Abdominal Compartment Syndrome (ACS)
David Ray Velez, MD
The Operative Review of Surgery. 2023; 1:142-149.
Table of Contents
Definitions
Definition 1
- Intraabdominal Pressure (IAP): Steady-State Pressure Concealed within the Abdominal Cavity
- Abdominal Perfusion Pressure (APP) = MAP – IAP
- Normal IAP: 5-7 mmHg in Critically Ill Adults
- Intraabdominal Hypertension (IAH): Sustained IAP ≥ 12 mmHg
- Abdominal Compartment Syndrome (ACS): Sustained IAP > 20 mmHg that is Associated with New Organ Dysfunction/Failure
- Primary ACS: ACS that Originates from Injury or Disease in the Abdominopelvic Region
- Secondary ACS: ACS that Originates from Injury or Disease Outside of the Abdominopelvic Region
- Recurrent ACS: ACS that Recurs After a Previously Treated ACS
- Polycompartment Syndrome: Two or More Anatomical Compartments Have Elevated Compartmental Pressures
- Compartments Include Abdomen, Thorax, Head, and Extremities 2
- The Compliance of Each Compartment is Key to Determining the Transmission of Pressure Between Compartments 2
Chronic Elevation
- IAP May Be Chronically Higher in Those with Ascites, Pregnant, or Obese (7-14 mmHg) 3,4
- Acute Increases in IAP May Be Less Well Tolerated if Superimposed on Chronic IAH 5
Intraabdominal Hypertension Grading 1
- Grade I: IAP 12-15 mmHg
- Grade II: IAP 16-20 mmHg
- Grade III: IAP 21-25 mmHg
- Grade IV: IAP > 25 mmHg
Pediatric Changes 1
- Intraabdominal Hypertension: Sustained IAP > 10 mmHg
- Abdominal Compartment Syndrome: Sustained IAP > 10 mmHg that is Associated with New Organ Dysfunction/Failure
Pathophysiology
Pulmonary Effects 6,7
- Intraabdominal Hypertension Causes Upward Displacement of the Diaphragm
- Upward Displacement of the Diaphragm Causes:
- Increased Intrathoracic Pressure
- Decreased Chest Wall Compliance
- Decreased Functional Residual Capacity (FRC)
- Increased Pulmonary Vascular Resistance
- Compression Atelectasis
- Increased Intrathoracic Pressure Causes:
- Increased Pleural Pressure
- Increased Airway Pressures (Peak, Mean, and Plateau)
- Effects on Gas Exchange:
- Hypercarbia and Hypoxia
- Increased Ventilation-Perfusion Mismatch with Dead-Space Ventilation and Intrapulmonary Shunting
Cardiovascular Effects 6-8
- Intraabdominal Hypertension Causes Increased Intrathoracic Pressure
- Increased Intrathoracic Pressure Causes:
- Decreased Preload Due to Increased Central Venous Pressure (CVP) and Pulmonary Artery Pressure (PAP)
- Increased Left Ventricle Afterload Due to Vascular Resistance
- Increased Right Ventricle Afterload Can Cause Septal Deviation to the Left, Further Decreasing Preload
- Results in Decreased Cardiac Output and High Peripheral Vascular Resistance
Renal Effects 6,9
- Intraabdominal Hypertension Causes:
- Poor Renal Perfusion Due to Decreased Cardiac Output
- Renal Venous Resistance
- Direct Renal Compression with Shunting of Blood from the Cortex to the Medulla
- Activation of the RAAS System Leading to Water and Sodium Retention
- Results in Renal Impairment and Oliguria/Anuria
- *First Clinical Sign of Intraabdominal Hypertension
