Small Bowel Obstruction (SBO)
Bruce T. Noble, MD
The Operative Review of Surgery. 2023; 1:274-282.
Table of Contents
Definitions and Classification
Definitions
- Small Bowel Obstruction (SBO): Interruption of the Normal Flow of Intraluminal Contents
- Functional SBO: Obstruction Due to Dysfunctional Peristalsis – Also Referred to as an “Ileus”
- Mechanical SBO: Obstruction Due to Intraluminal or Extraluminal Compression
- In Practice, The Term “Small Bowel Obstruction” Typically Refers to a “Mechanical Small Bowel Obstruction”
Classification
- Partial SBO: Some Gas or Liquid Stool is Able to Pass the Obstruction
- Complete SBO: Nothing is Able to Pass the Site of Obstruction
- Closed Loop Obstruction: Both the Proximal and Distal Ends are Obstructed
- No Outlets are Available for Decompression
- Rapid Progression with High Risk for Strangulation and Perforation
Grading
- Low-Grade SBO: Generally Describes Partial SBO without a Discrete Transition Point
- High-Grade SBO: Generally Describes Complete SBO with a Discrete Transition Point
- *Definitions are Varied
AAST Grade 1
- Grade I: Partial SBO
- Grade II: Complete SBO; Bowel Viable and Not Compromised
- Grade III: Complete SBO; Bowel Viable but Compromised
- Grade IV: Complete SBO; Bowel Nonviable or Perforation with Local Spillage
- Grade V: SBO with Perforation and Diffuse Peritoneal Contamination
Etiology and Presentation
Common Causes (90%) 3-4 Mn
- Postoperative Adhesions
- Most Common Cause in United States (> 70%)
- Abdominal Wall Hernia
- Most Common Cause in “Virgin Abdomens” (No Past Surgery)
- Most Common Cause Worldwide
- Neoplasm/Cancer
- Most Common Cause of Large Intestine Obstruction (Regardless of Surgical History)
- Intussusception
- Midgut Volvulus
- Risk Factors for “Primary Volvulus”: Long Mesentery, Deficient Mesenteric Fat, or Narrow Mesenteric Base 10
- “Secondary Volvulus” is More Common (Due to Other Pathology Such as Adhesions or Malrotation)
- Stricture
- Sclerosing Encapsulating Peritonitis (SEP)/Chronic Fibrosa Incapsulata
- Inflammatory Bowel Disease (Crohn’s Disease or Ulcerative Colitis)
- Abscess
- Endometriosis
- Pelvic Inflammatory Disease
- Internal Hernia
- Meckel’s Diverticulum
- Gallstone Ileus
- Bezoar
- Foreign Body
- Fecalith
- Tuberculosis
- Parasites
- Nausea and Vomiting
- More Severe with Proximal Obstructions than Distal Obstructions
- Risk for Aspiration
- Abdominal Pain
- Starts as Intermittent Periumbilical Cramping
- Pain Becomes Constant and Sharp as the Bowel Dilates and Intraluminal Pressure Exceeds Capillary Pressure Causing Wall Ischemia and Peritonitis
- Abdominal Distention
- Obstipation (Unable to Pass Flatus or Stool)
- Presentation is Generally Similar to an Ileus
- *Colon Obstruction More Often Has Constant Pain with Feculent Emesis and More Significant Distention
Diagnosis
Diagnosis 11-15
- Diagnosis is Generally Made by Abdominal Imaging
- Computed Tomography (CT)
- Generally the Preferred Diagnostic Study
- Greater Sensitivity than Plain Films (91% vs 67%)
- Better at Characterizing the Obstruction and Evaluating for Bowel Compromise
- Abdominal Plain Film
- Preferred Initial Testing is Controversial – Although Some Recommend Starting with an Abdominal Plain Film and then Proceeding with CT, Plain Film is Inferior in Evaluating for Mechanical Obstruction and CT is Often Preferred
