Pilonidal Disease
Irving Samuel Lambert, MD
The Operative Review of Surgery. 2023; 1:204-208.
Table of Contents
Pathophysiology and Presentation
Also Called “Pilonidal Cyst”, “Sacrococcygeal Pilonidal Sinus Disease” (SPSD), “Jeep Seat”, or “Jeep Disease” (Due to Prevalence in Drivers During World War 2)
Definition
- Inflammatory Condition of the Skin and Subcutaneous Tissue of the Gluteal Cleft 1
- “Pilonidal Cyst” is a Misnomer – No Epithelial Lining (Not a True Cyst)
Pathophysiology
- Exact Mechanism is Not Clear
- An Acquired Collection of Hair and Skin Debris within a Pore or Pit (Previously Believed to be Due to a Congenital Abnormality) 2,3
Risk Factors 4-6
- Young Adults (Teens-20’s)
- Male Sex
- Caucasian
- Obesity
- Deep Gluteal Cleft – Facilitates Hair Entrapment
- Hirsute Body (Thick/Stiff Body Hairy)
- Prolonged Sitting (> 6 Hours)
- Local Trauma
Presentations 5-7
- Acute Presentation: Acute Cellulitis or Abscess
- Sudden Onset Intergluteal Pain and Swelling
- Mucous or Purulent Drainage
- Fever
- Chronic Presentation: Chronic Smoldering Disease
- Recurrent or Persistent Pain and Drainage
- One or More Pits/Sinus Tracts
- May See Shed Hair Protruding from Pits
- Can Develop Squamous Cell Carcinoma in Long Standing Untreated Disease 8

Pilonidal Cyst 9
Diagnosis
Diagnosis
- Clinical Diagnosis Based on History and Physical Exam
- May Consider MRI if Osteomyelitis is Suspected
- May Consider Biopsy if Concerned for Malignancy with an Atypical or Aggressive Appearance
Classification Systems
- Multiple Classification Systems Have Been Described but None Have Been Universally Accepted 10
- Tezel Classification 11
- Type I: Asymptomatic Sinus
- Type II: Acute Abscess
- Type III: Chronic Symptomatic Disease, Limited to the Navicular Area
- Type IV: Chronic Symptomatic Disease, Extending Beyond the Navicular Area
- Type V: Recurrent Disease
- Guner Classification 12
- Stage I: Single Pit in the Midline
- Stage II: Multiple Pits in the Midline
- IIa: 2-3 Pits
- IIb: > 3 Pits
- Stage III: Midline Pits with Lateral Extension in One Direction
- Stage IV: Midline Pits with Lateral Extension in Both Directions
- (Stage R: Recurrent PSD Following Any Treatment)
- Other Classification Systems:
- Chavoin Classification 13
- Doll Classification 14
- Irkorucu Classification 15
- Karkas Classification 16
- Lapsekili Classification 17
- Awad Classification 18
Treatment
Acute Disease
- Cellulitis: Antibiotics
- Abscess: Incision and Drainage (I&D)
- Incision Made Lateral to the Cleft Off Midline – Improved Healing
- Sinus Curettage or Tract Excision in Acute Disease is Not Successful 19,20