Gastrointestinal Effects 6-8
- Intraabdominal Hypertension Causes:
- Decreased Cardiac Output
- Increased Splanchnic Vascular Resistance
- Results in Poor Mesenteric Blood Flow
- Risk for Mucosal Ischemia and Perforation
Hepatic Effects 7,8
- Intraabdominal Hypertension Causes:
- Decreased Cardiac Output
- Increased Splanchnic Vascular Resistance
- Results in Decreased Hepatic Artery and Portal Vein Blood Flow
- Results in Decreased Liver Function and Lactate Clearance
Central Nervous System Effects 6,7
- Intraabdominal Hypertension Causes Increased Intrathoracic Pressure
- Increased Intrathoracic Pressure Causes Increased Jugular Venous Pressure and Impairs Cerebral Venous Return
- Results in Increased Intracranial Pressure (ICP) and Decreased Brain Perfusion
Extremity Effects 6
- Intraabdominal Hypertension Causes:
- Increased Central Venous Pressure
- Increased Peripheral Vascular Resistance
- Decreased Cardiac Output
- Results in Decreased Peripheral Perfusion of the Extremities
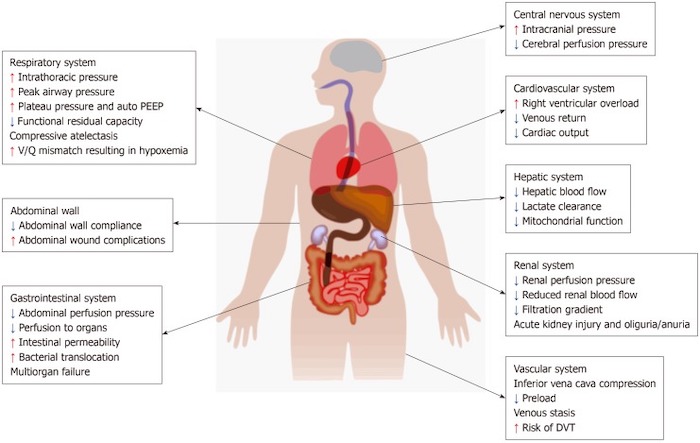
Effects of Abdominal Compartment Syndrome 7
Risk Factors
Reduced Abdominal Wall Compliance 7,10
- Obesity
- Abdominal Surgery
- Prone Positioning
- Rectus Sheath Hematoma
- Burns with Abdominal Eschar
- Mechanical Ventilation with High PEEP
- Ventilator Dyssynchrony
Increased Intraluminal Contents 7,10
- Gastric Distention
- Gastroparesis
- Ileus
- Small Bowel Obstruction
- Colonic Pseudo-Obstruction
- Volvulus
- Intraabdominal Tumor
- Retroperitoneal Tumor
- Damage Control Laparotomy
- Enteral Feeding
- Pregnancy
Abdominal Cavity Collections 7,10
- Ascites
- Hemoperitoneum
- Pneumoperitoneum
- Major Trauma
- Laparoscopy with Excessive Inflation Pressures
- Peritoneal Dialysis
- Abdominal Inflammation-Peritonitis (Pancreatitis)
- Abdominal Abscess
Capillary Leak and Fluid Resuscitation 7,10
- Acidosis
- Hypothermia
- Coagulopathy
- Massive Transfusion
- Trauma
- Sepsis
- Large Volume Fluid Resuscitation
- Major Burns
- Liver Transplant
Presentation
Symptoms 11
- Most Patients are Critically Ill and Unable to Communicate
- Fatigue and Malaise
- Dyspnea
- Lightheadedness
- Abdominal Pain
- Abdominal Distention
Physical Exam
- Tense and Distended Abdomen
- Abdominal Exam is a Poor Predictor of ACS 12-14
Additional Findings 6-9
- Pulmonary:
- Increased Airway Pressures
- Hypercarbia and Hypoxia
- Difficulty Weaning from the Ventilator
- Cardiovascular:
- Decreased Cardiac Output
- Increased Peripheral Vascular Resistance
- Renal Injury and Oliguria/Anuria
- Intestinal Ischemia and Perforation
- Elevated Intracranial Pressure (ICP)
Diagnosis
Diagnosis
- Definitive Diagnosis is Made by the Measurement of Intraabdominal Pressure (IAP) in the Setting of New Organ Dysfunction/Failure 1
- Requires IAP > 20 mmHg
- Perform with a Low Threshed of Suspicion 15
Measurement of IAP 16
- Intravesical (Bladder Pressure) – Standard Method
- Intragastric
- Intracolonic
- IVC Catheters
Requirements for Accurate Measurement 1
- Measured at End-Expiration
- Measured in the Supine Position
