Small Intestine: Intussusception
Intussusception
Basics
- Definition: Loop of Bowel Invaginates/Telescopes into Itself
- Segments:
- Intussusceptum – Prolapsed Bowel
- Intussuscipiens – Recipient Bowel
- Most Common in Peds, Rare in Adults
Lead Points
- Hypertrophied Peyer Patches (Viral Infection) – Most Common Lead Point in Peds
- Meckel’s Diverticulum – Most Common Pathologic Lead Point in Peds
- Cancer – Most Common Lead Point in Adults
- Inspissated Stool of Cystic Fibrosis
- Bowel Wall Hematoma
- Idiopathic
- Pediatric Postoperative Ileus
- Classically After A Prolonged Laparotomy but Can Occur After Any Surgery, Even Nonabdominal Procedures
- Most Common Site: Ileoileal

Intussusception 1
Location
- Enteroenteric – Small Bowel into Small Bowel
- Ileocolic – Terminal Ileum into Colon
- The Most Common Site (90%)
- Colocolic – Large Bowel into Large Bowel
Symptoms
- Intermittent Abdominal Pain
- Sausage-Shaped Abdominal Mass in Peds
- Currant Jelly Stools (Blood & Mucous from Vascular Congestion)
- SBO – Nausea, Vomiting & Obstipation
Diagnosis
- Peds: US (Target Sign)
- Adults: CT
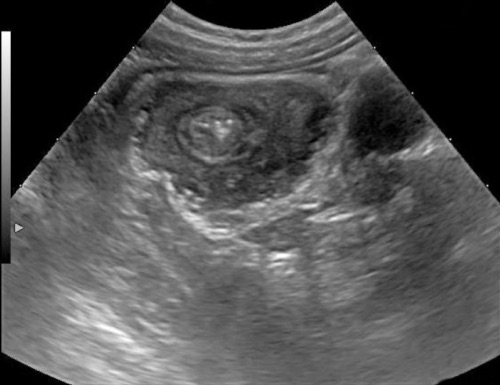
Intussusception on US 2

Intussusception on CT 3
Treatment – Pediatrics
- Primary Treatment: Air-Contrast Enema to Reduce
- Both Pneumatic (Air) or Hydrostatic (Saline/Contrast) are Acceptable
- Max Pneumatic Pressure: 120 mm Hg
- Max Barium Enema Column Height: 1 Meter/3 Feet
- Do Not Attempt Air-Contrast Enema if After a GI Surgery – Will Require Operative Reduction
- 70-85% Success; 10-20% Recur
- Both Pneumatic (Air) or Hydrostatic (Saline/Contrast) are Acceptable
- If Successful: Observe for 4 Hours & Discharge
- If Fails: Repeat Enema
- Can Repeat Multiple Times if Needed
- Risk for Perforation with Radiographic Reduction (< 1%)
- Perforation More Common in Intussuscipiens than the Intussusceptum
- Risk Similar for Pneumatic & Hydrostatic
- Increased Risk if Young (< 6 Months) & Long Duration of Symptoms (> 36 Hours)
- Surgery:
- Indications:
- Hemodynamically Unstable
- Peritonitis or Perforation
- Complete Failure of Air-Contrast Enema
- Procedure: Reduction & Resection of Any Necrotic Bowel
- Reduction: Apply Pressure to Distal End (Intussuscipiens) & Milk
- Do Not Apply Traction to the Proximal End
- Reduction: Apply Pressure to Distal End (Intussuscipiens) & Milk
- Indications:
Treatment – Adults
- Primary Treatment: Resection & Lymphadenectomy
- *There is Some Newer Evidence that Not All Patients Require Surgery, Some Present with Frequent Intussusception that May be Due to Peristalsis without Lead Point – “Safe Answer” at this Time is Surgery
References
- Joyce KM, Waters PS, Waldron RM, Khan I, Orosz ZS, Németh T, Barry K. Recurrent adult jejuno-jejunal intussusception due to inflammatory fibroid polyp – Vanek’s tumour: a case report. Diagn Pathol. 2014 Jun 27;9:127. (License: CC BY-4.0)
- Zavras N, Tsilikas K, Vaos G. Chronic Intussusception Associated with Malrotation in a Child: A Variation of Waugh’s Syndrome? Case Rep Surg. 2016;2016:5638451. (License: CC BY-4.0)
- Kee HM, Park JY, Yi DY, Lim IS. A Case of Intussusception with Acute Appendicitis. Pediatr Gastroenterol Hepatol Nutr. 2015 Jun;18(2):134-7. (License: CC BY-NC-3.0)