- Abdominal Ultrasound (US)
- Use is Evolving and Sensitivity/Specificity are Often Comparable to CT
- Benefit of Being Able to Visualize Peristalsis in Vivo
General Radiographic Findings
- Proximal Dilated Loops (> 3 cm) and Distal Decompressed Loops
- Air-Fluid Levels
- Air from Swallowed Nitrogen
- “Gasless Abdomen” without Air-Fluid Levels Can Be Seen When Obstruction Causes Fluid Sequestration
- Paucity of Gas in the Colon
- Transition Point
- “Swirling” of Mesentery Suggests a Closed-Loop Obstruction
Radiographic Findings that Predict the Need for Operative Exploration 16,17
- Absence of Fecalization of the Small Bowel – Fecalization is an Abnormal Sign But is a Reassuring Finding in the Setting of SBO (Indicates that the Obstruction has Been Present Long Enough for the Stasis to Allow Fecalization to Occur)
- Mesenteric Edema
- Bowel Wall Thickening
- Free Intraperitoneal Fluid
Small-Bowel Follow Through (SBFT) 18-20
- Procedure: Patient is Given Oral Water-Soluble Contrast (Gastrografin) and Sequential Plain Films are Taken After a Period of Time
- Imaging May Be Done at Periodic Intervals or a Single Image After a Few Hours
- Generally No Benefit Extending Past 8 Hours
- “Pass” if Patient Has a Bowel Movement or if Contrast is Seen in the Colon
- Provides Functional Information on How Contrast Passes Through the Bowel
- Should Not Be Used as the Primary Diagnostic Imaging Test
- Bowel Must First Be Decompressed and Not Actively Vomiting
- Helps Identify Patients Unlikely to Resolve by Nonoperative Management
- May Also Be Therapeutic as a Cathartic Agent – Hyperosmolar Agent to Reduce Bowel Edema and Acts as a Laxative
- Use of SBFT Decreases the Time to Nonoperative Resolution and Decreases Time to Identifying the Need for Surgical Intervention
Enteroclysis 21-23
- Procedure: An Enteroclysis Catheter is Advanced into the Proximal Small Bowel (Duodenum or Proximal Jejunum) and Barium is Injected into the Bowel
- Plain Film Imaging is Then Done at Periodic Intervals to Evaluate Passage of Contrast Through the Bowel (Similar to SBFT)
- Alternatively, CT Enteroclysis (CTE) Can Be Performed Once
- Enteroclysis is Superior to SBFT in Detecting Certain Small Bowel Pathology but it is More Invasive with Drawbacks Preventing More Universal Use
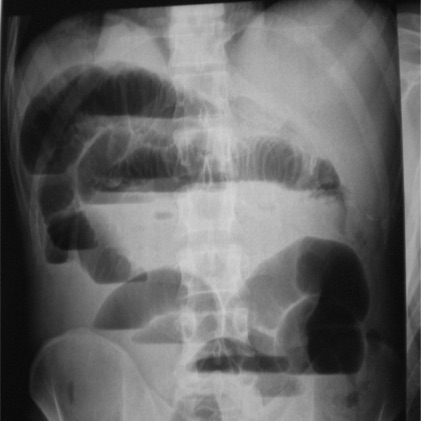
SBO on Abdominal Plain Film 24
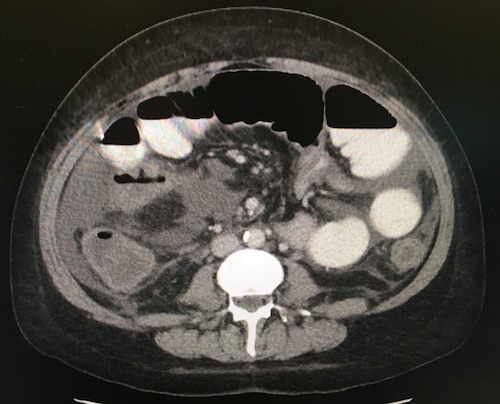
SBO on CT 24
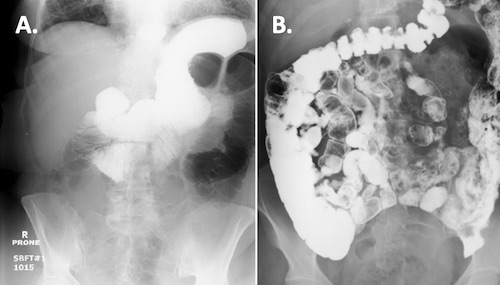
SBFT: A. Failed Progression, B. Passed with Contrast in the Colon 25,26
Treatment
Initial Management
- Most Initially Trial Nonoperative Management
- Term “Conservative Management” is Generally Considered Incorrect
- Indications for Urgent Surgery:
- Closed Loop Obstruction
- Peritonitis
- Bowel Ischemia or Strangulation
- Perforation
- Known Etiology that Will Not Resolve without Surgery
- Multiple Recurrence
- *Historically Stated that All “Virgin Abdomens” (No Surgical History) with SBO Should Undergo Surgery Due to the Risk of Malignancy – “Never Let the Sun Rise or Set on a Bowel Obstruction”. This Concept Has Since Fallen Out of Favor – Improved CT Scans Allow for Better Recognition of Malignancy and Many Have Other Reasons for Scar Tissue that May Have Been Unrecognized. 27
Nonoperative Management
- Managements:
- Bowel Rest/NPO
- Goal-Directed IV Fluids
