Acute Mesenteric Ischemia (AMI)
Victor Roman Steele, MD
The Operative Review of Surgery. 2023; 1:253-261.
Table of Contents
Definitions
Definitions
- Intestinal Ischemia: Inadequate Blood Supply to Meet Demands of Intestines
- Mesenteric Ischemia: Ischemia of the Small Intestine (Often Used Interchangeably with Intestinal Ischemia)
- Colonic Ischemia: Ischemia of the Large Intestine
- Splanchnic/Visceral Ischemia: A Broader Term to Describe Ischemia of the Intestine and Other Solid Organs (Liver, Kidney, Spleen)
Classification/Timing
- Acute Mesenteric Ischemia (AMI) – Rapid Onset Over Hours-Days
- Most Common Cause: Arterial Embolism
- Chronic Mesenteric Ischemia (CMI) – Slow Onset Over Weeks-Months
- Most Common Cause: Arterial Thrombosis/Atherosclerosis
- *See Chronic Mesenteric Ischemia
Causes
- Arterial Pathology:
- Arterial Embolism
- Arterial Thrombosis
- Mesenteric Venous Thrombosis (MVT)
- Non-Occlusive Mesenteric Ischemia (NOMI)
- Other General Causes of Intestinal Ischemia:
- Incarcerated/Strangulated Hernia
- Internal Hernia
- Adhesions
- Bowel Volvulus
- Extreme Bowel Distention
- Vasculitis
Bowel Ischemia 1,2
- Visceral Perfusion Fails to Meet Metabolic Demand
- Inadequate Collateral Circulation, Smaller Caliber Vessels, and Longer Duration of Ischemia Increase the Risk of Damage
- Bowel Autoregulation Can Enhance Oxygen Extraction and Perfusion by Vasodilation
- Small Intestine Can Compensate for a 75% Reduction in Mesenteric Blood Flow for up to 12 Hours 3
- Bowel Damage is Caused by Both Ischemic Hypoxia and Reperfusion Injury
- Ischemia Can Progress to Frank Bowel Necrosis and Perforation
- Bowel Mucosa is Affected First Due to Higher Metabolic Demand
- Ischemia Causes the Release of Toxic Byproducts and Oxygen Free Radicals
- Can Incite a Multisystem Organ Failure
Mortality
- Historically Associated with Exceptionally High Mortality Rates (70-90%) 4,5
- In-Hospital Mortality Still High But Significantly Decreased (17-21%) 6,7

Necrotic Bowel from Mesenteric Ischemia 8
Etiology
Arterial Embolism
- Most Common Cause of Acute Mesenteric Ischemia (40-50%) 9,10
- Embolic Source:
- Heart (Left Atrium, Ventricle, or Valves) – Most Common
- Aortic Plaques
- Risk Factors: 9,11
- Atrial Fibrillation
- Recent Myocardial Infarction
- Prosthetic Valves
- Ventricular Aneurysm
- Rheumatic Heart Disease
- SMA is at High Risk for Embolism Due to Acute Angle Off Aorta (30-60 Degrees) 12,13
- Decreased Angle of Takeoff Compared to Other Mesenteric Vessels
- Most Common Site: SMA Just Distal to the Middle Colic Artery
- SMA Begins to Narrow After the Middle Colic Takeoff
- Ischemia Spares the Proximal Jejunum and Transverse Colon
- 20% are Associated with Concurrent Emboli to Other Structures (Spleen, Kidney, etc.) indicating a Proximal Embolic Source 14
Arterial Thrombosis
- Second Most Common Cause of Acute Mesenteric Ischemia (20-30%) 9,10
- Often Have History of Chronic Mesenteric Ischemia with “Food Fear” and Weight Loss
- *See Chronic Mesenteric Ischemia
- Due to Prolonged Development, there is Usually Extensive Collateral Formation from the Celiac Artery to Compensate
- Most Common Site: SMA Origin
- Ischemia Involves the Entire Distribution
- Symptomatic SMA Thrombosis Most Often Has a Concurrent Celiac Occlusion – Due to Collaterals that Would Otherwise Compensate 15
- Higher Mortality Than Arterial Embolism
Mesenteric Venous Thrombosis (MVT)
- Least Common Cause of Acute Mesenteric Ischemia (5-10%) 9,10
- Often Associated with Virchow’s Triad (Vessel Injury, Blood Flow Stasis, and Hypercoagulability)
- Classification:
- Primary: Idiopathic
- Secondary: From Underlying Process (80-90% – Most Common) 10
