Mechanical Ventilation: Modes
David Ray Velez, MD
The Operative Review of Surgery. 2023; 1:283-290.
Table of Contents
Overview
Definitions
- Minute Ventilation (MV): Amount of Air that Enters the Lungs per Minute
- MV = RR x Vt
- Respiratory Rate (f/RR): Number of Breaths Delivered per Minute
- Tidal Volume (Vt): Volume of Air Delivered with Each Breath
- Pressure Support (PS): Additional Pressure Added to PEEP to Cause Inspiration
- Also Known as Inspiratory Pressure (PI) or Change in Pressure (∆P)
- Positive End Expiratory Pressure (PEEP): Positive Pressure Remaining in Airways at the End of Expiration
- Fraction of Inspired Oxygen (FiO2): Percentage of Oxygen in Air Delivered to the Patient
- Breath Types:
- Patient-Trigger Breath: A Breath Initiated by the Patient’s Own Respiratory Drive (Can Be Triggered by Pressure Changes, Flow Changes, Volume Changes, or Shape-Signal)
- Machine-Triggered Breath: A Breath Automatically Cycled by the Ventilator without Any Patient Initiation
Modes
- Non-Controlled Ventilation
- Continuous Positive Airway Pressure (CPAP)
- Pressure Support Ventilation (PSV)
- PSV Variations:
- CPAP with PSV (Similar to BPAP)
- Automatic Tube Compensation (ATC)
- Volume Support Ventilation (VSV)
- Volume-Controlled Ventilation
- Controlled Mechanical Ventilation (CMV)
- Assist-Control Ventilation (AC)
- Synchronized Intermittent Mechanical Ventilation (SIMV)
- Pressure-Controlled Ventilation
- Controlled Mechanical Ventilation (CMV)
- Assist-Control Ventilation (AC)
- Synchronized Intermittent Mechanical Ventilation (SIMV)
- Advanced Modes of Ventilation
- Airway Pressure Release Ventilation (APRV)
- High-Frequency Oscillatory Ventilation (HFOV)
- Adaptive Support Ventilation (ASV)
- Neurally Adjusted Ventilatory Assist (NAVA) Ventilation
Noninvasive Ventilation
Ventilator Management
- *See Mechanical Ventilation: Settings
- *See Mechanical Ventilation: Ventilator Management
- *See Mechanical Ventilation: Airway Pressures
- *See Mechanical Ventilation: Ventilator Liberation
Complications
Non-Controlled Ventilation
Continuous Positive Airway Pressure (CPAP)
- Provides a Continuous Pressure Level (Similar to PEEP)
- No Additional Support Provided to Patient-Triggered Breaths
- All Breaths are Patient-Triggered – Patient Determines the Rate and Volume
- General Settings:
- CPAP Pressure: 5-15 cmH2O
- FiO2: Adjusted as Needed
Pressure Support Ventilation (PSV)
- Additional Pressure Support Provided to Patient-Triggered Breaths
- All Breaths are Patient-Triggered – Patient Determines Rate and Volume
- General Settings:
- Pressure Support: 5-20 cmH2O
- FiO2: Adjusted as Needed
PSV Variations
- CPAP with PSV (Similar to BPAP)
- Pressure Support is in Addition to PEEP
- PSV 10/5 Indicates 5 cmH2O of PEEP and 15 cmH2O During Support
- Automatic Tube Compensation (ATC)
- Ventilator Programming Continuously Adjusts Pressure Support to the Level Needed to Overcome the Endotracheal Tube
- ATC Can Be Used as a Component and Combined with Any Conventional Ventilator Mode
- Volume Support Ventilation (VSV)/ Volume Targeted Ventilation (VTV)