- Nasogastric (NG) Tube for Decompression
- SBFT Once Bowel Has Been Decompressed and Not Actively Vomiting – Decreased Time to Nonoperative Resolution and Decreased Time to Identifying the Need for Surgical Intervention 23,24
- Failure Duration Prior to Proceeding with Surgery: 3-5 Days (Debated)
- Outcomes:
- Success for Adhesive SBO Resolution: 65-80%
- Recurrence Rate for Adhesive SBO: 16-53%
- Overall, Adhesive SBO Treated Nonoperatively Has Higher Recurrence Rates and Shorter Time to Recurrence than Those Managed Operatively 3,28,29
Admitting Service
- Patients Admitted to a Surgical Service (Opposed to a Medical Service) Have Better Outcomes 30-35
- Shorter Length of Stay
- Shorter Time to Surgery
- Lower Hospital Costs
- Lower Rate of Readmission
- Lower Mortality
Palliative Managements for Malignant Obstruction
- Consider a Palliative Enteric Bypass if the Mass is Large and Unresectable
- Consider a Decompressive Gastrostomy if There are Multiple Points of Obstruction
- Octreotide Can Assist as a Palliative Treatment for Nausea and Vomiting due to Malignant Obstruction
Surgical Intervention (Adhesiolysis)
Surgical Approach
- Open Laparotomy Generally Preferred Over Laparoscopy
- Potential Laparoscopic Indications:
- Mild Abdominal Distention (Bowel Diameter ≤ 4 cm and Early Presentation)
- Partial Obstruction
- Proximal Obstruction
- Few Operative Procedures
Adhesiolysis Technique
- Run Bowel from the Ligament of Treitz to the Ileocecal Valve
- Lysis of Adhesion (Enterolysis)
- Address Principal Site of Obstruction and Major Adhesions
- Total Lysis of All Adhesions is Unnecessary and Risks Damage to Healthy Bowel
- Reduce and Repair Any Hernias
- Resect Nonviable Bowel
- Consider Leaving an Open Abdomen with Planned Reexploration in 24-48 Horus if Viability is Uncertain
- Preform an Oncologic Resection for Any Mass (5-10 cm Margin with Associated Lymph Nodes)
Surgical Management of Strictures
- Single Stricture: Stricturoplasty
- Multiple Strictures: Bowel Resection
- Large Intestine Structure: Bowel Resection
- High Risk of Malignancy
Surgical Management of Injuries/Perforations
- Serosal Injuries: Oversew to Imbricate Mucosa
- Circumference < 50%: Primary Repair
- Circumference > 50%: Bowel Resection
Manual Bowel Decompression (“Milking”)
- Consider “Milking” Dilated and Distended Bowel
- Either Proximally to Be Decompressed Through a Nasogastric (NG) Tube or Distally into the Colon and Rectum
- Debated Effects 36-38
- Decompresses the Abdominal Compartment with Less Tension for Closure
- May Reduce Risk for Aspiration Pneumonia
- May Induce a Paralytic Ileus Although Transit Time is Generally Not Affected
- Proposed Concern for Possible Bacterial Translocation and Peritoneal Contamination
Mnemonics
General Causes of SBO
- “SHAVING”
- S: Stricture
- H: Hernia
- A: Adhesions
- V: Volvulus
- I: Intussusception or IBD
- N: Neoplasia
- G: Gallstone Ileus
References
- Hernandez MC, Haddad NN, Cullinane DC, Yeh DD, Wydo S, Inaba K, Duane TM, Pakula A, Skinner R, Rodriguez CJ, Dunn J, Sams VG, Zielinski MD, Choudhry A, Turay D, Yune JM, Watras J, Widom KA, Cull J, Toschlog EA, Graybill JC; EAST SBO Workgroup. The American Association for the Surgery of Trauma Severity Grade is valid and generalizable in adhesive small bowel obstruction. J Trauma Acute Care Surg. 2018 Feb;84(2):372-378.
