Large Intestine: Diverticulitis
Diverticulitis
Basics
- Incidence in Diverticulosis: 4-15%
- Most Common Source: Left Colon
- Cause: Perforation (Microscopic or Macroscopic) by Erosion from Increased Intraluminal Pressure
- Tic Obstruction (Fecalith) & Venous Congestion May Contribute but Now Thought to be Rarer than Previously Thought
- May be Associated with Colorectal Cancer
Features of Complicated Diverticulitis
- Hemorrhage
- Obstruction
- Stricture
- Free Perforation
- Fistula
- Abscess
- Purulent or Feculent Peritonitis
- Unable to Exclude CA
Presentation
- Abdominal Pain (Classically Constant in LLQ)
- Fever
- Nausea & Vomiting
- Constipation or Diarrhea
- Urinary Urgency or Frequency
Diagnosis
- Dx: CT
- Can Be Made Clinically with Classic Presentation & History of Diverticulitis
Diverticulitis 1
Classification
Hinchey Classification
- I: Pericolic Abscess or Phlegmon
- II: Distant Abscess (Intraabdominal/Pelvic/Retroperitoneal)
- III: Purulent Peritonitis
- IV: Feculent Peritonitis
Modified Hinchey Classification by Sher
- I: Pericolic Abscess
- II: Distant Abscess (Pelvis/Retroperitoneal/Intra-Abdominal)
- IIa: Amenable to Percutaneous Drainage
- IIb: Not Amenable to Percutaneous Drainage
- III: Purulent Peritonitis
- IV: Feculent Peritonitis
Modified Hinchey Classification by Wasvary
- 0: Mild Clinical Diverticulitis
- I: Pericolic Abscess or Phlegmon
- Ia: Confined Phlegmon
- Ib: Pericolic Abscess
- II: Distant Abscess (Pelvis/Retroperitoneal/Intra-Abdominal)
- III: Purulent Peritonitis
- IV: Feculent Peritonitis
Other Classification Systems
- Hughes Classification
- Kohler Classification
- Hansen/Stock Classification
- Siewert Classification
- Ambrosetti Classification
Modified Hinchey Class 0 2

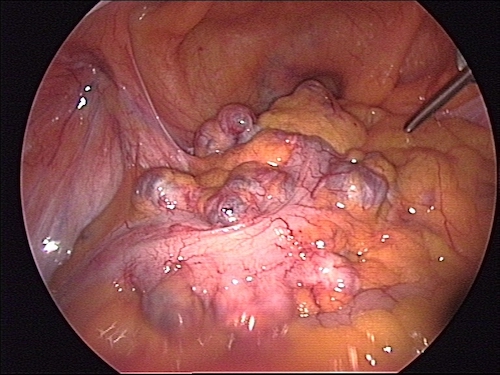
Diverticulitis Hinchey Class I 3
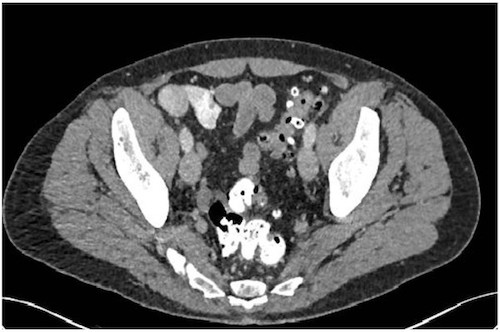
Diverticulitis Hinchey Class II 2

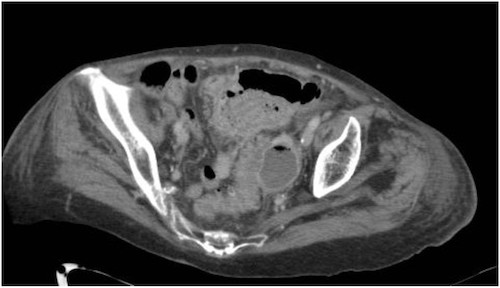
Diverticulitis Hinchey Class III/IV 4
Treatment
Treatment
- Uncomplicated (Class 0/Ia): Conservative Management
- Consider:
- Bowel Rest with IV Fluid Resuscitation vs Oral Hydration
- ABX (IV vs Oral) vs None (Controversial)
- Repeat CT if No Clinical Improvement After 5-7 Days
- Consider:
- Complicated by Abscess (Class Ib/II)
- < 3-4 cm: IV ABX
- Repeat CT if No Clinical Improvement After 5-7 Days