- Ensure that Abdominal Muscle Contractions are Absent (Sedation)
- Transducer Should be Zeroed at the Midaxillary Line
How to Measure Bladder Pressure (Procedure) 17
- Place Foley Catheter and Drain the Bladder
- Clamp Foley Catheter
- Zero Transducer at the Midaxillary Line
- Instill Sterile Saline into the Bladder (Maximum 25 cc) 1
- Insert an 18 Gauge Needle Attached to a Pressure Transducer into the Aspiration Port
- Some Commercially Available Catheters Permit Measurement by a Needle-Less Connection System
- Measure the Pressure at End-Expiration
- Wait for 60 Seconds After Instillation of Fluid to Allow Detrusor Muscle Relaxation
Treatment
Definitive Treatment
- Definitive Treatment is by Decompressive Laparotomy with Temporary Abdominal Closure 1
- Immediate Complications of Decompression:
- Bolus of Lactic Acid, Potassium and Other Anaerobic Byproducts (Induced Arrhythmia)
- Decrease in Preload (Induced Hypotension)
- Respiratory Alkalosis
- May Be Able to Avoid Laparotomy in Select Cases:
- Massive Ascites – Percutaneous Catheter Decompression/Paracentesis 18
- Burn Eschars Causing Mechanical Limitations – Escharotomy 19
Options to Temporize or Prevent Progression of IAH to ACS 20
- Place in the Supine Position and Avoid Elevating the Head of Bed
- Improve Abdominal Wall Compliance:
- Sedation and Analgesia
- Paralysis
- Reduce Intraabdominal Volume:
- Orogastric/Nasogastric Tube Decompression
- Foley Catheter
- Percutaneous Catheter Decompression/Paracentesis
- Low Tidal Volume & High PEEP
- Limit Fluid Administration
Morbidity and Mortality
- Failure to Recognize Can Cause Multisystem Organ Failure and Death
- High Mortality Once ACS Develops (40-100%) 21-25
References
- Kirkpatrick AW, Roberts DJ, De Waele J, Jaeschke R, Malbrain ML, De Keulenaer B, Duchesne J, Bjorck M, Leppaniemi A, Ejike JC, Sugrue M, Cheatham M, Ivatury R, Ball CG, Reintam Blaser A, Regli A, Balogh ZJ, D’Amours S, Debergh D, Kaplan M, Kimball E, Olvera C; Pediatric Guidelines Sub-Committee for the World Society of the Abdominal Compartment Syndrome. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med. 2013 Jul;39(7):1190-206.
- Malbrain ML, Roberts DJ, Sugrue M, De Keulenaer BL, Ivatury R, Pelosi P, Verbrugge F, Wise R, Mullens W. The polycompartment syndrome: a concise state-of-the-art review. Anaesthesiol Intensive Ther. 2014 Nov-Dec;46(5):433-50.
- Malbrain ML, De Keulenaer BL, Oda J, et al. Intra-abdominal hypertension and abdominal compartment syndrome in burns, obesity, pregnancy, and general medicine. Anaesthesiol Intensive Ther. 2015;47(3):228–240.
- Abdel-Razeq SS, Campbell K, Funai EF, Kaplan LJ, Bahtiyar MO. Normative postpartum intraabdominal pressure: potential implications in the diagnosis of abdominal compartment syndrome. Am J Obstet Gynecol. 2010;203(2):;149:e1–e4.
- Sugerman HJ. Effects of increased intra-abdominal pressure in severe obesity. Surg Clin North Am. 2001 Oct;81(5):1063-75, vi.
- Pereira BM. Abdominal compartment syndrome and intra-abdominal hypertension. Curr Opin Crit Care. 2019 Dec;25(6):688-696.
