Parathyroid Carcinoma
Parathyroid Carcinoma
Mitchell Temple, MD
Table of Contents
Background
A Rare Malignant Tumor of the Parathyroid Glands
Epidemiology
- Responsible for 1% of Primary Hyperparathyroidism (PHPT) Cases
- Affects Both Genders Equally
- Most Common in the Fifth Decade of Life
Etiology is Largely Idiopathic and Sporadic
Associated Familial Syndromes
- Multiple Endocrine Neoplasia (MEN) Syndromes
- Described in MEN I and MEN IIa
- *See Multiple Endocrine Neoplasia (MEN) Syndrome
- Hyperparathyroidism-Jaw Tumor Syndrome (HPT-JT) – Associated with Parathyroid Carcinoma and Fibro-Osseous Tumors of the Jaw
Radiation Exposure is a Potential Risk Factor
Parathyroid Carcinoma 1
Presentation and Diagnosis
Clinical Presentation
- Primary Hyperparathyroidism
- Most are Functional with Markedly Elevated Calcium and Parathyroid Hormone (PTH)
- Hypercalcemia Symptoms: Fatigue, Depression, Weakness, Bone Pain, Pathological Bone Fractures, Kidney Stones, and Gastrointestinal Upset
- Palpable Cervical Mass if Large – Many are Not Palpable and Found Incidentally
- Local Symptoms Including Compression from the Tumor or Evidence of Recurrent Laryngeal Nerve Paralysis
Diagnosis
- Often Diagnosed on Pathology After an Initial Surgery – Concern Raised if Adherent and Invading the Thyroid with No Clear Plane on Initial Surgery
- Labs Concerning for Malignancy:
- Serum Calcium > 14.0 mg/dL
- PTH > 3-10 x Normal Upper Limit
- Renal or Skeletal Abnormalities Combined with the Above
- Levels are Generally Significantly Higher than in Benign Causes of Hyperparathyroidism
- Imaging:
- Options: US, CT, MRI, and Sestamibi Scan
- Used to Localize an Abnormal Gland and May Demonstrate Suspicious Findings (Irregular and Fixed to Adjacent Tissue)
- FNA/Biopsy is Rarely Performed Due to Fear of Seeding the Tumor
- Definitive Diagnosis is Made by Histopathological Examination of the Excised Tumor
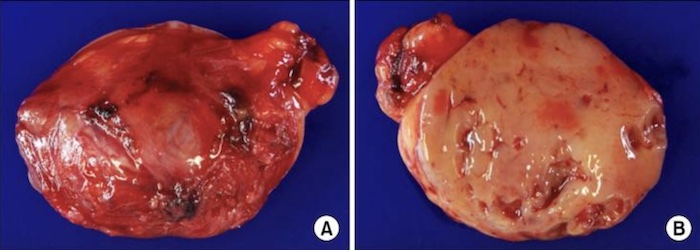
- Key Pathologic Features:
- Capsular Invasion, Vascular Invasion, or Metastases
- Cellular Atypia
- Fibrous Trabeculae
- Mitotic Figures