- Include Antibiotic Treatment if Diabetic, Immunocompromised, or Other Signs of Systemic Infection
- 60% Chance of Successful Healing 21
Chronic Disease
- Primary Management of Chronic Disease is by Surgical Excision 5,20
- Techniques:
- Complete Midline Excision of Pit and Sinus Tracts
- Tract Unroofing and Debridement without Pit Excision
- Pit Picking (Bascom’s Operation/Bascom I) – Pits are Excised Using 2-4 mm Biopsy Punches and then Trapped Hair Follicles are Removed Using Fine Clamps
- Smallest Intervention with Minimal Scarring
- Video-Assisted Sinus Ablation – An Evolving Minimally Invasive Approach 22
- Preferred Technique is Debated
- Preserve as Much Healthy Tissue as Possible
- Techniques:
- Nonoperative Managements: 20,23
- Meticulous Hair Control (Shaving, Laser Hair Removal, or Topical Depilatory Creams)
- Perineal Hygiene
Wound Closure After Surgical Excision 24
- Primary Wound Closure
- Approaches: Midline or Off-Midline
- Faster Healing (14.5 Days) and Return to Work (11.9 Days)
- Higher Recurrence Rates (8.7%)
- Delayed Wound Closure/Secondary Intention
- Approaches:
- Left Open
- Marsupialization – Suture Skin Margins to Presacral Fascia at the Edges
- Negative Pressure Wound Therapy (NPWT)
- Longer Healing (60.4 Days) and Return to Work (17.5 Days)
- Lower Recurrence Rates (5.3%)
- Approaches:
- Flap Closure
- Approaches:
- Rhomboid Flaps (Limberg, Dufourmentel, or Webster)
- Karydakis Flap
- Bascom’s Cleft Lip Procedure (Bascom II)
- V-Y Advancement Flap
- Z-Plasty
- Generally Reserved for Extensive Disease
- Decreases Tension to Facilitate Closure
- Approaches:
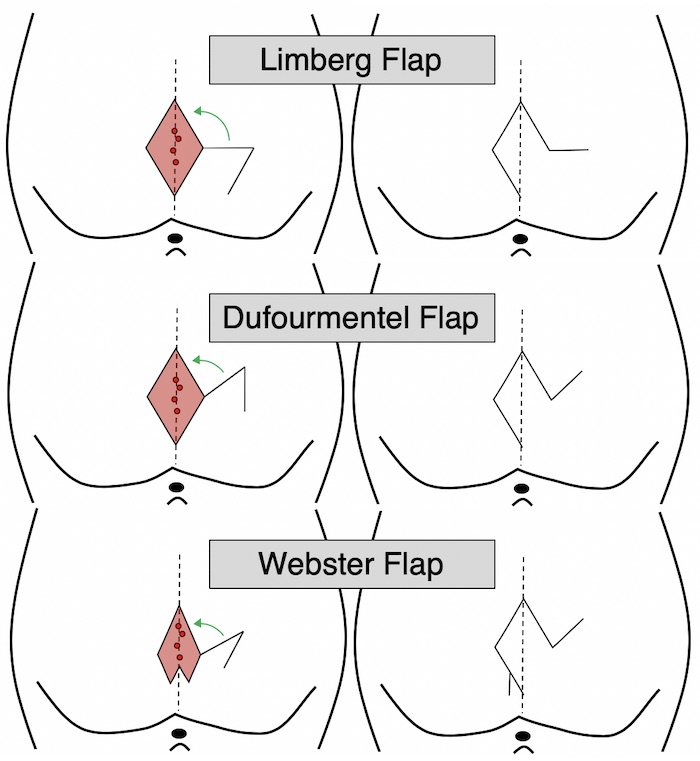
Rhomboid Flap Closure for Pilonidal Disease 25

Limberg Flap for Pilonidal Disease 26
References
- Pilonidal Disease. American Society of Colon and Rectal Surgeons (ASCRS).
- Classic articles in colonic and rectal surgery. Louis A. Buie, M.D. 1890-1975: Jeep disease (pilonidal disease of mechanized warfare). Dis Colon Rectum. 1982 May-Jun;25(4):384-90.
- DAVAGE ON. The origin of sacrococcygeal pilonidal sinuses based on an analysis of four hundred sixty-three cases. Am J Pathol. 1954 Nov-Dec;30(6):1191-205.
- Søndenaa K, Andersen E, Nesvik I, Søreide JA. Patient characteristics and symptoms in chronic pilonidal sinus disease. Int J Colorectal Dis. 1995;10(1):39-42.
- Khanna A, Rombeau JL. Pilonidal disease. Clin Colon Rectal Surg. 2011 Mar;24(1):46-53.
- Hull TL, Wu J. Pilonidal disease. Surg Clin North Am. 2002 Dec;82(6):1169-85.
- Jones DJ. ABC of colorectal diseases. Pilonidal sinus. BMJ. 1992 Aug 15;305(6850):410-2.
