Skin & Soft Tissue: Melanoma
Melanoma
Basics
- Tumor from Basal Melanocytes
- Highest Skin Cancer Mortality
Risk Factors
- Sun Exposure
- History of Melanoma
- Multiple Atypical Moles or Dysplastic Nevi
- Genetic Mutations
Presentation
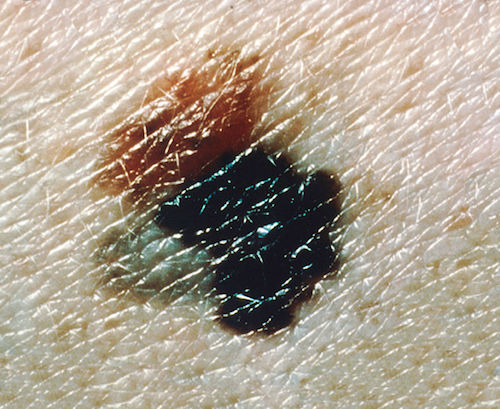
- Classic “ABCDE” Appearance:
- Asymmetric
- Borders Irregular
- Color Variegation
- Most Ominous Color: Blue
- Diameter > 6 mm
- Evolution Over Time
- Pigmented Lesion Out of Character with the Patient’s Mole Pattern
- New Pigmented Lesion After Age 40

Melanoma 1
Location
- Most Common Site:
- Men: Back
- Women: Legs
- Mets:
- Most Common Mets: Lung
- Melanoma is the Most Common Met to the Small Bowel
- Associated with S-100 Protein (Also Seen in Neurofibroma & Schwannoma)
Types
- In Situ (Hutchinson’s Freckle)
- Epidermis Only
- Lentigo Maligna
- Least Aggressive Subtype
- Superficial Spreading
- Most Common Type
- Radial Growth Initially, But Can Grow Vertically if Untreated
- Acral Lentiginous
- Palms/Soles of Blacks
- Very Aggressive
- Subungual: Below Fingernail
- Nodular
- Vertical Growth First
- Most Aggressive