- 50% Have a Prior History of Thrombosis 16
- Often Vague and Less Dramatic Presentation Over 1-2 Weeks with Bloating, Distention, and Nausea
Non-Occlusive Mesenteric Ischemia (NOMI)
- Third Most Common Cause of Acute Mesenteric Ischemia (20%) 9,10
- Ischemia Without an Associated Thromboembolic Occlusion
- Risk Factors:
- Decreased Perfusion from Low Cardiac Output (Most Common Cause)
- Hypovolemia
- Shock States
- Systemic Vasopressors
- Prior Myocardial Infarction
- Abdominal Compartment Syndrome
- Aortic Regurgitation
- Hepatic or Renal Failure/Hemodialysis
- Cocaine-Induced Vasoconstriction
- Most Vulnerable Sites: Watershed Areas
- Often More Insidious Onset than Arterial Disease
- Highest Mortality Rate – Often Associated with Multiple Organ Failure, Heart Failure, and Sepsis

Mesenteric Ischemia with Embolism on CTA 17

Mesenteric Ischemia from SMA Stenosis on CTA 18

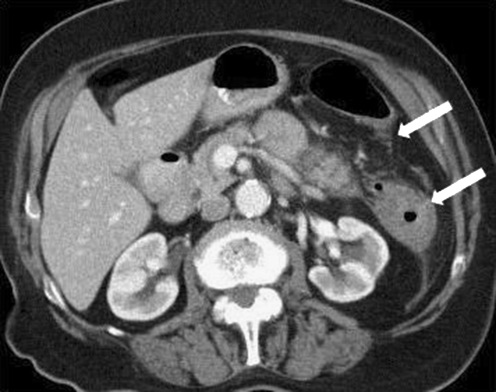
Mesenteric Venous Thrombosis on CTA: SMV Thrombus (Blue Arrows), Intact SMA (Red Arrows), Edematous Jejunum (White Arrows) 19
NOMI with Ischemia at Griffith’s Point 20
Presentation and Diagnosis
Presentation 21,22
- Abdominal Pain (95% – Most Common Symptom)
- Sudden and Severe
- “Pain Out of Proportion” – Patient Reports Significant Abdominal Pain That Does Not Correlate to Physical Exam Findings with Only Mild Abdominal Tenderness
- Nausea and Vomiting (35-44%)
- Diarrhea (35%)
- Blood per Rectum (16%)
- Classically Sudden and Forceful Bloody Diarrhea
- Abdominal Distention
- Fever
- *Clinical Scenarios and History Can Help to Differentiate the Etiology
Diagnosis
- CTA is the Preferred Diagnostic Imaging and Should Be Performed as Soon as Possible 10
- Poor Diagnostic Studies:
- Mesenteric Duplex US – Obscured by Bowel Gas in the Acute Setting and More Operator Dependent
- Plain Film X-Ray
- Laboratory Studies – May See Elevated Leukocytosis (90%) and Lactate (88%) but Not Specific 23
Treatment
Initial Managements 10,24,25
- Aggressive Fluid Resuscitation
- Aggressive Electrolyte Correction
- Nasogastric Decompression
- IV Heparin Infusion
- Not Necessary for NOMI
- Broad-Spectrum Antibiotics (High Risk for Bacterial Translocation and Sepsis with Early Loss of the Mucosal Barrier)
- Indications for Emergent Exploratory Laparotomy: 25
- Hemodynamically Unstable
- Overt Peritonitis
- Perforation
Definitive Treatment
- Arterial Embolus: Open SMA Embolectomy
- May Consider Endovascular Intervention in Stable and Nonperitoneal Patients
- Arterial Thrombosis: Open SMA Bypass
- May Consider Endovascular Intervention in Stable and Nonperitoneal Patients
- Mesenteric Venous Thrombosis (MVT): IV Heparin Infusion
- Rescue Options if Continues to Decompensate Despite Anticoagulation: 10
- Percutaneous Transhepatic Thrombolysis
- TIPS with Aspiration or Thrombolysis
- Arterial Approaches via the SMA
- Will Also Require Prolonged Anticoagulation at Discharge (6 Months vs Lifelong)
- Rescue Options if Continues to Decompensate Despite Anticoagulation: 10
- Non-Occlusive Mesenteric Ischemia (NOMI): Improve Circulatory Support and Catheter-Directed Intra-Arterial Vasodilators to SMA
- The Focus of Treatment Should be to Correct the Underlying Cause When Possible 10
- Vasodilators: Prostaglandin E1 (PGE1), Nitroglycerine, or Papaverine 26,27
Endovascular Treatment
- Generally Avoided in Acute Mesenteric Ischemia if There is Concern for Bowel Ischemia Requiring an Open Surgical Evaluation 28
- May Be Preferred if There Are No Signs of Bowel Necrosis and the Expertise is Available with No Contraindications – Evolving 28
- Decreased Morbidity and Mortality Over Open Surgery for Arterial Occlusive AMI 29
- Interventions:
