Cardiothoracic Surgery: Pulmonary Physiology
Lung Volumes
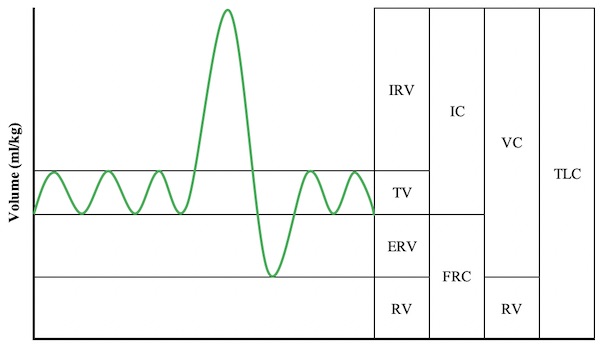
Lung Volumes
- Base Volumes:
- Tidal Volume (TV): Normal Breath
- Inspiratory Residual Volume (IRV): Maximum Extra Inhaled
- Expiratory Reserve Volume (ERV): Maximum Extra Exhaled
- Residual Volume (RV): Volume Unable to Exhale
- Other Volumes: Mn
- Inspiratory Capacity (IC) = TV + IRV
- Functional Residual Capacity (FRC) = ERV + RV
- Increase: PEEP
- Decrease: Surgery, ARDS, Trauma
- Vital Capacity (VC) = TV + IRV + ERV = TLC – RV
- Aka Functional Vital Capacity (FVC)
- Total Lung Capacity (TLC) = VC + RV
Factors that Effect
- Compliance: Volume Produced by a Unit of Pressure Change
- Elastic Recoil: Ability to Rebound After Inhalation
Muscles of Respiration
- Inspiration – Elevates Ribs & Sternum
- Diaphragm (80% of Normal)
- Accessory Muscles: (20% of Normal)
- External Intercostals
- *May Be Considered a Primary Muscle of Inspiration Depending on the Source
- SCM
- Scalenes (Anterior, Middle & Posterior)
- Serratus Anterior & Posterior
- Levators
- External Intercostals
- Expiration – Depresses Ribs & Sternum
- Mostly Passive Due to Elastic Recoil
- Forceful Expiration:
- Internal Intercostals
- Innermost Intercostals
- Subcostalis Muscle
- Abdominal Muscles (Rectus Abdominis, Transverse Abdominis, External Oblique & Internal Oblique)
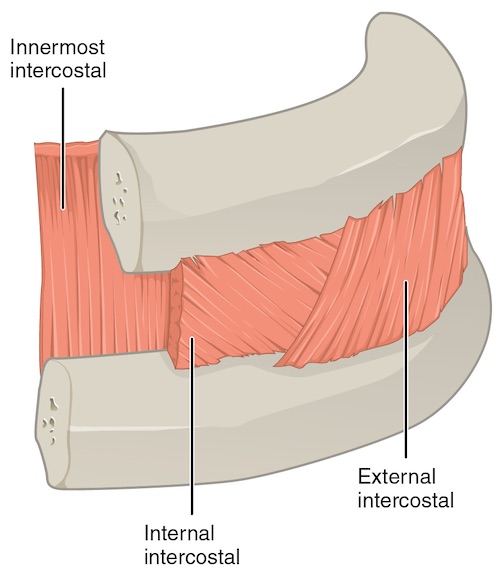
Intercostal Muscles 1
Disease Changes
- Obstructive Lung Disease
- Decreased: Low FEV1 & FEV1/FVC Ratio
- *FEV1 = Forced Expiratory Volume in 1 Second
- Increased: TLC & RV
- Prolonged Expiratory Phase
- Decreased: Low FEV1 & FEV1/FVC Ratio
- Restrictive Lung Disease
- Decreased: TLC, RV & FVC
Gas Exchange
Pulmonary Physiology
- Develops From 7 Months Gestation to 10 Years Old
- Pneumocytes
- Type I: Gas Exchange
- Type II: Produce Phosphatidylcholine/Surfactant
- Lowers Surface Tension & Keeps Alveoli Open
- Collateral Ventilation:
- Pores of Kohn: Direct Air Exchange Between Alveoli
- Channels of Lambert: Air Exchange from Bronchiole to Alveolus
- Channels of Martin: Air Exchange Between Bronchioles
- Partial Pressure of Oxygen
- Highest Point: Pulmonary Capillaries
- Slightly Less by the Time Blood Reaches the Atrium
- Lowest Point: Coronary Veins
- Highest Point: Pulmonary Capillaries
Ventilation/Perfusion
- Dead Space: Area Ventilated but Not Perfused
- Causes Increased PCO2
- Most Common Cause: Excessive PEEP (Induces Capillary Compression)
- Shunt: Area Perfused but Not Ventilated
- Causes Decreased PO2
- Most Common Cause: Atelectasis
Ventilation/Perfusion (V/Q) Ratio
- Causes of High V/Q Ratios:
- Dead Space
- Normal Lung Apex
- COPD
- Pulmonary Embolism
- Causes of Low V/Q Ratios:
- Shunting
- Normal Lung Base
- Asthma
- Pulmonary Edema
- Ratio Changes with Body Positioning
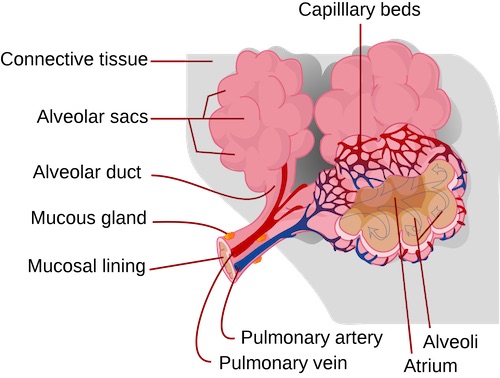
Pulmonary Alveoli 2
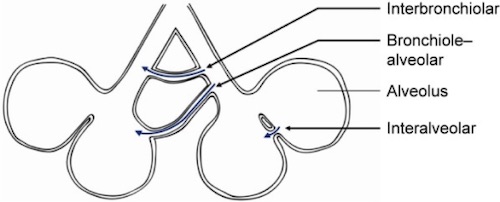
Collateral Ventilation 3
Pleural Fluid
Function
- Serous Fluid
- Acts as a Lubricant for Parietal & Visceral Pleura to Prevent Adhesion During Respiration
Flow
- Production: Parietal Circulation (Intercostal Arteries) from Bulk Flow
- Reabsorption: Lymphatic System
- Mostly (75%) from Lymphatics of the Parietal Pleura
- Visceral Pleural Plays No Significant Role in Drainage
Volume
- Normal Amount Present: 10-20 cc
- Fluid Turnover Ability: 1-2 L/Day
- Can Increase Up to 40x Normal Rates
- *Requires a Profound Increase in Production or Blockage of Lymphatics to Initiate Fluid Accumulation
Mnemonics
Capacities vs Residual Volumes
- C-C: Capacity = Combination of Others
References
- CF CF. Wikimedia Commons. (License: CC BY-SA-4.0)
- Lady of Hats. Wikimedia Commons. (License: Public Domain)
- Koster TD, Slebos DJ. The fissure: interlobar collateral ventilation and implications for endoscopic therapy in emphysema. Int J Chron Obstruct Pulmon Dis. 2016 Apr 13;11:765-73.(License: CC BY-NC-3.0)