Delivering Bad News
David Ray Velez, MD
The Operative Review of Surgery. 2023; 1:150-154.
Table of Contents
SUNBURN Protocol
Definition
- Framework for Delivering Bad News in Trauma and Acute Care Surgery
- Used to Guide Discussion with the Patient and/or Family Depending on the Circumstances
Steps 1
- S: Set Up – Review the Clinical History and Prepare for the Conversation
- U: Understand Perceptions – Appreciate What information is Already Known and Correct Any Misconceptions
- N: Notify (“Warning Shot”) – “I’m Afraid I Have Some Bad News”, Followed by a Pause to Sink In
- B: Brief Narrative and Break Bad News – Brief Narrative to Provide Context and then Deliver the News Directly
- U: Understand Emotions – Allow for Silence and Appreciate the Emotional Response
- R: Respond – Respond to Patient/Family Emotions with Empathy and Care
- N: Next Steps – Discuss the Next Steps or Strategy Going Forward
Unique Challenges in Trauma and Acute Care Surgery
- “SPIKES” and Other Protocols Poorly Correlate in Trauma 1
- No Previously Established Rapport
- Injury is Often Sudden Unexpected 2
- Events are Shrouded in Misconception 2
- Patients are Generally Younger 2
- Fewer Resources for Grief Support – Often Present on Nights and Weekends (Not Fully Staffed) 3,4
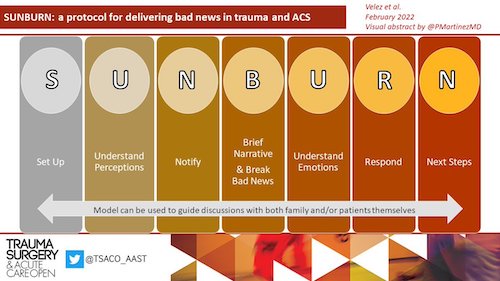
SUNBURN Visual Abstract 1
SPIKES Protocol
Definition
- Framework for Delivering Bad News
- Originally Designed for the Use in Oncology Patients at MD Anderson Cancer Center 2
- The Most Commonly Described Model in Medicine
Factors 5
- S: Setting – Set Up the Interview
- P: Perception – Assess the Patient/Family Perception
- I: Invitation – See What the Patient Wants to Know
- K: Knowledge – Share Knowledge
- E: Emotions – Respond to Patient/Family Emotions
- S: Strategy/Summary – Recap and Decide the Next Plan
Other Models
ABCDE Protocol 6
- Developed for Use in Primary Care
- Factors:
- A: Advanced Preparation – Review History and Prepare
- B: Build a Therapeutic Environment/Relationship – Ensure Adequate Time and Privacy in an Appropriate Setting
- C: Communicate Well – Avoid Medical Jargon and Allow for Silence
- D: Deal with Patient/Family Reactions – Actively Listen and Explore Empathy
- E: Encourage and Validate Emotions
BREAKS Protocol 7
- Developed for Oncology and Palliative Care in India
- Factors:
- B: Background – Review the Clinical History and Relevant Information Before Hand
- R: Rapport – Build Rapport and Allow Time to Understand Patient/Family Concerns
- E: Explore – Determine Patient/Family Understanding of Illness
- A: Announce – Give a “Warning Shot” and Deliver the News
- K: Kindle – Address Emotions as they Arise
- S: Summarize – Summarize the News and Patient Concerns
General Approach
Preparation
- Take a Moment to Compose Yourself
- Anticipate and Understand the Details Surrounding the Event and Clinical Course
- Mentally Prepare What You Will Say
- Bringing an Experienced Nurse Can Be Helpful
- Remove Any Blood-Stained Clothing
Setting
- Use a Quiet Room
- Have a Safety Strategy to Exit the Physical Space in the Case of a Violent Response
- Multiple Family Members Can Be Supportive but Avoid Excessively Large Groups
- Particularly in Pediatric Traumas – Larger Groups May Detract from the Ability to Provide Support to Parents
Delivery
- Sit Down – Do Not Stand by the Door
- Make Eye Contact and Look at Who You are Addressing
- Understand What Information They Already Know to Correct Any Misconceptions
- Begin with a “Warning Shot”
- “I’m Afraid I Have Some Bad News”
- “I Am So Sorry…”
- Be Honest and Direct, Do Not Beat Around the Bush