- Miller G, Boman J, Shrier I, Gordon PH. Etiology of small bowel obstruction. Am J Surg. 2000 Jul;180(1):33-6.
- Bower KL, Lollar DI, Williams SL, Adkins FC, Luyimbazi DT, Bower CE. Small Bowel Obstruction. Surg Clin North Am. 2018 Oct;98(5):945-971.
- Baker S, Miller-Hammond K, King-Mullins E. Small Bowel Obstruction in the Virgin Abdomen. Surg Clin North Am. 2021 Dec;101(6):1045-1052.
- Lau WLJ, Aung L. Rare cause of small bowel intestinal obstruction. ANZ J Surg. 2020 Nov;90(11):E125-E126.
- Lamyman MJ, Noble DJ, Narang S, Dehalvi N. Small bowel obstruction secondary to intestinal schistosomiasis. Trans R Soc Trop Med Hyg. 2006 Sep;100(9):885-7.
- Al Samaraee A, Bhattacharya V. Facing the unexpected: unusual causes of mechanical small bowel obstruction in adults. Clin J Gastroenterol. 2021 Oct;14(5):1287-1302.
- Lai WC, Tay SP. Small bowel obstruction secondary to crab shell bezoar: A case report. Med J Malaysia. 2022 Mar;77(2):252-254.
- Ploneda-Valencia CF, Gallo-Morales M, Rinchon C, Navarro-Muñiz E, Bautista-López CA, de la Cerda-Trujillo LF, Rea-Azpeitia LA, López-Lizarraga CR. Gallstone ileus: An overview of the literature. Rev Gastroenterol Mex. 2017 Jul-Sep;82(3):248-254.
- Papadimitriou G, Marinis A, Papakonstantinou A. Primary midgut volvulus in adults: report of two cases and review of the literature. J Gastrointest Surg. 2011 Oct;15(10):1889-92.
- Li Z, Zhang L, Liu X, Yuan F, Song B. Diagnostic utility of CT for small bowel obstruction: Systematic review and meta-analysis. PLoS One. 2019 Dec 30;14(12):e0226740.
- Gottlieb M, Peksa GD, Pandurangadu AV, Nakitende D, Takhar S, Seethala RR. Utilization of ultrasound for the evaluation of small bowel obstruction: A systematic review and meta-analysis. Am J Emerg Med. 2018 Feb;36(2):234-242.
- Taylor MR, Lalani N. Adult small bowel obstruction. Acad Emerg Med. 2013 Jun;20(6):528-44.
- Hollerweger A, Wüstner M, Dirks K. Bowel Obstruction: Sonographic Evaluation. Ultraschall Med. 2015 Jun;36(3):216-35; quiz 236-8.
- Seitz K. Ultrasound First. Dtsch Arztebl Int. 2018 Jan 8;115(1-02):8-9.
- Zielinski MD, Eiken PW, Bannon MP, Heller SF, Lohse CM, Huebner M, Sarr MG. Small bowel obstruction-who needs an operation? A multivariate prediction model. World J Surg. 2010 May;34(5):910-9.
- Zielinski MD, Eiken PW, Heller SF, Lohse CM, Huebner M, Sarr MG, Bannon MP. Prospective, observational validation of a multivariate small-bowel obstruction model to predict the need for operative intervention. J Am Coll Surg. 2011 Jun;212(6):1068-76.
- Ellis PK, Mills JO. Small bowel follow-through. Clin Radiol. 1995 Jan;50(1):67-8.
- Licata A, El Moudden I, Bandy N, Sternick M, Britt R. Diatrizoate (Gastrograffin®) Small Bowel Follow Through for Small Bowel Obstructions: Timing and Outcomes. Am Surg. 2022 Apr;88(4):722-727.
