Duodenal Trauma
Scott Williams, MD
The Operative Review of Surgery. 2023; 1:11-16.
Table of Contents
General Information
General
- Difficult Due to Complex Anatomical & Physiologic Relationships 1
- Delay in Diagnosis is a Significant Factor in Morbidity & Mortality
- Mortality Risk 4x if Diagnosis Delayed by Over 24-Hours 2
- Morbidity Rate: 22-27% 1
- Mortality Rate: 5-30% 1
- Grade I: 8.3%
- Grade II: 18.7%
- Grade III: 27.6%
- Grade IV: 30.8%
- Grade V: 58.8%
Etiology
- Rare: Only 3.7-5% of All Abdominal Injuries 3
- Penetrating Trauma Most Common (77.7%) 4
- 81% Gunshot Wounds 1
- 19% Stab Wounds 1
- Blunt Trauma (22.3%) 4
- 85% Motor Vehicle Collisions 1
- Other Blunt Causes: Assault & Falls
Mechanism of Injury
- Penetrating Mechanisms:
- Direct Injury
- Cavitation
- Shock Wave
- Blunt Mechanisms:
- Crushing Force
- Shearing Force
- Bursting Force
- *See Approach to Abdominal Trauma
Location of Injury 1
- First Portion: 13%
- Second Portion: 36% – Most Common
- Third Portion: 18%
- Fourth Portion: 15%
- *18% Affect Multiple Portions

Duodenal D1 Transection 5
Presentation & Diagnosis
Presentation 6
- Mostly Nonspecific
- Abdominal Pain, Can Radiate to the Back
- Chest Pain
- Nausea & Vomiting
- Hematemesis
- Rarely Associated with Severe Testicular Pain & Priapism I
- Due to Sympathetic Stimulation Along the Gonadal Vessels
Diagnosis
- Difficult Due to Complex Anatomical & Physiologic Relationships 1
- Requires a High Index of Suspicion
- Stable Patients May Be Diagnosed on CT
- May Be Diagnosed Intraoperatively
AAST Duodenum Injury Scale
- *See AAST
- Injury Scale is Under Copyright
Associated Injuries 1
- Liver (17%)
- Colon (13%)
- Pancreas (12%)
- Other Small Bowel (11%)
- Stomach (9%)
- *Rarely Occurs in Isolation
Complications 6
- Duodenal Leak/Fistula – Major Source of Morbidity
- Initial Treatment: Conservative (NPO/NGT/TPN) & Octreotide
- Missed Injury
- Intraabdominal Abscess
- Duodenal Obstruction
- Recurrent Pancreatitis
- Bleeding
Treatment
Surgical Access
- Kocher Maneuver: Access D1, D2 & Proximal D3
- Cattel-Braasch Maneuver: Access Entire Duodenum (Including Distal D3 & D4)
Primary Repair
- Primary Repair is Generally the Preferred Treatment for Most Duodenal Injuries 7
- Successful for 70-85% of Injuries (Even with Full Transection) 8
- Requires: Little Tissue Loss with No Tension & No Involvement of the Ampulla
- Considerations:
- Nasogastric Tube to Protect Repair
- Extraluminal Drain – Use is Debated with No Level I Evidence
- Possible Increased Risk for Duodenal Leak 6
- Severe or Concurrent Pancreatic Injury: Pyloric Exclusion with Gastrojejunostomy 9
- Pyloric Exclusion (PEX) – Gastrotomy & Closure of the Pylorus Using Absorbable Suture (Vicryl or PDS) 11
- After 4-12 Weeks Gastrojejunostomy Closes and Pylorus Reopens