- Continuously Adjusts Pressure Support to the Level Needed to Achieve a Target Tidal Volume
- Some Evidence Suggests Decreased Weaning Time and Total Ventilation Time 1
- Significant Literature Evaluating its Use in Neonates 2,3
General Use
- Used Primarily for Ventilator Weaning
- Pressure Used to Overcome the Resistance of the Endotracheal Tube
- Disadvantages:
- Higher Work of Breathing and Can Cause Respiratory Fatigue
- Can Result in Carbon Dioxide Retention and Acidosis
- Poor Choice for Full Ventilatory Support
Volume-Controlled Ventilation
Controlled Mechanical Ventilation (CMV)
- Mechanism:
- Sets a Controlled Minute Ventilation (Rate and Volume)
- Does Not Allow Any Patient-Triggered Breaths
- Advantages:
- Lowest Work of Breathing
- Set Minute Ventilation is Easily Adjusted
- Disadvantages:
- Less Comfortable
- May See Ventilator Dyssynchrony with Wasted Effort
- May Require Deeper Sedation or Paralytics
Assist-Control Ventilation (AC)
- Mechanism:
- Sets a Minimum Minute Ventilation (Rate and Volume)
- Allows Patient-Triggered Breaths in Addition to Set Minimum Breaths
- Patient-Triggered Breaths are at the Set Volume
- Advantages:
- Increased Comfort
- Allows Sedation Weaning
- Improved Ventilator Synchrony
- Lower Work of Breathing than SIMV
- Disadvantages:
- Higher Work of Breathing than CMV
- Can Hyperventilate with “Breath-Stacking”
Synchronized Intermittent Mechanical Ventilation (SIMV)
- Mechanism:
- Sets a Minimum Minute Ventilation (Rate and Volume)
- Allows Patient-Triggered Breaths in Addition to Set Minimum Breaths
- Patient-Triggered Breaths are at a Patient’s Own Volume
- Advantages:
- May Allow Exercise of Respiratory Muscles – No Proven Advantage to SIMV 4
- Disadvantages:
- Highest Work of Breathing and Can Cause Respiratory Fatigue
- Less Comfortable
- Can Hyperventilate with “Breath-Stacking”
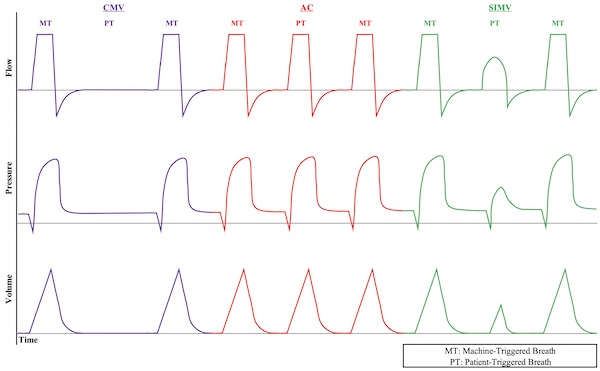
Time Graphs of Volume-Controlled Ventilation Modes 5
Pressure-Controlled Ventilation
Mechanism
- Provides a Set Airway Pressure for the Given Inspiratory Time
- Adjusts the Inspiratory Pressure Level Instead of Tidal Volume
Modes
- Delivered Using Same Modes as Volume-Controlled Ventilation (*See Above)
- Controlled Mechanical Ventilation (CMV)
- Assist-Control Ventilation (AC)
- Synchronized Intermittent Mechanical Ventilation (SIMV)
Use
- Used Much Less Often than Volume-Controlled Ventilation
- Advantages:
- Peak Inspiratory Pressure (PIP) is Constant (Inspiratory Pressure + PEEP)
- Decreased Risk for Barotrauma by Lower PIP
- *See Mechanical Ventilation: Airway Pressures
- Increased Mean Airway Pressure and Duration of Alveolar Recruitment
- Increased Comfort and Decreased Work of Breathing
- May Allows Better Synchrony with the Ventilator
- Peak Inspiratory Pressure (PIP) is Constant (Inspiratory Pressure + PEEP)
- Disadvantages:
- Tidal Volume and Minute Ventilation is Variable
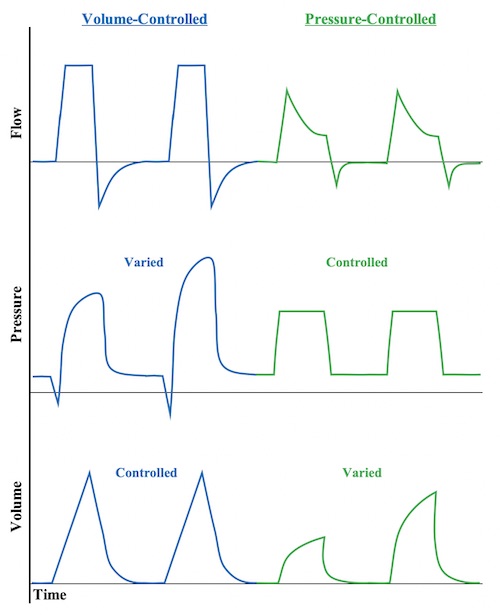
Time Graphs of Volume- vs Pressure-Controlled Ventilation 5
Advanced Modes of Ventilation
Airway Pressure Release Ventilation (APRV)
- Mechanism:
- Maintains High Pressure (P High) for an Extended Time (T High) to Optimize Oxygenation
- Pressure Released (P Low) for Short Time Period of Time (T Low) to Allow Ventilation
- Longer Inspiratory/Expiratory Ratio: 80-95%
- Spontaneous Breathing is Permitted but Will Have Low Tidal Volumes at the Higher Pressures
- Most Commonly Used for Severe ARDS When Having Difficulty Oxygenating on Other Modes 6,7
- Settings:
- P High 25-35 cmH2O
- T High 4.5-6.0 Seconds
- P Low 0 cmH2O
- T Low 0.5-0.8 Seconds
- FiO2: Adjusted as Needed
- Keep Automatic Tube Compensation (ATC) on if Spontaneous Breathing
- Advantages:
- Maximize Alveolar Recruitment and Oxygenation
- Lung-Protective (Lower Peak Pressures and Less Barotrauma)
- More Comfortable than CMV – Allows Decreased Sedation
- Disadvantages:
- Not Ideal if Requiring Heavy Sedation – Spontaneous Breathing is Important for Ventilation
- Generally Avoided in Severe Obstructive Airway Disease – Risks Hyperinflation with Increased Pressure and Barotrauma
- Generally Avoided if Needing High Ventilatory Requirements
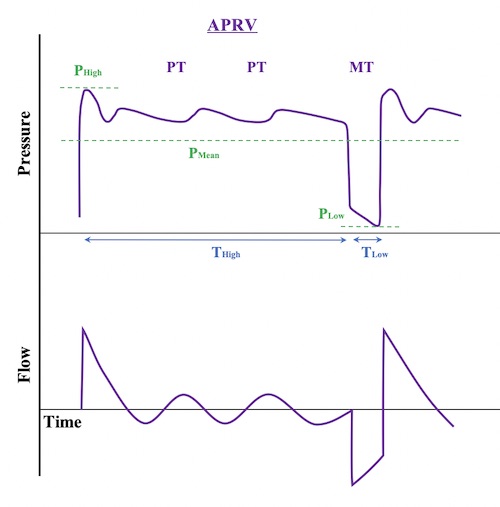
APRV Time Graphs 5
High-Frequency Oscillatory Ventilation (HFOV)
- Mechanism:
- Very High Respiratory Rate (300-900 Breaths per Minute) by a High-Frequency Oscillatory Pump
- Rate is So Fast That the Airway Pressure Merely Oscillates Around a Constant Mean Airway Pressure
- Does Not Produce Large Bulk Tidal Volumes but Rather Creates a Relatively Continuous Gas Flow
- Most Commonly Used for Severe ARDS Only When Having Difficulty Oxygenating on Other Modes – Should Not Be Used Routinely (May Actually Increase Mortality) 8,9
- Settings:
- Bias Flow: 30-40 L/min
- Frequency (F): 3-15 Hz (1 Hz is Equivalent to 60 Breaths per Minute)
- Inspiratory Time: 33% (I:E Ratio of 1:2)
- Mean Airway Pressure (MAP): 25-35 cmH2O
- Generally Started at 2-3 cmH2O Above the Prior MAP on CMV
- Power/Amplitude (Delta P): 30-90 cmH2O
- Sets the Variation Around the MAP
- Appropriate Amplitude is Based on “Chest Wiggle”/Vibration
- FiO2: Adjusted as Needed
- Advantages:
- Maintains Alveolar Recruitment and Oxygenation
- Lung-Protective (Lower Peak Pressures and Less Barotrauma)
- Disadvantages:
- Significant Discomfort and Requires Heavy Sedation or Paralysis
- Decreased Expiratory Time Creates Risk for Hyperinflation with Increased Pressure and Barotrauma
- High Risk of Hemodynamic Instability Due to High Mean Airway Pressures
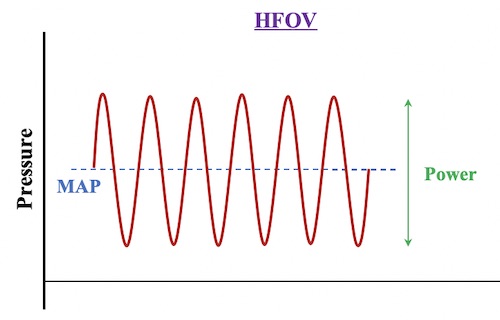
HFOV Pressure-Time Graph 5
Adaptive Support Ventilation (ASV)
- Mechanism:
- Continual Adjustments are Automatically Made to Respiratory Rate and Inspiratory Pressure to Achieve a Goal Minimum Minute Ventilation (MMV)
- The Ventilator Calculates Optimal Settings by the “Otis Equation” to Minimize Work of Breathing 10,11
- Accounts for Respiratory Mechanics (Resistance, Compliance, Dead Space – Calculated)
- Patient-Triggered Breaths are Given Pressure Support
- Machine-Controlled Breaths are Given as Needed to Achieve a Calculated Respiratory Rate
- Continual Adjustments are Automatically Made to Respiratory Rate and Inspiratory Pressure to Achieve a Goal Minimum Minute Ventilation (MMV)
