)
- Refer to Vascular Surgery One Creatinine Clearance < 25 mL/min
- Requires 6 Weeks to Mature Prior to Use
- Rule of 6’s:
- 6 Weeks to Mature
- ≥ 2 x 3 = 6 mm Preoperative Diameters
- < 6 mm from Skin Best
- ≥ 6 in Segment Needed to Use
- Must Support > 600 cc/min Flow
Minimum Maturation Time Prior to Use
- CVC: Immediate
- PD Cath: 2 Weeks
- Prosthetic Graft: 2 Weeks
- AVF: 6 Weeks
AVF Site Selection
- Vasculature Requirements:
- Artery Diameter ≥ 2.0 mm
- Vein Diameter ≥ 2.0-3.0 mm
- Patent Palmer Arch
- General Approach:
- Upper Extremity is Preferred to Lower Extremity
- Easier Access & Lower Infection Risk
- Non-Dominant Arm Preferred Over Dominant Arm
- Most Distal Site Possible Preferred Over Proximal Sites
- Preserve Proximal Sites for Future Access
- Resulting Dilation of Proximal Veins Increases Success of Later Fistulas
- Autogenous AVF Preferred Over Prosthetic Grafts
- Higher Patency
- Lower Complications
- Upper Extremity is Preferred to Lower Extremity
- Highest Patency: End-of-Vein to Side-of-Artery
- Options:
- Posterior Radial Branch-Cephalic (Snuffbox) Fistula
- Radial-Cephalic (Cimino) Fistula
- High Early Failure Rate
- Brachial-Cephalic Fistula
- Easier Cannulation
- Brachial-Basilic Fistula
- Requires Superficialization of Deep Basilic Vein
- Often Done in Two-Stages (Mature Before Superficialization)
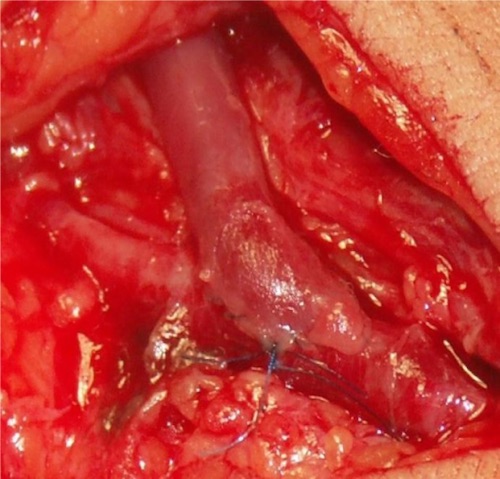
Cimino AVF 1
Prosthetic Grafts
- AVF Comparison:
- Grafts Have Lower Primary Patency
- Grafts Have Similar Long-Term Patency
- Grafts Have Worse Outcomes Overall
- Most Commonly Use 6 mm PTFE Grafts
- Requires 2 Weeks to Heal Prior to Use (No Maturation Needed)
- Use/Indications:
- Forearm Prosthetic Grafts Should Be Considered a Bridge to Autogenous Upper Arm Fistulas
- Upper Arm Prosthetic Grafts Used if No Adequate Veins are Available
- Options:
- Forearm:
- Radial-Antecubital Straight Access
- Radial-Antecubital Looped Access
- Brachial-Antecubital Looped Access
- Upper Arm:
- Brachial-Axillary Straight Access
- Brachial-Brachial Straight Access
- Proximal Radial-Axillary Straight Access
- Proximal Radial- Brachial Straight Access
- Forearm:
Other Options
- HeRO (Hemodialysis Reliable Outflow)
- Catheter Placed Through Stenotic Vein
- Option for Central Vein Stenosis
- Leg Access Indications:
- All Arm Options Exhausted
- Young Women (Avoid Scars)
- Paraplegics (Need Arms for Wheelchairs)
Arteriovenous Hemodialysis Access – Complications
Infection
- Most Common Complication
- Treatment:
- Autogenous AVF: ABX 2-4 Weeks
- Prosthetic Graft: Partial Graft Resection vs. Complete Excision
Access Failure
- Failure of Maturation
- Good Thrill but Unable to Cannulate
- Cause: Anastomotic Stricture or Too Deep
- Dx: US
- May Require Angioplasty or Revision
- Most Common Cause of Later Failure: Venous Outflow Stenosis
- From Intimal Hyperplasia/Stenosis at Graft-Venous Anastomosis
- Worsens with Time
Thrombosis
- Autogenous AVF:
- Thrombectomy Often Leads to Recurrent Thrombosis Due to Abnormal Underlying Surface & Trauma from Thromboembolectomy Catheter
- Percutaneous Thrombectomy May Have Better Results
- Prosthetic AV Graft:
- No Single Best Treatment
- Treatment:
- Early (< 30 Days): Surgical Thrombectomy
- Tolerates Balloon Thromboembolectomy Better Than Autogenous AVF
- Later (> 30 Days): Percutaneous Thrombectomy
- Early (< 30 Days): Surgical Thrombectomy
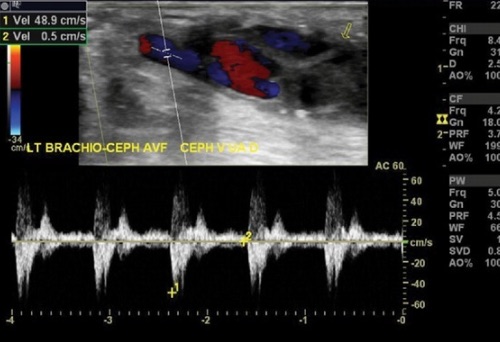
Fistula Thrombosis; To-and-From Waveform Indicating Outflow Obstruction 2
Access-Related Hand Ischemia (ARHI)/Steal Syndrome
- Ischemia Distal to Fistula
- Most Common in Proximal Fistulas
- Presentation: Pain, Numbness, Burning, Coolness & Weakness
- Diagnosis: Duplex US & Angiography
- Grade:
- Grade 0: No Symptoms
- Grade 1: Mild – Few Symptoms & Flow Augmentation with Occlusion
- Grade 2: Moderate – Claudication & Intermittent Pain Only During Dialysis
- Grade 3: Severe – Rest Pain & Tissue Loss
- Treatment:
- Mild: Exercise
- Moderate: May Require Surgical Intervention