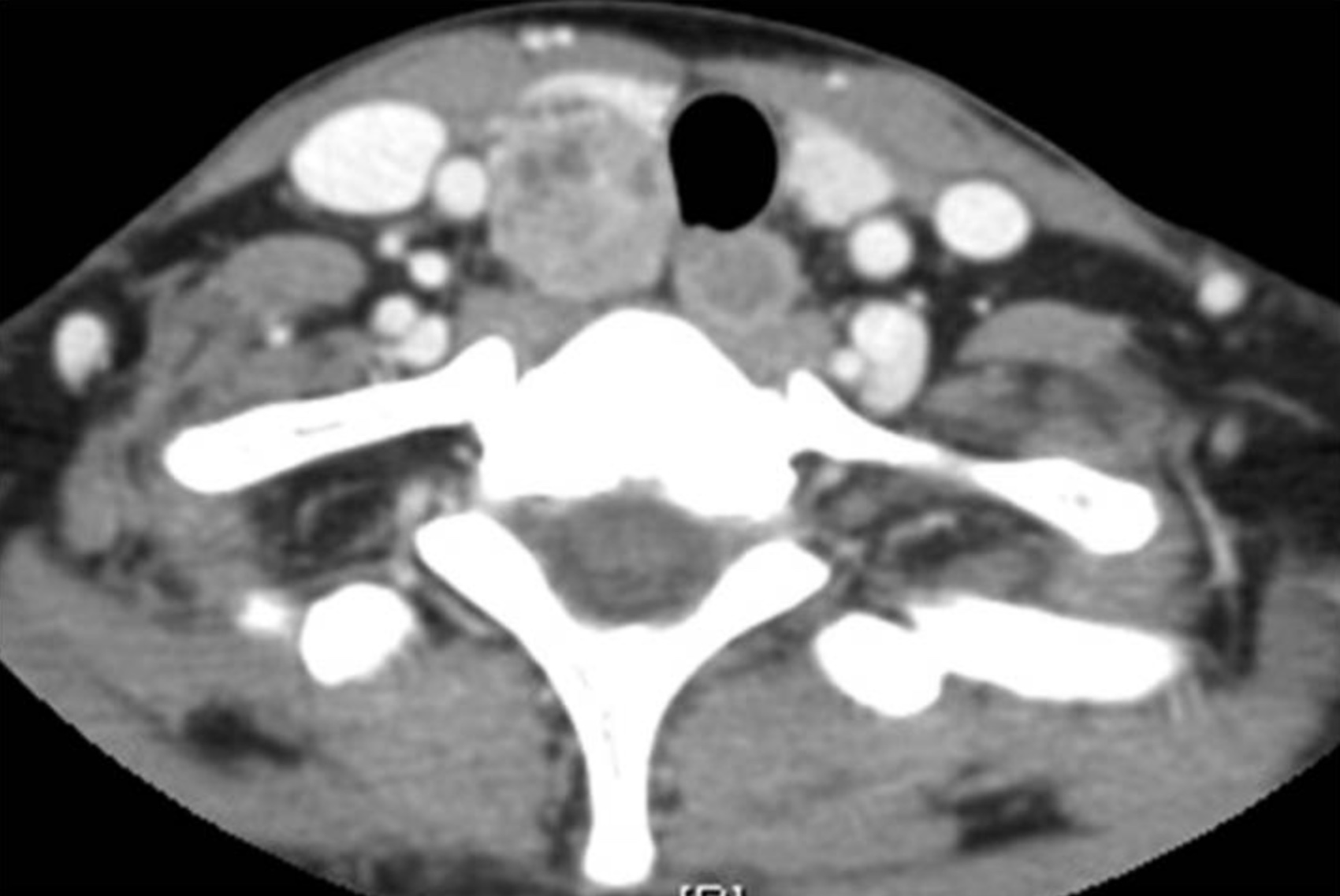
Parathyroid Carcinoma on CT 1
Treatment
Primary Treatment: Radical Parathyroidectomy (En Bloc Resection with Ipsilateral Thyroid Lobectomy)
- The Primary Treatment for Localized Disease
- Avoid Capsular Disruption to Avoid Tumor Seeding and Parathyromatosis
- May Require Recurrent Laryngeal Nerve Resection if Clearly Invading
- Consider Lymph Node Dissection if There is Concern for Nodal Involvement
- No Need for Prophylactic Central or Lateral Lymph Node Dissection – High Morbidity with Low Risk of Metastases
Risk for Hypocalcemia After Resection – May Require Calcium and Vitamin D Supplementation
Patients Require Lifelong Monitoring with Regular Serum Calcium, PTH, and Imaging to Detect Recurrence or Metastasis
Adjuvant and Palliative Therapy
- Consider Resection Even if Locoregional or Distant Metastases are Present and Resection Would Not Be Curative – Reducing Tumor Burden May Normalize Calcium and Provide Symptomatic Palliation
- Medical Management: Calcimimetics, Bisphosphonates, and Calcitonin May Be Used to Manage Hypercalcemia and Decrease Systemic Effects
- Radiotherapy: Reserved for Palliative Cases and Should Not Be Routinely Used Post-Operatively
- Chemotherapy: Not Generally Used and Considered Ineffective in Parathyroid Carcinoma
Prognosis
- 5-Year Survival: 85.5%
- Recurrence Rates Remain Elevated – About 50%
- Prognosis is Improved When the Tumor is Localized and Completely Resected Early
References
Cover: Nephron. Parathyroid Carcinoma. Wikimedia Commons. 2019. (License: CC BY-SA-4.0)
- Kim KM, Park JB, Bae KS, Kang SJ. Hungry bone syndrome after parathyroidectomy of a minimally invasive parathyroid carcinoma. J Korean Surg Soc. 2011 Nov;81(5):344-9. (License: CC BY-NC-3.0)
- Sippel R, Chen H. The Handbook of Endocrine Surgery. World Scientific; 2012.
- Byrd C, Kwartowitz G. Cancer, Parathyroid. Nih.gov. Published February 24, 2019.
- Wilhelm SM, Wang TS, Ruan DT, et al. The American Association of Endocrine Surgeons Guidelines for Definitive Management of Primary Hyperparathyroidism. JAMA Surgery. 2016;151(10):959.