Anorectal: Rectal Cancer
Rectal Cancer
Colorectal Polyp Work-Up
- *See Large Intestine: Colon Polyps
- Staging: MRI or Endoscopic US (EUS)
- Comparison:
- EUS is More Accurate at Defining T-Stage (Decreases with Higher Staging)
- MRI Better Defines the Extent of Mesorectal Fascia Involvement & Radial Margin of Larger Tumors
- CT for Distant Mets but Not Sufficient for T/N Status
- Comparison:
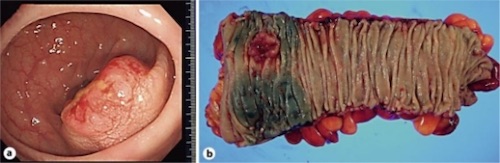
Rectal Cancer 1
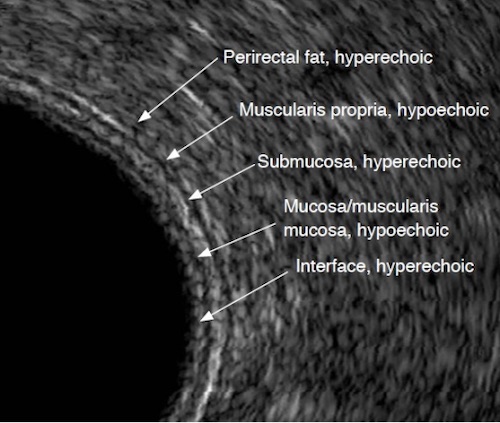
Rectal EUS – Layers 2
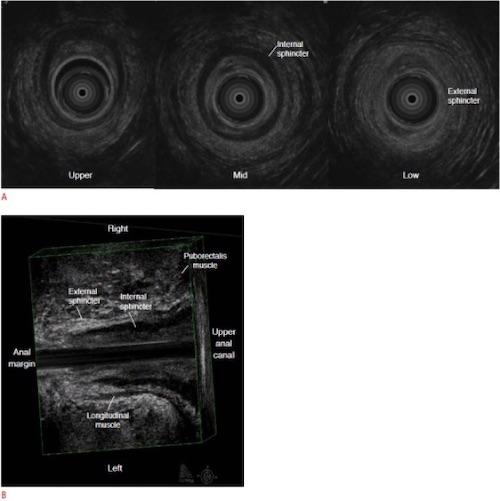
Rectal EUS – Sphincters 2
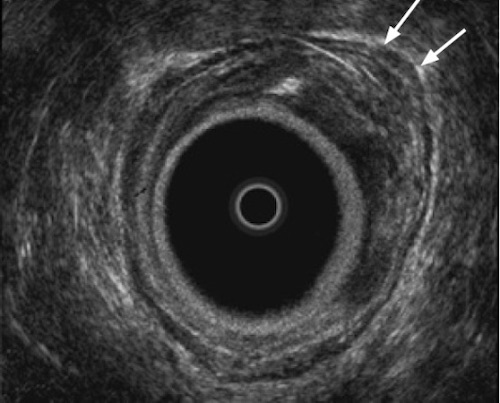
Rectal Cancer on EUS 2
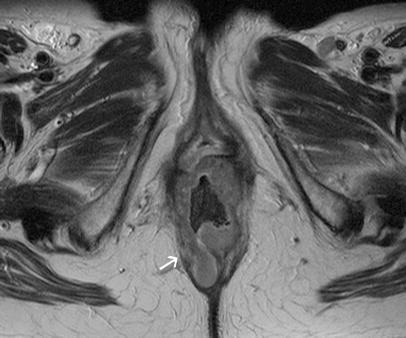
Rectal Cancer on MRI 3
TNM Staging
- Comparison:
- Rectal Cancer Same as Colon
- Anal Cancer Different
- TNM
| T | N | M | |
| 1 | Submucosa | 1a – 1
1b – 2-3 1c – Discrete Tumor Nodules in Lymph Drainage Area without Identifiable Lymph Node Tissue |
1a – One Distant Organ
1b – ≥ 2 Distant Organs 1c – Peritoneal Mets |
| 2 | Into Muscularis Propria | 2a – 4-6 LN
2b – ≥ 7 LN |
|
| 3 | Into Serosa | ||
| 4 | 4a – Through Serosa
4b – Into Adjacent Tissue/Organs |
- Staging
| T | N | M | ||
| I | T1-2 | N0 | M0 | |
| II | A | T3 | N0 | M0 |
| B | T4a | N0 | M0 | |
| C | T4b | N0 | M0 | |
| III | A | T1 | N1-2a | M0 |
| T2 | N1 | M0 | ||
| B | T1 | N2b | M0 | |
| T2 | N2 | M0 | ||
| T3 | N1-N2a | M0 | ||
| T4a | N1 | M0 | ||
| C | T3 | N2b | M0 | |
| T4a | N2 | M0 | ||
| T4b | N1-2 | M0 | ||
| IV | A | Any T | Any N | M1a |
| B | Any T | Any N | M1b | |
| C | Any T | Any N | M1c | |
Rectal Cancer – Treatment
Treatment
- Primary Tx: Surgical Resection
- May Consider Wide Local Excision (WLE) if All Criteria Are Met
Transanal/Endoscopic WLE
- Indication Criteria (Lowest Risk of LN Mets):
- T1
- < 3 cm
- < 30% Circumference
- < 8 cm from Verge
- Mobile
- No Lymphatic Invasion
- No Mucin Production
- Considerations:
- Position Patient So that the Lesion in Lying Dependent
- Full-Thickness
