Breast: Breast Cancer Screening
Breast Examination
Self-Examination
- Done by the Patient
- NOT Recommended for Average Risk Women
- Increased Rate of Unnecessary Biopsy for Benign Disease
Clinical Breast Examination
- Done by Provider
- Routine Screening Exam Not Recommended for Average Risk Women
- Diagnostic Exam However Remains an Important Tool
Screening Mammogram
Basics
- Mammographic Screening Decreases Mortality by 25%
Normal Risk
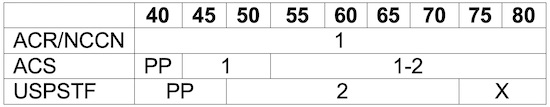
- National Comprehensive Cancer Network (NCCN)
- ≥ 40: Every Year
- American College of Radiology
- ≥ 40: Every Year
- American Cancer Society
- 40-44: Patient Preference
- 45-54: Every Year
- ≥ 55: Every 1-2 Years
- US Preventative Services Task Force (USPSTF)
- 40-49: Patient Preference
- 50-74: Every 2 Years
- ≥ 75: Insufficient Evidence
High-Risk (Lifetime > 20%)
- Family Hx
- Start: 10 Years Before Age of Dx in First Degree Relative
- BRCA Positive
- Yearly Breast MRI Starting at Age 25
- Start Earlier if a First-Degree Relative Diagnosed < Age 30
- Add Yearly Mammogram at Age 30
- Also Include Pelvic Exam, US & CA-125
- Yearly Breast MRI Starting at Age 25
Post Mastectomy
- Physical Exam:
- Every 6 Months for 5 Years
- Then Annually
- No Screening Imaging Needed
- Continue Routine Yearly Imaging for Contralateral Side if it Remains
Screening MRI
Indications for Annual MRI Screening
- High-Risk (Lifetime Risk > 20%)
- BRCA1 or BRCA2 Mutations
- First-Degree Relative with BRCA Mutation, But Patient Untested
- High-Risk Genetic Disease in Patient or a First-Degree Relative
- Li-Fraumeni, PTEN, Cowden or Bannayan-Riley-Ruvalcaba Syndromes
- Prior Chest Radiation Between Ages 10-30 Years
Insufficient Evidence – Decision Made on an Individual Basis
- Moderate-Risk (Lifetime Risk 15-20%)
- Personal History of Invasive Cancer
- Carcinoma In-Situ (LCIS/DCIS)
- Atypical Hyperplasia (ALH/ADH)
- Heterogenous or Extremely Dense Breast Tissue on Mammogram
Genetic Screening
Genes Tested
- BRCA1 & BRCA2
- PALB2
- PTEN
- TP53
- CDH1
Indications for Genetic Testing (NCCN Recommendations)
- Known Family History of High-Risk Mutations (BRCA, etc.)
- If Previously Tested Negative on a More Limited Test but Interested in Pursuing Multi-Gene Testing
- Personal History of Cancer:
- Breast Cancer:
- Diagnosed at Age ≤ 45 Years
- Diagnosed at Age 46-50 Years with:
- Unknown or Limited Family History
- A Second Breast Cancer at Any Age
- ≥ 1 Close Relative with Breast, Ovarian, Pancreatic or Prostate Cancer
- Diagnosed at Age ≤ 60 Years with Triple-Negative Breast Cancer
- Diagnosed at Any Age with:
- Ashkenazi Jewish Descent
- ≥ 1 One Close Relative with:
- Breast Cancer at Age ≤ 50
- Ovarian or Pancreatic Cancer at Any Age
- Metastatic, Intraductal/Cribriform Histology or High- or Very-High-Risk Group Prostate Cancer at Any Age
- ≥ 3 Total Diagnoses of Breast Cancer in the Patient and/or Close Relatives
- Male Breast Cancer at Any Age
- Epithelial Ovarian Cancer (Including Fallopian Tube or Peritoneal Cancers) at Any Age
- Exocrine Pancreatic Cancer at Any Age
- Prostate Cancer at Any Age with:
- Metastatic, Intraductal/Cribriform Histology or High- or Very-High-Risk Group
- Ashkenazi Jewish Descent
- ≥ 1 One Close Relative with:
- Breast Cancer at Age ≤ 50
- Ovarian or Pancreatic Cancer at Any Age
- Metastatic, Intraductal/Cribriform Histology or High- or Very-High-Risk Group Prostate Cancer at Any Age
- ≥ 2 Close Relatives with Either Breast or Prostate Cancer at Any Age
- A Mutation Identified on Tumor Genomic Testing that has Clinical Implication if Also Identified in the Germline
- If Meets Testing Criteria Otherwise for Li-Fraumeni Syndrome or Cowden/PTEN Hamartoma Tumor Syndrome
- To Aid in Systemic Therapy Decision-Making, Such as HER2-Negative Metastatic Breast Cancer
- Breast Cancer:
- Family History of Cancer:
- An Individual with a First- or Second-Degree Relative Meeting Any of the Above Criteria (Except Individuals Who Meet Criteria Only for Systemic Therapy Decision Making)
- If Affected Relative Has Pancreatic or Prostate Cancer, Only First-Degree Relatives Should Be Offered Testing Unless Indicated Otherwise
- An Individual Who Otherwise Does Not Meet Criteria Above but Has a Probability > 5% of BRCA1/2 Mutation Based on Prior Probability Models
- An Individual with a First- or Second-Degree Relative Meeting Any of the Above Criteria (Except Individuals Who Meet Criteria Only for Systemic Therapy Decision Making)
- *Close Relatives: First, Second or Third-Degree
Possible Indications to Consider – Decision Made on an Individual Basis
- Multiple Prior Breast Cancers, First Diagnosed Between Ages 50-65
- Ashkenazi Jewish Descent without Other Indications
- An Individual Who Otherwise Does Not Meet Criteria Above but Has a Probability 2.5-5% of BRCA1/2 Mutation Based on Prior Probability Models