Esophagus: Heller Myotomy
Heller Myotomy
Basics
- Esophagogastric Myotomy Used for Motility Disorders
- Most Effective in Achalasia
Procedure for Achalasia
- Approach:
- Traditionally Open Anterior & Later a Left Thoracotomy
- Laparoscopic (Now Gold Standard)
- Start with Upper Endoscopy
- Evaluates for Residual Food
- Assessment During Operation
- Evaluate Mucosal Integrity After Myotomy
- Define/Mobilize Esophagus
- Open Gastrohepatic Ligament to Visualize Right Crura
- Incise Phrenoesophageal Membrane at 10 O’clock Position Along Right Crura
- Extend Clockwise to Define the Anterior Aspect
- Evaluate for Hiatus
- If Hiatal Hernia Present: Mobilize Posterior Attachments
- If No Hiatal Hernia: Leave Posterior Attachments Intact
- Dissect Fat Pad to Expose Anterior Surface
- Myotomy
- Start Myotomy 2 cm Proximal to GE Junction
- Divide Muscle Until Submucosa is Seen
- Extend 5-6 cm Proximal to GJ Junction & 2 cm Distally onto Stomach Cardia
- Dissect Muscle Fibers from Mucosa to Expose ≥ 50% of Mucosal Circumference
- Partial Fundoplication
- Done to Cover Myotomy & Prevent Reflux
- Nissen Contraindicated Due to Significant Obstruction
- *See Esophagus: Fundoplication
- Done to Cover Myotomy & Prevent Reflux
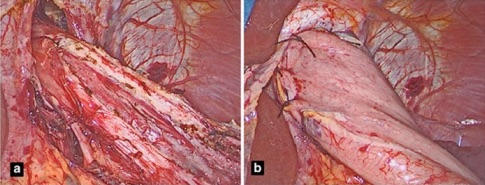
Heller Myotomy; (A) Myotomy, (B) Dor Fundoplication 1
Procedure Considerations for DES or Nutcracker Esophagus
- Length of Esophageal Body Myotomy
- Many Recommend Long Thoracic Myotomy – Requires Right Thoracotomy
- Inclusion of EG Junction in Myotomy
- Concomitant Fundoplication
Complications
- Most Common Complication: Reflux
- Intraoperative Bleeding
- Commonly from Tearing of Muscle Fibers
- Stop with Direct Pressure (Not Electrocautery – Causes Delayed Thermal Injury)
- Bleeding
- Sigmoid Esophagus
- Postoperative Dysphagia with No Obstruction
- Tx: Esophagectomy
- Perforation
- Tx: Repair Perforation & Repeat Myotomy on Opposite Wall
References
- Ramirez M, Patti MG. Changes in the diagnosis and treatment of achalasia. Clin Transl Gastroenterol. 2015 May 21;6(5):e87. (License: CC BY-NC-ND-4.0)