- SMA Embolism:
- Embolectomy/Percutaneous Aspiration
- Thrombolysis
- SMA Thrombosis:
- Thrombectomy
- Thrombolysis
- Percutaneous Transluminal Angioplasty (PTA)
- Stenting
- SMA Embolism:
Surgical Technique
Exploratory Laparotomy
- Bowel Resection:
- Resect Areas of Gross Necrosis Before Embolectomy or Revascularization – Risk for Infection After Revascularization
- Reevaluate Areas of Partial Ischemia After Embolectomy or Revascularization – Preserve as Much Viable Bowel as Possible
- Massive Gut Necrosis May Be Best Managed By Comfort Care Measures and Evaluation of Underlying Comorbidities and Advanced Directives Should Be Considered Prior to Resection 10
- Low Threshold for Leaving an Open Abdomen and Second Look in 24-48 Hours to Reassess Bowel Viability if Questioned 30-32
Exposure of the SMA
- The SMA May or May Not Have a Palpable Pulse and May Be Difficult to Identify
- Anterior Approach:
- Retract the Transverse Colon Cephalad and the Small Bowel to the Right
- Palpate the SMA at the Root of the Transverse Colon Mesentery at the Inferior Margin of the Pancreas
- Carefully Dissect Down to Isolate the Artery
- Multiple Small Venous Branches from the SMV May Cross Over the SMA and Require Division (SMA Lies to the Left of the SMV)
- Lateral Approach:
- Take Down the Ligament of Treitz
- Retract the Entire Small Bowel to the Right
- Carefully Dissect Down to Isolate the Artery
SMA Embolectomy
- Expose the SMA – Through an Anterior Approach
- Obtain Proximal and Distal Control of the Artery
- Make a Proximal Transverse Arteriotomy
- Perform the Embolectomy Using a 3-4 mm Fogarty Balloon Catheter
- Insert Both Proximally and Distally to Extract Embolus
- Repeat Passage as Needed to Ensure All Clot is Removed
- Flush with Heparinized Saline
- Close Arteriotomy Primarily with 6-0 Prolene Sutures
- *Rarely May Consider Longitudinal Incision with Patch Angioplasty if Concerned for Small Caliber Vessel and Resulting Stricture
SMA Bypass
- General Technique:
- Expose the SMA – Through a Lateral Approach
- Expose the Inflow Site
- Anastomose the Bypass After Obtaining Proximal and Distal Control at Each Site Sequentially
- Cover the Graft with an Omental Buttress to Protect and Decrease the Risk of Kinking
- Inflow Bypass Route:
- Right Common Iliac Artery to SMA – The Preferred Route in Emergent Situations
- Retrograde in “Lazy-C” Configuration
- Avoids Aortic Cross Clamping and Provides Good Positioning with Minimal Kinking
- Other Retrograde Sources if Right Common Iliac is Diseased:
- Left Common Iliac Artery
- Infrarenal Aorta
- Antegrade Supraceliac Bypass
- Technically More Difficult Dissection and Increases the Physiologic Insult from Aortic Cross Clamping
- Only if Infrarenal Aorta and Iliacs are Diseased
- May Consider Bifurcated Prosthetic Conduit to Both the Celiac and SMA if Both are Diseased in Select Circumstances – More Often Used in a Chronic Mesenteric Ischemia
- Right Common Iliac Artery to SMA – The Preferred Route in Emergent Situations
- Graft Options:
- Synthetic Graft (Dacron) – Generally Preferred
- Benefits:
- Better Patency
- Better Size Match
- Easier Handling
- Kink Resistant
- Avoid Additional Time Required for Vein Harvesting
- Generally Avoided in the Setting of Bowel Necrosis or Perforation
- Benefits:
- Autogenous Vein
- Preferred if Bowel is Necrosed or with Peritoneal Spillage
- Requires a Vein of Suitable Size and Quality – Most Commonly the GSV
- Higher Risk of Kinking and Requires Extra Time for Harvesting
- Synthetic Graft (Dacron) – Generally Preferred

SMA Bypass with C-Loop Graft 33
References
- Zimmerman BJ, Granger DN. Reperfusion injury. Surg Clin North Am. 1992 Feb;72(1):65-83.