- > 3-4 cm: IV ABX & Percutaneous Drain
- If Fails or Unable to Access: Laparoscopic Drain
- < 3-4 cm: IV ABX
- Unstable, Peritonitis or Free Perforation (Class III/IV): Surgical Sigmoidectomy
Surgical Management
- Surgical Options:
- Two-Stage Procedures
- Hartmann’s Procedure with End Colostomy – Traditional Gold Standard
- Over Half Never Return to the OR for Ostomy Reversal
- Primary Anastomosis & Diverting Loop Ileostomy
- Similar Morbidity & Mortality
- Better Rates of Stoma Reversal
- Hartmann’s Procedure with End Colostomy – Traditional Gold Standard
- One-Stage Procedure
- Sigmoid Colectomy & Primary Anastomosis without Ostomy
- May Consider if Stable with Good Nutrition & Minimal Peritonitis
- Two-Stage Procedures
- Rarely Performed Options:
- Three-Stage Procedure
- Proximal Diverting Colostomy
- Sigmoidectomy
- Colostomy Takedown
- Now Largely Replaced by Two-Stage Procedures
- Laparoscopic Lavage without Resection
- Generally Not Advised – 3x Increased Risk for Further Invasive Procedures
- May Consider if No Diffuse Peritonitis with a Contained Abscess or Inflammation Too Severe for a Safe Colectomy
- Three-Stage Procedure
Post-Diverticulitis Management if Managed Nonoperatively
- Follow Up Colonoscopy in 6-8 Weeks (Evaluate Risk for Cancer)
- Consider Elective Colectomy
- Stronger Recommendation After an Episode of Complicated Diverticulitis than Uncomplicated Diverticulitis
- Statistically Most Likely to Have a Complication with the First Episode than with Later Episodes
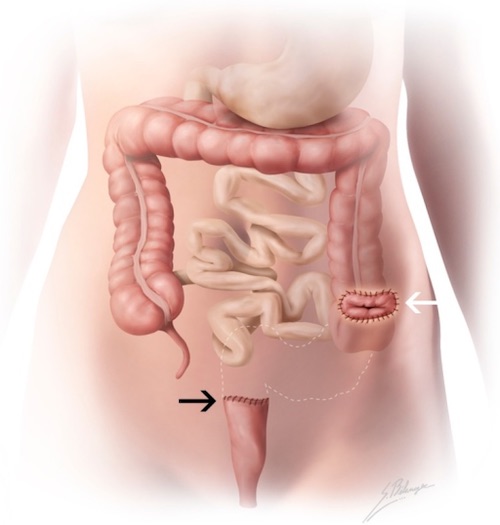
Hartmann Procedure 5
References
- Anpol42. Wikimedia Commons. (License: CC BY-SA-4.0)
- Sartelli M, Moore FA, Ansaloni L, et al. A proposal for a CT driven classification of left colon acute diverticulitis. World J Emerg Surg. 2015 Feb 19;10:3. (License: CC BY-4.0)
- Heilman J. Wikimedia Commons. (License: CC BY-SA-3.0)
- Naves AA, D’Ippolito G, Souza LRMF, Borges SP, Fernandes GM. What radiologists should know about tomographic evaluation of acute diverticulitis of the colon. Radiol Bras. 2017 Mar-Apr;50(2):126-131. (License: CC BY-4.0)
- Terrone DG, Lepanto L, Billiard JS, Olivié D, Murphy-Lavallée J, Vandenbroucke F, Tang A. A primer to common major gastrointestinal post-surgical anatomy on CT-a pictorial review. Insights Imaging. 2011 Dec;2(6):631-638. (License: CC BY-2.0)