Vascular: Lymphatic Pathology
Lymphedema
Basics
- Definition: Swelling Due to Accumulation of Lymphatic Fluid
- From Lymphatic Obstruction or Incompetence
- Accumulation of Hyaluronan & Glycoproteins Causes Increased Fibroblasts, Keratinocytes & Macrophages
- Increased Collagen & Collective Tissue Causes Progressive Subcutaneous Fibrosis
Causes
- Primary Lymphedema Mn
- Congenital Lymphedema: Present at Birth
- Lymphedema Praecox: Presents During Childhood & Adolescence
- Most Common Primary Cause (94%)
- Lymphedema Tarda: Presents as an Adult
- Secondary (Acquired) Lymphedema
- More Common Than Primary
- Most Common Cause in U.S.: ALND
- Most Common Cause in the World: Filariasis (Wuchereria bancrofti Parasite)
Presentation
- Painless Leg Swelling
- Woody Edema: From Subcutaneous Fibrosis
- Swelling Extends into the Feet
- Stemmer Sign – Unable to Pinch Skin of Second Toe
- Feet Have Characteristic “Buffalo Hump”
- “Square Toes”
- Difficult to Distinguish from Venous Stasis
Grading
- Latent Phase: Fluid Accumulation Around Lymphatics without Edema
- Grade I: Pitting Edema Relieved by Elevation, No Fibrosis
- Grade II: Non-Pitting Edema Not Relieved by Elevation, Fibrosis Present
- Grade III: Lymphostatic Elephantiasis, Irreversible Edema from Repeated Inflammation & Fibrosis
Complications
- Recurrent Cellulitis
- Protein-Rich Fluid Provides a Good Substrate for Bacterial Growth
- Lymphangiosarcoma
- Presents as Multicentric Raised Blue-Red Nodules
- Highly Aggressive with Poor Prognosis
- Metastasizes to Lung Early
- Stewart-Treves Syndrome: From Chronic Lymphedema
- Majority Occur Post Mastectomy or ALND
- Presentation: Dark Purple Lesions (Bruises) of Arm 5-10 Years Later
- Treatment: Early Wide Local Excision
- Often Requires Amputation
- Malnutrition
- From Severe Loss of Proteins
Diagnosis
- Most Often a Clinical Diagnosis
- Strongly Consider Venous US to Rule Out Venous Pathology
- If Uncertain: Lymphoscintigraphy (Nuclear Medicine Radiotracer)
Treatment
- Initial Approach: Conservative Management
- Compression Stockings
- Elevation
- Physiotherapy & Manual Lymphatic Decompression (Massage Technique)
- Skin Care
- Weight Loss
- Microsurgery
- Options:
- Lymphovenous Anastomosis
- Vascularized Lymph Node Transfer
- Indications:
- Failure of Conservative Management
- Recurrent Cellulitis
- Functional Limitation
- Deformity
- Refractory Pain
- Impaired Quality of Life
- Options:

Lymphedema; (Left) Left Leg, (Right) Right Arm 1

Lymphangiosarcoma 16 Years After Mastectomy 2
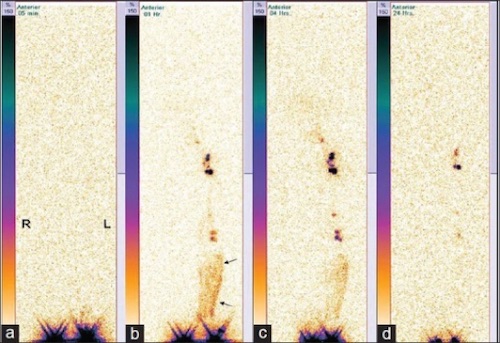
Serial Lymphoscintigraphy Showing Lymphedema ((a) Immediate, (b) 1h, (c) 4h, (d) 24h); RLE No Uptake in Lymph Nodes or Channels, LLE with Dermal Backflow (Arrows) 3
Similar Pathology
- Venous Stasis
| Venous Stasis | Lymphedema | |
| Pitting | Yes | Early, Not Late |
| Feet/Toes | Spares | Affects Mn |
| Hyperpigmentation | Yes | No |
| Recurrent Cellulitis | No | Yes |
- Lipedema
- Symmetric Leg Enlargement from Fat Distribution
- Similar to Lymphedema but Does Not Affect Feet
- Tx: Weight Loss
Other Lymphatic Pathology
Lymphangitis
- Inflammation Along Lymphatic Channels
- Most Commonly from a Skin Infection
- Most Common Organisms:
- Acute Infection: Group A Streptococcus
- Chronic Infection: Sporothrix schenckii
- Presentation: Tender Red Linear Streaking
- Tx: Penicillin
- Clindamycin if Allergic
Lymphocele (Cystic Lymphangioma)
- Lymphatic Fluid Collection without an Epithelial Lining
- Prone to Leakage (No Platelets or Clotting Factors)
- Most Common Causes: Surgery or Trauma
- Most Common Site: Groin
- Treatment: Percutaneous Drainage
- If Fails: Surgical Resection (Some Prefer as the Primary Treatment)

Lymphangitis After Bug Bites 4
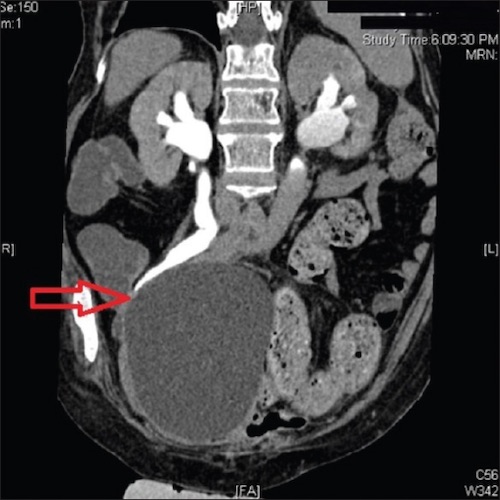
Pelvic Lymphocele After Radical Cystectomy 5
Mnemonics
Presentation of Primary Lymphedema
- P-P: Praecox in Peds
- Tardy/Later: Tarda in Adults
Venous Stasis vs Lymphedema
- Venous – “V” Looks Like a Single Leg WITHOUT the Foot
- Lymphatic – “L” Looks Like a Single Leg WITH the Foot (Lymphedema Affects the Feet)
References
- Cannon S. Pneumatic compression devices for in-home management of lymphedema: two case reports. Cases J. 2009 Mar 23;2:6625.(License: CC BY-3.0)
- Sepah YJ, Umer M, Qureshi A, Khan S. Lymphangiosarcoma of the arm presenting with lymphedema in a woman 16 years after mastectomy: a case report. Cases J. 2009 Sep 1;2:6887. (License: CC BY-3.0)
- Kalawat TC, Chittoria RK, Reddy PK, Suneetha B, Narayan R, Ravi P. Role of lymphoscintigraphy in diagnosis and management of patients with leg swelling of unclear etiology. Indian J Nucl Med. 2012 Oct;27(4):226-30. (License: CC BY-NC-SA-3.0)
- Akinerov. Wikimedia Commons. (License: CC BY-SA-4.0)
- Bankar SS, Bakshi GK, Prakash G, Sable NP. Delayed complication of pelvic lymphocele: Ileal conduit obstruction. Indian J Urol. 2015 Jul-Sep;31(3):254-5. (License: CC BY-NC-SA-3.0)