- Zimmerman BJ, Granger DN. Mechanisms of reperfusion injury. Am J Med Sci. 1994 Apr;307(4):284-92.
- van Petersen AS, Kolkman JJ, Meerwaldt R, Huisman AB, van der Palen J, Zeebregts CJ, Geelkerken RH. Mesenteric stenosis, collaterals, and compensatory blood flow. J Vasc Surg. 2014;60:111–119. doi: 10.1016/j.jvs.2014.01.063.
- Ottinger L.W.: The surgical management of acute occlusion of the superior mesenteric artery. Ann Surg 1978; 188: pp. 721-731.
- Ischemia of the gastrointestinal tract. Br Med J 1972; 4: pp. 566-567.
- Zettervall S.L., Lo R.C., Soden P.A., et. al.: Trends in treatment and mortality for mesenteric ischemia in the united states from 2000 to 2012. Ann Vasc Surg 2017; 42: pp. 111-119.
- Ryer E.J., Kalra M., Oderich G.S., et. al.: Revascularization for acute mesenteric ischemia. J Vasc Surg 2012; 55: pp. 1682-1689.
- Zachariah SK. Adult necrotizing enterocolitis and non occlusive mesenteric ischemia. J Emerg Trauma Shock. 2011 Jul;4(3):430-2. (License: CC BY-NC-SA 3.0)
- Gnanapandithan K, Feuerstadt P. Review Article: Mesenteric Ischemia. Curr Gastroenterol Rep. 2020 Mar 17;22(4):17.
- Bala M, Kashuk J, Moore EE, Kluger Y, Biffl W, Gomes CA, Ben-Ishay O, Rubinstein C, Balogh ZJ, Civil I, Coccolini F, Leppaniemi A, Peitzman A, Ansaloni L, Sugrue M, Sartelli M, Di Saverio S, Fraga GP, Catena F. Acute mesenteric ischemia: guidelines of the World Society of Emergency Surgery. World J Emerg Surg. 2017 Aug 7;12:38.
- Karkkainen JM, Acosta S. Acute mesenteric ischemia (part I) – incidence, etiologies, and how to improve early diagnosis. Best Pract Res Clin Gastroenterol. 2017;31(1):15–25.
- Bhagirath Desai A, Sandeep Shah D, Jagat Bhatt C, Umesh Vaishnav K, Salvi B. Measurement of the distance and angle between the aorta and superior mesenteric artery on CT scan: values in Indian population in different BMI categories. Indian J Surg. 2015;77(Suppl 2):614–7.
- Ozkurt H, Cenker MM, Bas N, Erturk SM, Basak M. Measurement of the distance and angle between the aorta and superior mesenteric artery: normal values in different BMI categories. Surg Radiol Anat. 2007;29(7):595–9.
- Acosta S, Ogren M, Sternby NH, Bergqvist D, Björck M. Clinical implications for the management of acute thromboembolic occlusion of the superior mesenteric artery: autopsy findings in 213 patients. Ann Surg. 2005;241:516–522.
- Kärkkäinen JM, Acosta S. Acute mesenteric ischemia (part I) -incidence, etiologies, and how to improve early diagnosis. Best Pract Res Clin Gastroenterol. 2017;31:15–25.