- de Bree E, Zoetmulder FA, Christodoulakis M, Aleman BM, Tsiftsis DD. Treatment of malignancy arising in pilonidal disease. Ann Surg Oncol. 2001 Jan-Feb;8(1):60-4.
- Giggs Hammouri. Wikimedia Commons. (License: CC BY 3.0)
- Beal EM, Lee MJ, Hind D, Wysocki AP, Yang F, Brown SR. A systematic review of classification systems for pilonidal sinus. Tech Coloproctol. 2019 May;23(5):435-443.
- Tezel E. A new classification according to navicular area concept for sacrococcygeal pilonidal disease. Colorectal Dis. 2007 Jul;9(6):575-6.
- Guner A, Cekic AB, Boz A, Turkyilmaz S, Kucuktulu U. A proposed staging system for chronic symptomatic pilonidal sinus disease and results in patients treated with stage-based approach. BMC Surg. 2016 Apr 16;16:18.
- Quinodoz PD, Chilcott M, Grolleau JL, Chavoin JP, Costagliola M. Surgical treatment of sacrococcygeal pilonidal sinus disease by excision and skin flaps: the Toulouse experience. Eur J Surg. 1999 Nov;165(11):1061-5.
- Doll D, Vassiliu P (2018) Another pilonidal classification—PLLATIN. Pilonidal Sinus J [Internet]. 4(1):1–3.
- Irkörücü O. Management for pilonidal disease: Before you compare, use a classification system. Asian J Surg. 2016 Oct;39(4):260-1.
- Karakaş DÖ, Yılmaz İ, Hazer B, Dandin Ö, Sücüllü İ, Sinüs P et al (2017) Congress of Turkish colon and rectal surgery on 19–23. Color Dis [Internet]. 27:65–6.
- Lapsekill E, Coskun M, Oztas M, Urkan M, Can MF (2013) A classification proposal for the sacrococcygeal pilonida1 sinus disease (SPSD). Eur Surg Res [Internet]. 50(SUPPL. 1):144.
- Awad MM, Elbaset AA, Ebraheem S, Tantawy E, Elhafez MA, Elsayed AM. A scoring system as a method to evaluate pilonidal sinus disease to make an easy decision for its management. Indian J Plast Surg. 2009 Jan-Jun;42(1):43-8.
- Matter I, Kunin J, Schein M, Eldar S. Total excision versus non-resectional methods in the treatment of acute and chronic pilonidal disease. Br J Surg. 1995 Jun;82(6):752-3.
- Humphries AE, Duncan JE. Evaluation and management of pilonidal disease. Surg Clin North Am. 2010 Feb;90(1):113-24.
- Jensen SL, Harling H. Prognosis after simple incision and drainage for a first-episode acute pilonidal abscess. Br J Surg. 1988 Jan;75(1):60-1.
- Velotti N, Manigrasso M, Di Lauro K, Araimo E, Calculli F, Vertaldi S, Anoldo P, Aprea G, Simone G, Vitiello A, Musella M, Milone M, De Palma GD, Milone F, Sosa Fernandez LM. Minimally Invasive Pilonidal Sinus Treatment: A Narrative Review. Open Med (Wars). 2019 Aug 7;14:532-536.
- Doll D, Friederichs J, Boulesteix AL, Düsel W, Fend F, Petersen S. Surgery for asymptomatic pilonidal sinus disease. Int J Colorectal Dis. 2008 Sep;23(9):839-44.
- Al-Khamis A, McCallum I, King PM, Bruce J. Healing by primary versus secondary intention after surgical treatment for pilonidal sinus. Cochrane Database Syst Rev. 2010 Jan 20;2010(1):CD006213.
- Lambert IS. Flap Closure for Pilonidal Disease. The Operative Review of Surgery. 2023.
- Bali İ, Aziret M, Sözen S, Emir S, Erdem H, Çetinkünar S, İrkörücü O. Effectiveness of Limberg and Karydakis flap in recurrent pilonidal sinus disease. Clinics (Sao Paulo). 2015 May;70(5):350-5. (License: CC BY-NC 3.0)