- Give a Brief Narrative for Context and Then Deliver the News
- If Patient Has Died, Use the Words “Death” or “Dead” and Avoid Euphemisms (“Passed Away”)
- Avoid Excessively Long Drawn Out Narratives that Delay Delivery – There is No Way to Soften the Impact
- Avoid Excessive Technical Information or Unnecessarily Gruesome Details
- Do Not Rush
After
- Allow Silence for Facts to Sink In
- Allow for the Bereaved to React to the News – Varied Reactions May Be Seen
- Provide Tissues
- Touching/Holding a Hand to Comfort is Generally Appropriate but Should Be Considered in Various Social/Cultural Settings
- Avoid Platitudes or False Sympathy
- “You Have Another Son”
- “I Know What it is Like”
- Do Not Concentrate on Yourself
- “I Have a Child Too”
- “You Know, This Isn’t Easy for Me”
- Provide an Opportunity for Family to See the Patient – Even if Injuries are Mutilating, Although Cover Wounds as Able
Debrief with the Medical Team
- “Second Victims” – Traumatic and Adverse Events Can Cause Significant Psychological Distress to the Physicians and Medical Team Providing Care as Well 8
- Consider a Debrief with the Medical Team to Ensure the Emotional Stability of the Staff
- Discussions Should be Led by the Team Leader/Physician as Close to the End of an Event as Possible 9
- Primary Goals of the Discussion: 9,10
- Review What Happened
- Analyze the Team Functioning and Evaluate for Necessary Changes/Improvements
- Create a Feeling of Professional Capability, Resilience, and Trust
- Enable Expression of Feelings
- Screening of Team Members for Acute Stress Reactions
Most Important Factors in Trauma (From the Perspective of Family) 11
- Most Important:
- Attitude of the News-Giver (72% Consider Important)
- Clarity of the Message (70%)
- Privacy (65%)
- Knowledge/Ability to Answer Questions (57%)
- Intermediate Importance:
- Sympathy
- Time for Questions
- Location of the Conversation
- Least Important:
- Attire of the News-Giver (3%)
References
- Velez D, Geberding A, Ahmeti M. SUNBURN: a protocol for delivering bad news in trauma and acute care surgery. Trauma Surg Acute Care Open. 2022 Feb 9;7(1):e000851. (License: CC BY-NC 4.0)
- McLauchlan CA. ABC of major trauma. handling distressed relatives and breaking bad news. BMJ1990;301:1145–9.
- Kieffer WKM, Michalik DV, Gallagher K, McFadyen I, Bernard J, Rogers BA. Temporal variation in major trauma admissions. Ann R Coll Surg Engl2016;98:128–37.
- Smith SA, Yamamoto JM, Roberts DJ, Tang KL, Ronksley PE, Dixon E, Buie WD, James MT, Care WS. Weekend surgical care and postoperative mortality: a systematic review and meta-analysis of cohort studies. Med Care2018;56:121–9.
- Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES-A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist2000;5:302–11.
- VandeKieft GK. Breaking bad news. Am Fam Physician2001;64:1975–8.
- Narayanan V, Bista B, Koshy C. ‘BREAKS’ protocol for breaking bad news. Indian J Palliat Care2010;16:61–5.
- Seys D, Wu AW, Van Gerven E, Vleugels A, Euwema M, Panella M, Scott SD, Conway J, Sermeus W, Vanhaecht K. Health care professionals as second victims after adverse events: a systematic review. Eval Health Prof2013;36:135–62.
- Missouridou E. Secondary posttraumatic stress and nurses’ emotional responses to patient’s trauma. J Trauma Nurs2017;24:110–5.
- Knobler HY, Nachshoni T, Jaffe E, Peretz G, Yehuda YB. Psychological guidelines for a medical team Debriefing after a stressful event. Mil Med2007;172:581–5.
- Jurkovich GJ, Pierce B, Pananen L, Rivara FP. Giving bad news: the family perspective. J Trauma2000;48:865–73.