- Severe: Surgical Intervention
- Surgical Procedures:
- DRIL Procedure (Distal Revascularization & Interval Ligation)
- Arterial Bypass Originating Proximal to the Fistula and Terminating Distal to the Fistula
- Ligate the Artery Just Distal to the Fistula Anastomosis
- Generally the Procedure of Choice
- RUDI Procedure (Revision Using Distal Inflow)
- Ligate Fistula at Arterial Anastomosis
- Reestablish Flow with Graft from a More Distal Arterial Site
- Banding
- Placing a Single Tie/Band Around the Fistula Near the Arterial Anastomosis
- Creates Stenosis & Therefore Decreases Flow
- Fistula Ligation
- Generally the Last Resort Only for Limb Salvage
- DRIL Procedure (Distal Revascularization & Interval Ligation)
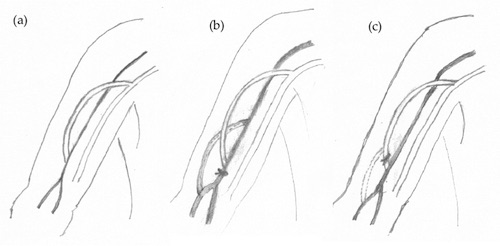
Steal Syndrome (a), DRIL Procedure (b), RUDI Procedure (c) 1
Ischemic Monomelic Neuropathy (IMN)
- Acute Shunting of Blood from Distal Nerve Fibers
- Can Potentially Cause Irreversible Damage
- Presentation: Severe Pain, Numbness, Paresthesias & Numbness
- Typically Immediately After Surgery
- Risk Factors: Diabetes, Atherosclerosis, Female & Proximal Access
- Treatment: Emergent Flow Augmentation or Fistula Ligation
Venous Hypertension
- Most Common Cause: Central Vein Stenosis – Mostly from Central Venous Catheters
- Stenosis Cannot Handle Sudden Increased Venous Return
- Can Be Seen in Superior Vena Cava Syndrome
- Presentation: Disabling Swelling & Distal Pain
- Can Risk Access Patency
- Diagnosis: Venography (Gold Standard) & Duplex US
- Treatment: Percutaneous Transluminal Angioplasty (PTA)
High-Output Cardiac Failure
- Fistula Creates a Left-to-Right Shunt
- Exaggeration of Normal Congestive Heart Failure
- Nicoladoni-Branham Sign: AVF Compression Causes Decreased HR & Increased BP
- From Increased Peripheral Vascular Resistance & Afterload
- Large Changes Seen with Compression
- Treatment: Ligation or Surgical Plication (Band Narrowing Just Beyond Arterial Anastomosis)
Aneurysm
- Aneurysm
- Requires Cessation of Cannulation Punctures
- First Step: Fistulogram to Rule Out High Outflow Resistance
- Treatment: Varies (Relocation, Partial Resection, Excision or Angioplasty)
- *See Vascular: Peripheral Aneurysm
- Pseudoaneurysm
- Mostly from Repeated Cannulation Punctures or Poor Technique
- Management: Change in Cannulation Technique & Site
- Intervention Based on Symptoms:
- *See Vascular: Peripheral Pseudoaneurysm
Bleeding
- Bleeding Can Be Rapid & Profuse
- The Most Common Cause is Repeated Trauma from Needle Cannulation During Dialysis
- Sites Should Be Rotated Each Session with Proper Technique to Avoid Risk
- Treatment:
- Initial Measure: Direct Pressure Can Control Most
- Consider Tourniquet if Needed
- Bleeding Often Stops After Pressure Held for 15-20 Minutes
- Options to Control Bleeding:
- Topical Agents (Thrombin/Surgicel/QuikClot)
- Suture Closure at Bedside
- Consider Correction of Coagulopathy if Needed
- Exploration in OR
- Can Consider Discharge if Hemodynamically Stable with Minimal Blood Loss
- Initial Measure: Direct Pressure Can Control Most
- Bedside Suture Closure:
- Assistant Should Place Pressure Above & Below to Slow Bleeding While Repairing
- Technique:
- Figure-of-Eight or Purse-String Fashion
- Generally Closing Skin is Sufficient – Scar Tissue from Repeated Access
- Suture Choice:
- Ideally Use a Non-Cutting Needle to Avoid Further Injury to Fistula
- 3-0 Nylon or 5-0 Prolene are Commonly Used
References
- Santoro D, Benedetto F, Mondello P, Pipitò N, Barillà D, Spinelli F, Ricciardi CA, Cernaro V, Buemi M. Vascular access for hemodialysis: current perspectives. Int J Nephrol Renovasc Dis. 2014 Jul 8;7:281-94.(License: CC BY-NC-3.0)
- Teodorescu V, Gustavson S, Schanzer H. Duplex ultrasound evaluation of hemodialysis access: a detailed protocol. Int J Nephrol. 2012;2012:508956. (License: CC BY-3.0)
- Elwakeel H, Elalfy K. Vascular Access for Hemodialysis – How to Maintain in Clinical Practice. Intech. 2013. (License: CC BY-3.0)