- Risk for Marginal Ulcer (Some Add Truncal Vagotomy, Most Manage Medically)
If Primary Repair Not Feasible
- Under Tension or Involves Ampulla: Roux-en-Y Duodenojejunostomy (DJ) 12
- Jejunal Limb Anastomosis to the Proximal Duodenum & Oversewing of Distal Duodenum
- Massive Injury Involving Head of Pancreas: Pancreaticoduodenectomy (Whipple Procedure) 13
- Never Done in an Emergent Setting
- Requires Wide Drainage at Index Operation & Definitive Repair Upon Medical Stabilization
Historical Options Fallen Out of Favor
- Jejunal Serosal Patch 14
- Less Desirable than Roux-en-Y
- Retrograde Jejunostomy
- For Duodenal Decompression
- Duodenal Diverticularization 15
- Procedure: Primary Repair, Antrectomy & Gastrojejunostomy
- Creates a Permanent Bypass of the Repair
- May Add Tube Duodenostomy for Decompression
- Triple-Ostomy Repair 16
- Procedure: Gastrostomy, Duodenostomy (Or Retrograde Jejunostomy) & Feeding Jejunostomy
- Triple-Tube Repair 16
- Procedure: Primary Repair with NG Tube, Feeding Jejunostomy & Retrograde Jejunostomy
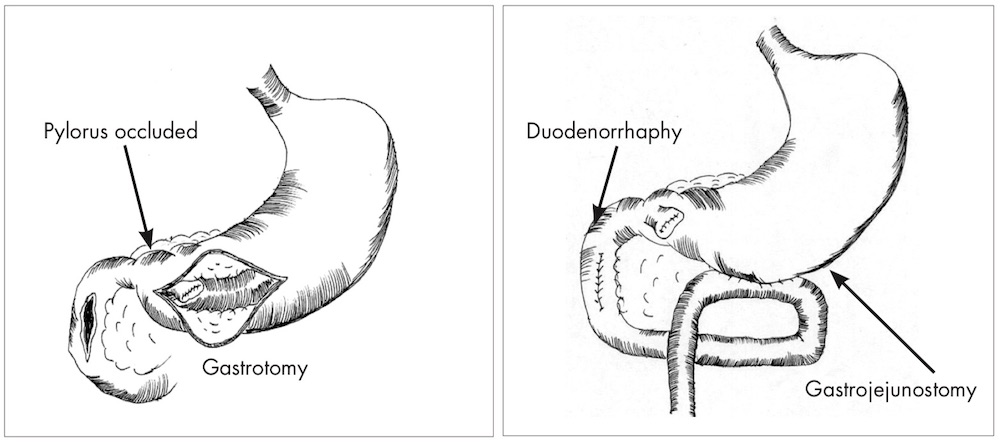
Pyloric Exclusion 10
Paraduodenal Hematoma
Causes
- Most Common in Peds After Play (Bicycle Handlebars or Sports) or Abuse 18
- Can Be Spontaneous Due to Hemophilia
- May Be Associated with Anticoagulation in Older Patients 19
- *Duodenum is the Most Common Site of Intramural Hematoma Among the GI Tract (27.5%) 20
Presentation 19
- Mostly Nonspecific
- Primary Concern is Progression Causing Luminal Obstruction
- Abdominal Pain
- Nausea & Vomiting
- Hematemesis
- Ampullary Obstruction Can Cause Cholestasis or Pancreatitis 21-23
Diagnosis
- Often Difficult to Diagnose & Requires a High Index of Suspicion
- Primarily Diagnosed by CT or UGI 19
- May Also Be Seen on MRI
- US Often Used in Peds to Avoid Radiation 19
- “Stacked Coins” or “Coiled Spring” Sign on UGI – Due to Partial Intussusception of the Bowel Wall Distal to the Hematoma 24
Treatment (If Found on Imaging)
- Conservative Treatment (NPO & Serial Exams)
- Most (60-85%) Improve Within a Short Period (2-3 Weeks) 19
- Complete Resolution of Symptoms Often Takes Months (Average 13 Months) 19
- If Obstructs: NGT, TPN, & UGI Every 5-7 Days
- If Persists > 2-3 Weeks: Operative Evacuation 17
Treatment (If Found Intraoperatively)
- Mostly Conservative Treatment
- Kocher & Thoroughly Inspect for Perforation
- Indications for Hematoma Evacuation: 6
- High Suspicion for Full-Thickness Injury
- > 50% Luminal Narrowing

Duodenal Hematoma 17
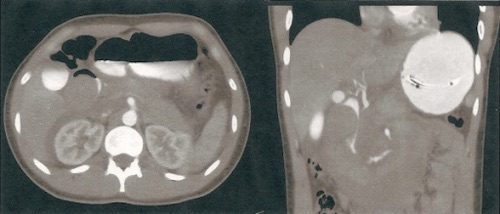
Duodenal Hematoma 17
References
- García Santos E, Soto Sánchez A, Verde JM, Marini CP, Asensio JA, Petrone P. Duodenal injuries due to trauma: Review of the literature. Cir Esp. 2015 Feb;93(2):68-74.
- Lucas CE, Ledgerwood AM. Factors influencing outcome after blunt duodenal injury. J Trauma. 1975 Oct;15(10):839-46.