- Settings:
- Ventilate by Setting a Percentage of Minimum Volume (MinVol) of Desired Minute Ventilation
- 100% Normal, 120% in ARDS, 90% in Asthma, 110% in Others
- Add 20% for Fevers > 101.3 F
- Oxygenate by Setting PEEP and FiO2
- Ventilate by Setting a Percentage of Minimum Volume (MinVol) of Desired Minute Ventilation
- Advantages:
- Decreased Work of Breathing
- Attempts Lung Protective Strategies to Prevent Volutrauma, Barotrauma and Auto PEEP
- May Decrease Ventilator Weaning Time in COPD
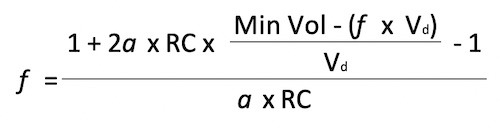
Otis Equation for Adaptive Support Ventilation 5
Neurally Adjusted Ventilatory Assist (NAVA) Ventilation
- Mechanism:
- Catheter Implanted in a Gastric Tube Detects Electrical Discharge in the Diaphragm
- Diaphragmatic Excitation Triggers a Mechanical Breath
- The Degree of Assist Varies by the Amplitude of the Electrical Discharge – Tidal Volume Continuously Varies
- Advantages:
- Neural-Ventilator Coupling (Time Between Spontaneous Breath and Delivered Mechanical Breath) is Faster than Conventional Modes
- May Increase Ventilator Synchrony
- Disadvantages:
- Requires Spontaneous Breathing – Unable to Use with Heavy Sedation or Blunted Respiratory Drive
References
- Sancar NK, Özcan PE, Şentürk E, Selek Ç, Çakar N. The Comparison of Pressure (PSV) and Volume Support Ventilation (VSV) as a ‘Weaning’ Mode. Turk J Anaesthesiol Reanim. 2014 Aug;42(4):170-5.
- Peng W, Zhu H, Shi H, Liu E. Volume-targeted ventilation is more suitable than pressure-limited ventilation for preterm infants: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2014 Mar;99(2):F158-65.
- Klingenberg C, Wheeler KI, McCallion N, Morley CJ, Davis PG. Volume-targeted versus pressure-limited ventilation in neonates. Cochrane Database Syst Rev. 2017 Oct 17;10(10):CD003666.
- de Godoi TB, Marson FAL, Palamim CVC, Cannonieri-Nonose GC. Influence of ventilatory strategies on outcomes and length of hospital stay: assist-control and synchronized intermittent mandatory ventilation modes. Intern Emerg Med. 2021 Mar;16(2):409-418.
- Velez DR. Mechanical Ventilation: Modes. The Operative Review of Surgery. 2023.
- Mireles-Cabodevila E, Dugar S, Chatburn RL. APRV for ARDS: the complexities of a mode and how it affects even the best trials. J Thorac Dis. 2018 Apr;10(Suppl 9):S1058-S1063.
- Zhou Y, Jin X, Lv Y, Wang P, Yang Y, Liang G, Wang B, Kang Y. Early application of airway pressure release ventilation may reduce the duration of mechanical ventilation in acute respiratory distress syndrome. Intensive Care Med. 2017 Nov;43(11):1648-1659.
- Sklar MC, Fan E, Goligher EC. High-Frequency Oscillatory Ventilation in Adults With ARDS: Past, Present, and Future. Chest. 2017 Dec;152(6):1306-1317.
- Ng J, Ferguson ND. High-frequency oscillatory ventilation: still a role? Curr Opin Crit Care. 2017 Apr;23(2):175-179.
- Otis AB, Fenn WO, Rahn H. Mechanics of breathing in man. J Appl Physiol. 1950;2:592–607.
- Tehrani FT, Roum JH. Flex: A new computerized system for mechanical ventilation. J Clin Monit Comput. 2008;22:121–30.