- Galardi N, Collins J, Friend K. Use of early gastrografin small bowel follow-through in small bowel obstruction management. Am Surg. 2013 Aug;79(8):794-6.
- Kohli MD, Maglinte DD. CT enteroclysis in incomplete small bowel obstruction. Abdom Imaging. 2009 May-Jun;34(3):321-7.
- Maglinte DD, Peterson LA, Vahey TN, Miller RE, Chernish SM. Enteroclysis in partial small bowel obstruction. Am J Surg. 1984 Mar;147(3):325-9.
- Maglinte DD, Sandrasegaran K, Lappas JC, Chiorean M. CT Enteroclysis. Radiology. 2007 Dec;245(3):661-71.
- Polat C, Aktepe F, Turel S, Yazicioglu B, Ozkececi T, Arikan Y. A giant mesenteric fibromatosis case presenting with mechanical intestinal obstruction and successfully resected with partial duodeno-jejunectomy and right hemicolectomy. Clinics (Sao Paulo). 2010;65(1):110-3. (License: CC BY 4.0)
- Zakaria A, Al Share B, Turk I, Ahsan S, Farra W. An Uncommon Cause of a Small-Bowel Obstruction. Case Rep Gastrointest Med. 2017;2017:1628215. (License: CC BY 4.0)
- Estridge P, Akoh JA. Recurrent spontaneous pneumoperitoneum: A surgical dilemma. Int J Surg Case Rep. 2017;30:103-105. (License: CC BY-NC-ND 4.0)
- Diaz A, Ricci KB, Rushing AP, Ingraham AM, Daniel VT, Paredes AZ, Baselice HE, Oslock WM, Heh V, Strassels SA, Santry HP. Re-examining “Never Letting the Sun Rise or Set on a Bowel Obstruction” in the Era of Acute Care Surgery. J Gastrointest Surg. 2021 Feb;25(2):512-522.
- Meier R.P., de Saussure W.O., Orci L.A., et. al.: Clinical outcome in acute small bowel obstruction after surgical or conservative management. World J Surg 2014; 38: pp. 3082-3088.
- Williams S.B., Greenspon J., Young H.A., et. al.: Small bowel obstruction: conservative vs. surgical management. Dis Colon Rectum 2005; 48: pp. 1140-1146.
- Thacker C, Lauer C, Nealon K, Walker C, Factor M. Admitting Service and Outcome for Small Bowel Obstruction. Am Surg. 2022 Apr;88(4):643-647.
- Schwab DP, Blackhurst DW, Sticca RP. Operative acute small bowel obstruction: admitting service impacts outcome. Am Surg. 2001 Nov;67(11):1034-8; discussion 1038-40.
- Thacker C, Lauer C, Nealon K, Wang S, Factor M. Should Surgical Services Admit Small Bowel Obstructions Managed Non-operatively? Am Surg. 2022 Aug;88(8):1845-1848.
- Malangoni MA, Times ML, Kozik D, Merlino JI. Admitting service influences the outcomes of patients with small bowel obstruction. Surgery. 2001 Oct;130(4):706-11; discussion 711-3.
- Oyasiji T, Angelo S, Kyriakides TC, Helton SW. Small bowel obstruction: outcome and cost implications of admitting service. Am Surg. 2010 Jul;76(7):687-91.
- Sternick M, Licata A, Britt R. Outcomes of Small Bowel Obstructions by Admitting Specialty and Hospital Type. Am Surg. 2023 Feb 16:31348231157865.
- Törer N, Nursal TZ, Tufan H, Can F, Bal N, Tarim A, Moray G, Haberal M. Effect of manual bowel decompression (milking) in the obstructed small bowel. Am J Surg. 2008 Jun;195(6):807-13.
- Ezer A, Torer N, Colakoglu T, Colakoglu S, Parlakgumus A, Yildirim S, Moray G. Clinical outcomes of manual bowel decompression (milking) in the mechanical small bowel obstruction: a prospective randomized clinical trial. Am J Surg. 2012 Jan;203(1):95-100.
- Aysan E, Demir M, Kinaci E, Basak F. Complications of intestinal milking: experimental model. ANZ J Surg. 2005 May;75(5):322-5.