- Rajasurya V, Surani S. Abdominal compartment syndrome: Often overlooked conditions in medical intensive care units. World J Gastroenterol. 2020 Jan 21;26(3):266-278. (License: CC BY-NC 4.0)
- Cheatham ML. Abdominal compartment syndrome: pathophysiology and definitions. Scand J Trauma Resusc Emerg Med. 2009 Mar 2;17:10.
- Patel DM, Connor MJ Jr. Intra-Abdominal Hypertension and Abdominal Compartment Syndrome: An Underappreciated Cause of Acute Kidney Injury. Adv Chronic Kidney Dis. 2016 May;23(3):160-6.
- Malbrain ML, De laet IE. Intra-abdominal hypertension: evolving concepts. Clin Chest Med. 2009;30:45–70, viii.
- Newman RK, Dayal N, Dominique E. Abdominal Compartment Syndrome. 2022 Apr 21. In: StatPearls
- Malbrain ML, Cheatham ML, Kirkpatrick A, Sugrue M, Parr M, De Waele J, Balogh Z, Leppäniemi A, Olvera C, Ivatury R, D’Amours S, Wendon J, Hillman K, Johansson K, Kolkman K, Wilmer A. Results from the International Conference of Experts on Intra-abdominal Hypertension and Abdominal Compartment Syndrome. I. Definitions. Intensive Care Med. 2006 Nov;32(11):1722-32.
- Kirkpatrick AW, Brenneman FD, McLean RF, Rapanos T, Boulanger BR. Is clinical examination an accurate indicator of raised intra-abdominal pressure in critically injured patients? Can J Surg. 2000 Jun;43(3):207-11.
- Sugrue M, Bauman A, Jones F, Bishop G, Flabouris A, Parr M, Stewart A, Hillman K, Deane SA. Clinical examination is an inaccurate predictor of intraabdominal pressure. World J Surg. 2002 Dec;26(12):1428-31.
- Malbrain ML. Is it wise not to think about intraabdominal hypertension in the ICU? Curr Opin Crit Care. 2004 Apr;10(2):132-45.
- Malbrain ML. Different techniques to measure intra-abdominal pressure (IAP): time for a critical re-appraisal. Intensive Care Med. 2004 Mar;30(3):357-71.
- Nickson C. Intra-Abdominal Pressure Monitor. Life in the Fastlane. 2020.
- Cheatham ML, Safcsak K. Percutaneous catheter decompression in the treatment of elevated intraabdominal pressure. Chest. 2011 Dec;140(6):1428-1435.
- Hobson KG, Young KM, Ciraulo A, Palmieri TL, Greenhalgh DG. Release of abdominal compartment syndrome improves survival in patients with burn injury. J Trauma. 2002 Dec;53(6):1129-33; discussion 1133-4.
- Dries DJ. Abdominal compartment syndrome: toward less-invasive management. Chest. 2011 Dec;140(6):1396-1398.
- Malbrain ML, Chiumello D, Pelosi P, Bihari D, Innes R, Ranieri VM, Del Turco M, Wilmer A, Brienza N, Malcangi V, Cohen J, Japiassu A, De Keulenaer BL, Daelemans R, Jacquet L, Laterre PF, Frank G, de Souza P, Cesana B, Gattinoni L. Incidence and prognosis of intraabdominal hypertension in a mixed population of critically ill patients: a multiple-center epidemiological study. Crit Care Med. 2005 Feb;33(2):315-22.
- De Waele JJ, Kimball E, Malbrain M, Nesbitt I, Cohen J, Kaloiani V, Ivatury R, Mone M, Debergh D, Björck M. Decompressive laparotomy for abdominal compartment syndrome. Br J Surg. 2016 May;103(6):709-715.
- An G, West MA. Abdominal compartment syndrome: a concise clinical review. Crit Care Med. 2008 Apr;36(4):1304-10.
- Kron IL, Harman PK, Nolan SP. The measurement of intra-abdominal pressure as a criterion for abdominal re-exploration. Ann Surg. 1984 Jan;199(1):28-30.
- Cheatham ML, Safcsak K. Is the evolving management of intra-abdominal hypertension and abdominal compartment syndrome improving survival? Crit Care Med. 2010 Feb;38(2):402-7.