- Goal Margin: 10 mm
- Does Not Include a Lymphadenectomy
- Higher Local Recurrence Rates than Transabdominal Resection
Resection
- Procedure:
- *See Anorectal: Proctectomy
- Upper-Mid Rectum: Low Anterior Resection (LAR)
- Preserves Sphincter
- Low Rectum: Abdominoperineal Resection (APR)
- Loss of Sphincter Requiring Permanent Colostomy
- Concepts:
- Ensure a Total Mesorectal Excision (TME)
- Margins:
- Proximal: 5 cm
- Distal: 1-2 cm
- *Historically Required 5 cm Margins for LAR
- APR If Unable to Achieve Margins
- Goal LN: 12
Neoadjuvant Therapy
- Neoadjuvant Chemotherapy & Radiation
- Chemo Regimens: 5-FU, FOLFOX or CAPEOX
- Indications: Stage ≥ II (T3 or N+)
- Resection Timing: After 2-3 Months
- Goals:
- If Stage II/III – Attempt Preserve Sphincter Function
- If Stage IV – Attempt for APR Instead of Only Colostomy
Adjuvant Therapy
- Adjuvant Chemo:
- Chemo Regimens: 5-FU, FOLFOX or CAPEOX
- Indications:
- T3 if Threatened Circumferential Resection Margin
- T4
- N+
- Adjuvant XRT: Never Indicated
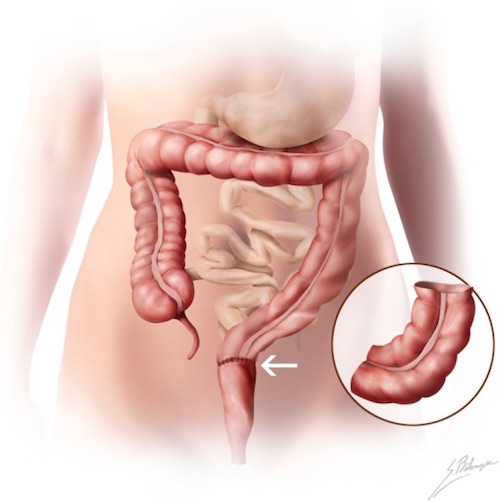
LAR 4
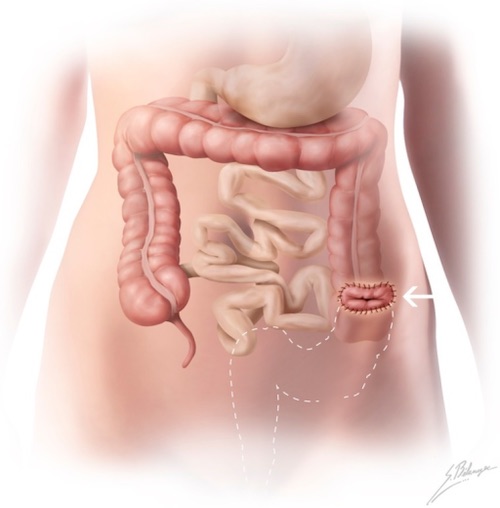
APR 4
References
- Tsukada T, Nakano T, Matoba M, Sasaki S, Higashi K. False-Positive Mediastinal Lymphadenopathy on 18F-Fluorodeoxyglucose Positron Emission Tomography and Computed Tomography after Rectal Cancer Resection: A Case Report of Thoracoscopic Surgery in the Prone Position. Case Rep Oncol. 2011 Sep;4(3):569-75. (License: CC BY-NC-ND-3.0)
- Kim MJ. Transrectal ultrasonography of anorectal diseases: advantages and disadvantages. Ultrasonography. 2015 Jan;34(1):19-31. (License: CC BY-NC-3.0)
- Klessen C, Rogalla P, Taupitz M. Local staging of rectal cancer: the current role of MRI. Eur Radiol. 2007 Feb;17(2):379-89. (License: CC BY-NC-2.0)
- Terrone DG, Lepanto L, Billiard JS, Olivié D, Murphy-Lavallée J, Vandenbroucke F, Tang A. A primer to common major gastrointestinal post-surgical anatomy on CT-a pictorial review. Insights Imaging. 2011 Dec;2(6):631-638. (License: CC BY-2.0)