- Malhotra A, Biffl WL, Moore EE, Schreiber M, Albrecht RA, Cohen M, Croce M, Karmy-Jones R, Namias N, Rowell S, Shatz DV, Brasel KJ. Western Trauma Association Critical Decisions in Trauma: Diagnosis and management of duodenal injuries. Journal of Trauma and Acute Care Surgery. 2015;79(6):1096-1101.
- Poyrazoglu Y, Duman K, Harlak A. Review of pancreaticoduodenal trauma with a case report. Indian Journal of Surgery. 2016;78(3):209-213.
- Smiley K, Wright T, Skinner S, Iocono JA, Draus JM. Primary Closure without Diversion in Management of Operative Blunt Duodenal Trauma in Children. ISRN Pediatr. 2012;2012:298753. (License: CC BY-3.0)
- Velez DR, Briggs S. Duodenal Trauma. StatPearls. 2022 Aug.
- Feliciano DV, Mattok KL, Moore EE. Trauma, 9e. 2020. McGraw Hill.
- Fraga GP, Biazotto G, Bortoto JB, Andreollo NA, Mantovani M. The use of pyloric exclusion for treating duodenal trauma: case series. Sao Paulo Med J. 2008 Nov;126(6):337-41.
- Degiannis E, Krawczykowski D, Velmahos GC, Levy RD, Souter I, Saadia R. Pyloric exclusion in severe penetrating injuries of the duodenum. World J Surg. 1993 Nov-Dec;17(6):751-4.
- Pierro AC, Mantovani M, Reis NS, Morandin RC, Fraga GP. Tratamento do trauma duodenal complexo: comparação entre sutura simples e sutura associada à exclusão pilórica e gastrojejunostomia em cães. Acta Cir Bras. [serial online] 2005 Jan- Fev;20(1). (License: CC BY-4.0)
- DeSantis M, Devereux DF, Thompson D. Pyloric exclusion. Suture material of choice. Am Surg. 1987 Dec;53(12):711-4.
- Diggs LP, Gregory S, Choron RL. Review of Traumatic Duodenal Injuries: Etiology, Diagnosis, and Management. Am Surg. 2022 Jan 2:31348211065091.
- THAL AP, WILSON RF. A PATTERN OF SEVERE BLUNT TRAUMA TO THE REGION OF THE PANCREAS. Surg Gynecol Obstet. 1964 Oct;119:773-8.
- Ivatury RR, Gaudino J, Ascer E, Nallathambi M, Ramirez-Schon G, Stahl WM. Treatment of penetrating duodenal injuries: primary repair vs. repair with decompressive enterostomy/serosal patch. J Trauma. 1985 Apr;25(4):337-41.
- Donovan AJ, Hagen WE. Traumatic perforation of the duodenum. Am J Surg. 1966 Mar;111(3):341-50.
- Stone HH, Fabian TC. Management of duodenal wounds. J Trauma. 1979 May;19(5):334-9.
- Nolan GJ, Bendinelli C, Gani J. Laparoscopic drainage of an intramural duodenal haematoma: a novel technique and review of the literature. World J Emerg Surg. 2011 Dec 20;6(1):42. (License: CC BY-2.0)
- Clendenon JN, Meyers RL, Nance ML, Scaife ER. Management of duodenal injuries in children. J Pediatr Surg. 2004 Jun;39(6):964-8.
- Niehues SM, Denecke T, Bassir C, Hamm B, Haas M. Intramural duodenal hematoma: clinical course and imaging findings. Acta Radiol Open. 2019 Apr 8;8(4):2058460119836256.
- Veldt BJ, Haringsma J, Florijn KW, et al.Coumarin-induced intramural hematoma of the duodenum: case report and review of the literature.Scand J Gastroenterol2011; 46:376–379.
- Abbas MA, Collins JM, Olden KW.Spontaneous intramural small-bowel hematoma: imaging findings and outcome.Am J Roentgenol2002; 179:1389–1394.
- Sadry F, Hauser H. Fatal pancreatitis secondary to iatrogenic intramural duodenal hematoma: a case report and review of the literature.Gastrointest Radiol1990; 15:296–298.
- van Spreeuwel JP, van Gorp LH, Bast TJ, et al. Intramural hematoma of the duodenum in a patient with chronic pancreatitis.Endoscopy1981; 13:246–248.
- Jones WR, Hardin WJ, Davis JT, et al.Intramural hematoma of the duodenum: a review of the literature and case report.Ann Surg1971;173:534–544.