- Hmoud B, Singal AK, Kamath PS. Mesenteric venous thrombosis. J Clin Exp Hepatol. 2014;4(3):257–63.
- Clores MJ, Monzur F, Rajapakse R. Acute Mesenteric Ischemia Caused by Rare Cardiac Tumor Embolus. ACG Case Rep J. 2014 Oct 10;2(1):27-9. (License: CC BY-NC-ND 4.0)
- Reginelli A, Genovese E, Cappabianca S, Iacobellis F, Berritto D, Fonio P, Coppolino F, Grassi R. Intestinal Ischemia: US-CT findings correlations. Crit Ultrasound J. 2013 Jul 15;5 Suppl 1(Suppl 1):S7. (License: CC BY 2.0)
- Kim HM, Kim HL, Lee HS, Jung JH, Kim CH, Oh S, Kim JH, Zo JH. Nonbacterial Thrombotic Endocarditis in a Patient with Bowel Infarction due to Mesenteric Vein Thrombosis. Korean Circ J. 2014 May;44(3):189-92. (License: CC BY-NC 3.0)
- Baugh CW, Levine AC, Pallin DJ. Heart block and nonocclusive mesenteric ischemia. Int J Emerg Med. 2009 Sep;2(3):171-2. (License: CC BY-NC 2.0)
- Park WM, Gloviczki P, Cherry KJ, Jr, Hallett JW, Jr, Bower TC, Panneton JM, Schleck C, Ilstrup D, Harmsen WS, Noel AA. Contemporary management of acute mesenteric ischemia: Factors associated with survival. J Vasc Surg. 2002;35:445–452.
- Stone JR, Wilkins LR. Acute mesenteric ischemia. Tech Vasc Interv Radiol. 2015 Mar;18(1):24-30.
- Kougias P, Lau D, El Sayed HF, Zhou W, Huynh TT, Lin PH. Determinants of mortality and treatment outcome following surgical interventions for acutemesenteric ischemia. J Vasc Surg. 2007;46:467–474.
- Corcos O, Nuzzo A. Gastro-intestinalvascular emergencies. Best Pract Res Clin Gastroenterol. 2013;27:709–725. doi: 10.1016/j.bpg.2013.08.006.
- Acosta S. Surgical management of peritonitis secondary to acute superior mesenteric artery occlusion. World J Gastroenterol. 2014;20(29):9936–41.
- Trompeter M, Brazda T, Remy CT, Vestring T, Reimer P. Non-occlusive mesenteric ischemia: etiology, diagnosis, and interventional therapy. Eur Radiol. 2002;12(5):1179–87.
- Mitsuyoshi A, Obama K, Shinkura N, Ito T, Zaima M. Survival in nonocclusive mesenteric ischemia: early diagnosis by multidetector row computed tomography and early treatment with continuous intravenous high-dose prostaglandin E(1). Ann Surg. 2007;246(2):229–35.
- Karkkainen JM, Acosta S. Acute mesenteric ischemia (Part II) – vascular and endovascular surgical approaches. Best Pract Res Clin Gastroenterol. 2017;31(1):27–38.
- Salsano G, Salsano A, Sportelli E, Petrocelli F, Dahmane M, Spinella G, et al. What is the best revascularization strategy for acute occlusive arterial mesenteric ischemia: systematic review and meta-analysis. Cardiovasc Intervent Radiol. 2018;41(1):27–36.
- Freeman AJ, Graham JC. Damage control surgery and angiography in cases of acute mesenteric ischaemia. ANZ J Surg. 2005;75(5):308–14.
- Weber DG, Bendinelli C, Balogh ZJ. Damage control surgery for abdominal emergencies. Br J Surg. 2014;101(1):e109–18.
- Kaminsky O, Yampolski I, Aranovich D, Gnessin E, Greif F. Does a second-look operation improve survival in patients with peritonitis due to acute mesenteric ischemia? A five-year retrospective experience. World J Surg. 2005;29(5):645–8.
- Zia-ur-Rehman, Alvi AR, Sophie Z. Abdominal angina–a rare cause of chronic abdominal pain. J Coll Physicians Surg Pak. 2011 Jul;21(7):439-41. (License: Creative Commons – Unspecified)