Lentigo Maligna 2
Superficial Spreading 1

Acral Lentiginous 3

Subungual 4

Nodular 5
Prognosis
- Poor Prognosis:
- Depth (Not Level of Invasion)
- Stage
- LDH
- Ulceration
- Mitotic Rate
- Node Status – Most Important
- Breslow Thickness
- Based on Total Depth
- Clark Level (Not Used Anymore)
- Based on Level of Invasion
- I: Epidermis (In Situ)
- II: Papillary Dermis
- III: Junction of Papillary/Reticular Dermis
- IV: Reticular Dermis
- V: Subcutaneous
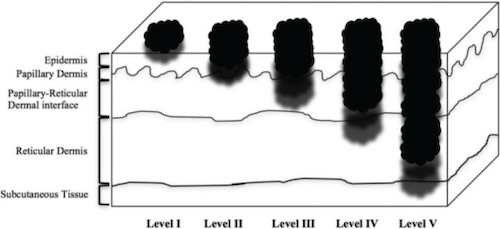
Melanoma Clark Level 6
Melanoma – TNM Staging (AJCC 8)
TNM
| T | N | M | |
| 1 | ≤ 1.0 mm
1a: < 0.8 mm without Ulceration 1b: ≥ 0.8 mm without Ulceration or ≤ 1.0 mm With Ulceration |
1+ LN | 1a: Distant Skin, Soft Tissue or LN
1b: Lung 1c: Visceral Sites 1d: CNS |
| 2 | > 1.0 mm | 2-3+ LN | |
| 3 | > 2.0 mm | ≥ 4+ LN | |
| 4 | > 4.0 mm |
- T Stage Sub-Staging:
- TXa: Without Ulceration
- TXb: With Ulceration
- N Stage Sub-Staging:
- NXa: Clinically Occult
- NXb: Clinically Detected
- NXc: Presence of In-Transit, Satellite and/or Microsatellite Metastases
- N1c: No LN+
- N2c: 1 LN+
- N3c: ≥ 2 LN+
- M Stage Sub-Staging:
- M1x(0): LDH Not Elevated
- M1x(1): LDH Elevated
- T Stage Sub-Staging:
Stage
| Stage | T | N | M | |
| I | A | T1a-b | N0 | M0 |
| B | T2a | N0 | M0 | |
| II | A | T2b-3a | N0 | M0 |
| B | T3b-4a | N0 | M0 | |
| C | T4b | N0 | M0 | |
| III | A | T1a/b-T2a | N1a or N2a | M0 |
| B | T0 | N1b/c | M0 | |
| T1a/b-T2a | N1b/c or N2b | M0 | ||
| T2b-T3a | N1a-N2b | M0 | ||
| C | T0 | N2b-N2c or N3b-N3c | M0 | |
| T1a-T3a | N2c-N3c | M0 | ||
| T3b-T4a | N1a-N3c | M0 | ||
| T4b | N1a-N2c | M0 | ||
| D | T4b | N3a-N3c | M0 | |
| IV | Any T | Any N | M1 | |
Melanoma – Treatment
Management of Primary Lesion
- If Previously Diagnosed by Shave-Biopsy with Positive Deep Margin: Need Full Thickness Biopsy to Determine Depth
- Primary Treatment: Wide Local Excision
- Margins: Mn
- In Situ: 0.5-1.0 cm
- ≤ 1.0 mm Depth: 1.0 cm
- > 1.0 mm Depth: 1.0-2.0 cm
- > 2.0 mm Depth: 2.0 cm
- In General Length to Width Ratio of 3:1 Required to Allow Primary Closure
- Subungual Melanomas: Amputation of Distal Digit (1 cm Margin)
Management of Lymph Nodes
- Consider Systemic Immunotherapy for any Stage III Disease
- Clinically Palpable Lymph Nodes: FNA (Fine Needle Aspiration)
- Resect if Positive (Goal is to Clear, Not to Stage)
- Sentinel Lymph Node Biopsy (SLNB)
- Indications: ≥ T1b (≥ 0.8 mm or Ulcerating)
- Indications for Node Retrieval:
- Dye: All Nodes That Have Taken Up Dye
- Radiotracer: All Nodes with > 10% Highest Ex-Vivo Count
- Any Firm Node, Regardless of Dye/Radiotracer
- Most Commonly Sent for Permanent Pathology – Frozen Section Generally Abandoned Due to Low Sensitivity
- Completion Lymphadenectomy:
- Axillary Lymph Node Dissection (ALND)
- Indications: Positive SLNB or Axillary Nodes with No Primary
- Include Level III Nodes for Melanoma
- Groin Dissection
- Superficial Groin (Inguinofemoral) Dissection
- Indications: SLNB Positive
- Femoral Triangle Borders:
- Lateral: Sartorius
- Medial: Adductor Longus
- Superior: Inguinal Ligament
- Deep Inguinal (Iliac-Obturator) Dissection
- Indications:
- Positive Cloquet’s Lymph Node – Within Femoral Canal (Bridge Between Superficial & Deep Nodal Basins)
- > 4 Positive Lymph Nodes on Superficial Dissection
- Enlarged Ileo-Obturator Lymph Nodes on Preoperative Imaging
- Clinically Palpable or Extracapsular Invasion of Femoral Lymph Nodes
- Procedure:
- Divide Inguinal Ligament Medially (Avoid Femoral Vessels)
- Start at Common Iliac Vessels and Extend Caudally
- Suture Inguinal Ligament to Lacunar Ligament to Close Femoral Canal
- Close Residual Defects with Mesh or Sartorius Flap
- Indications:
- Superficial Groin (Inguinofemoral) Dissection
- Axillary Lymph Node Dissection (ALND)
- If Sentinel LN+ May Consider US Observation:
- Observation with US & Completion LN Dissection Have Similar Melanoma-Specific Survival
- US Schedule:
- Every 4 Months for 2 Years
- Then Every 6 Months for 3 Years
- Then Annually
Management of Metastases
- Limited (Resectable): Systemic Therapy & Resect
- Disseminated (Unresectable): Systemic Therapy
Systemic Therapies
- Immunotherapy:
- Nivolumab: Monoclonal Antibody (mAb) Against PD-1
- Pembrolizumab: Monoclonal Antibody (mAb) Against PD-1
- Ipilimumab: Monoclonal Antibody (mAb) Against CTLA-4
- Molecular Targeted Therapy for BRAF V600-Activating Mutations:
- Dabrafenib (BRAF Inhibitor) & Trametinib (MEK Inhibitor)
- Vemurafenib (BRAF Inhibitor) & Cobimetinib (MEK Inhibitor)
- Encorafenib (BRAF Inhibitor) & Binimetinib (MEK Inhibitor)
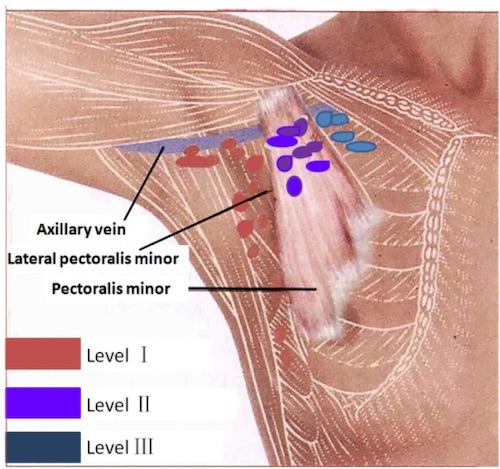
Axillary Lymph Node Levels 7
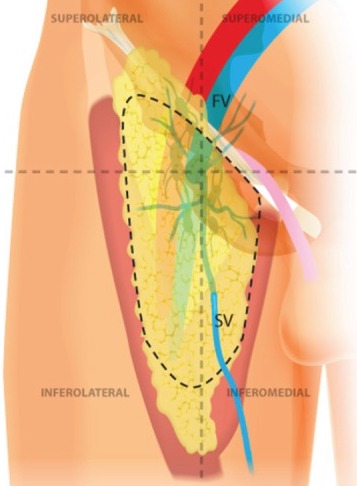
Superficial Groin Dissection 8
Mnemonics
Melanoma Margins
- ≤ 1 mm: 1 cm
- 1-2 mm: 1-2 cm
- > 2 mm: 2 cm
References
- National Cancer Institute. Wikimedia Commons. (License: Public Domain)
- Bari O, Cohen P R (February 13, 2017) Tumoral Melanosis Associated with Pembrolizumab-Treated Metastatic Melanoma. Cureus 9(2): e1026. (License: CC BY-3.0)
- Xavier-Júnior, J.C.C., Munhoz, T., Souza, V. et al.Focal invasiveness in complete histological analyses of a large acral lentiginous melanoma. Diagn Pathol 10, 73 (2015). (License: CC BY-4.0)
- Wawjak. Wikimedia Commons. (License: CC BY-4.0)
- Ox6adb015. Wikimedia Commons. (License: CC BY-SA-3.0)
- Leilabadi SN, Chen A, Tsai S, Soundararajan V, Silberman H, Wong AK. Update and Review on the Surgical Management of Primary Cutaneous Melanoma. Healthcare (Basel). 2014 Jun 10;2(2):234-49. (License: CC BY-3.0)
- Lu Q, Hua J, Kassir MM, Delproposto Z, Dai Y, Sun J, Haacke M, Hu J. Imaging lymphatic system in breast cancer patients with magnetic resonance lymphangiography. PLoS One. 2013 Jul 5;8(7):e69701. (License: CC BY-4.0)
- Sotelo R, Cabrera M, Carmona O, de Andrade R, Martin O, Fernandez G. Robotic bilateral inguinal lymphadenectomy in penile cancer, development of a technique without robot repositioning: a case report. Ecancermedicalscience. 2013 Sep 26;7:356.(License: CC BY-3.0)