Fascial Closure
Fascial Closure
Rachel Deborah Miller, MD
Table of Contents
Laparotomy Incision Closure
Optimal Technique
- Continuous/Running Suture
- Small Bites (5-7 mm Every 5-7 mm) – Largely Based on the STITCH Trial
- Goal Suture:Wound Length: 4:1
Suture Selection
- Slowly Absorbable Monofilament Suture is Generally Preferred
- 2-0 PDS Was Used in the Classic STITCH Trial
- Barbed Suture (Stratafix, V-Loc) May Decrease the Risk of Fascial Dehiscence and Evisceration
- Triclosan-Coated Suture (Stratafix Symmetric, PDS Plus) May Decrease the Rates of Surgical Site Infections
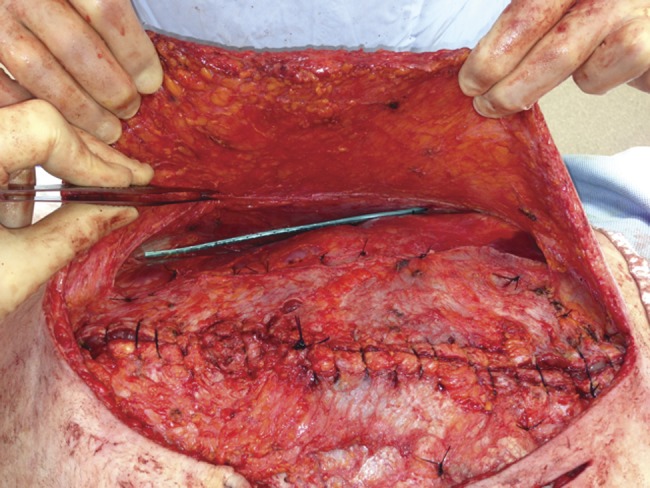
Prophylactic Mesh Placement
- May Decrease the Risk of Hernia
- Onlay or Retro-Muscular Plane is Preferred
- Complications:
- Increased Risk of Seroma
- No Increased Risk of Infection
- *Use is Debated and Not Clearly Defined
Abdominal Binders
- No Evidence to Show Decreased Risk of Incisional Hernia or Burst Abdomen
- May Decrease Postoperative Pain
Fascial Closure 1
Port-Site Closure
Indications to Close the Fascial Defect
- Trocar Sites ≥ 10 mm
- Any Size After Single-Incision Laparoscopic Surgery (SILS)
- Any Size at the Umbilical Site
Technique for Port-Site Closure
- Over 20+ Techniques Have Been Described but There are Three General Groups
- Intracorporeal Assistance – Require 2 Additional Ports (One to Visualize and One to Manipulate)
- Maciol Needles
- Grice Needles
- Endoclose Suture Device
- Extracorporeal Assistance – Require One Additional Port to Visualize
- Carter-Thomason CloseSure System
- Endo-Judge Wound Closure Device
- Tahoe Surgical Instrument Ligature Device
- External Closure – No Additional Ports Required
- Suture Carrier
- Dual-Hemostat Technique
- Standard Hand Suture Closure
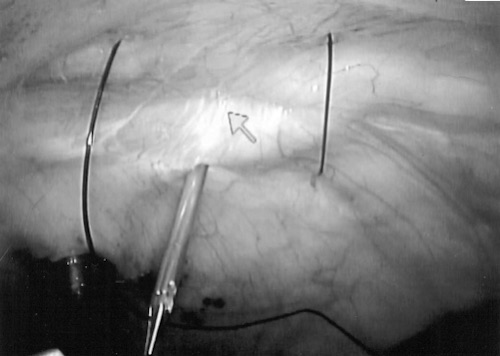
Carter-Thomason Device 2
References
- Rawstorne E, Smart CJ, Fallis SA, Suggett N. Component separation in abdominal trauma. J Surg Case Rep. 2014 Jan 20;2014(1):rjt133. (License: CC BY-NC-3.0)
- Eid GM, Thodiyil PA, Collins J, Bonanomi G, Mattar SG, Hughes SJ, Schauer PR, Wilson M. Laparoscopic repair of umbilical hernias in conjunction with other laparoscopic procedures. JSLS. 2006 Jan-Mar;10(1):63-5. (License: CC BY-NC-ND-3.0)