Serrated Polyposis Syndrome (SPS)
Jackson Phillip Bauer, MD
The Operative Review of Surgery. 2023; 1:126-128.
Table of Contents
Pathophysiology and Presentation
Historically Known as “Hyperplastic Polyposis Syndrome”
Genetic Mutations
- Genetic Basis is Mostly Unknown 1
- Mutations in RNF43 are Most Closely Related 2
- Most Patients Have No Predisposing Mutation (97%) 2
Colorectal Cancer
- Lifetime Risk: 25-70% 3-5
- 5-Year Incidence: 1.5% 6
Extracolonic Manifestations
- Overall Incidence: 6
- 54% Have a Family History of Extracolonic Malignancy
- 24% Develop an Extracolonic Malignancy
- Exact Associations are Debated 7,8
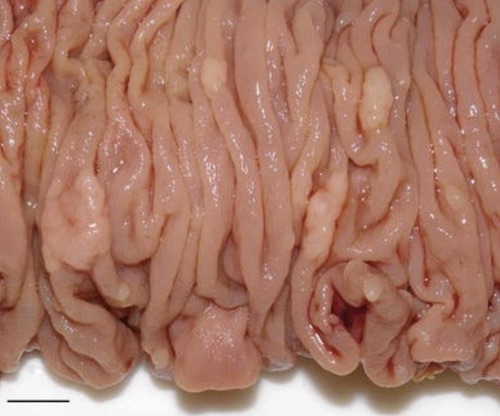
Colectomy Specimen with Multiple Sessile Polyps in a Patient with SPS 9
Diagnosis and Management
Diagnosis (WHO 2019 Criteria) 10
- Either:
- ≥ 5 Serrated Lesions/Polyps Proximal to the Rectum
- All ≥ 5 mm in Size
- Two ≥ 10 mm in Size
- > 20 Serrated Lesions/Polyps Throughout the Colon
- ≥ 5 Polyps Proximal to the Rectum
- ≥ 5 Serrated Lesions/Polyps Proximal to the Rectum
- Polyp Count is Cumulative Over Multiple Colonoscopies 5
- Criteria are Not Systematically Applied and the Diagnosis is Often Missed 11
- *Historical 2010 WHO Criteria Also Included “Any Number of Serrated Polyps Proximal to the Sigmoid Colon with a Family History of SPS in a First-Degree Relative”, Now Removed
Screening/Surveillance 1
- Colonoscopy Every 1-3 Years
- May Consider Shorter Intervals of 1-2 Years 12
- Starting Age Not Clearly Defined
- No Extracolonic Cancer Surveillance Indicated
Colectomy
- Indications for Colectomy: 1
- Unable to Control the Growth of Serrated Polyps
- Development of Colorectal Cancer
- Prophylactic Colectomy Generally Not Indicated
- Generally Recommend Total Abdominal Colectomy with Ileorectal Anastomosis (TAC/IRA) 1
- May Consider Segmental Colectomy or Proctocolectomy if Indicated
Other Colorectal Cancer and Polyposis Syndromes
Syndromes
- Familial Adenomatous Polyposis (FAP)
- Lynch Syndrome
- Juvenile Polyposis Syndrome (JPS)/Familial Juvenile Polyposis
- MUT Y Homolog (MUTYH)-Associated Polyposis (MAP)
- Peutz-Jeghers Syndrome (PJS)
- Serrated Polyposis Syndrome (SPS)
- PTEN Hamartoma Tumor Syndromes: (PHTS)
Comparisons
References
- Syngal S, Brand RE, Church JM, Giardiello FM, Hampel HL, Burt RW; American College of Gastroenterology. ACG clinical guideline: Genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015 Feb;110(2):223-62; quiz 263.
- Stanich PP, Pearlman R. Hereditary or Not? Understanding Serrated Polyposis Syndrome. Curr Treat Options Gastroenterol. 2019 Dec;17(4):692-701.
- Boparai KS, Mathus-Vliegen EM, Koornstra JJ, Nagengast FM, van Leerdam M, van Noesel CJ, Houben M, Cta A, van Hest LP, Fockens P, Dekker E. Increased colorectal cancer risk during follow-up in patients with hyperplastic polyposis syndrome: a multicentre cohort study. 2010;59:1094–100.
- IJspeert JE, Rana SA, Atkinson NS, van Herwaarden YJ, Bastiaansen BA, van Leerdam ME, Sanduleanu S, Bisseling TM, Spaander MC, Clark SK, Meijer GA, van Lelyveld N, Koornstra JJ, Nagtegaal ID, East JE, Latchford A, Dekker E Dutch workgroup serrated polyps & polyposis (WASP) Clinical risk factors of colorectal cancer in patients with serrated polyposis syndrome: a multicentre cohort analysis. 2017;66:278–84.
- Song H, Tetangco E, Martin E, Willhite D, Yap JEL. Serrated Polyposis Syndrome: Increasing Awareness and Importance. Cureus. 2020 Jul 15;12(7):e9198.
- Fousekis FS, Mitselos IV, Christodoulou DK. Diagnosis, epidemiology and management of serrated polyposis syndrome: a comprehensive review of the literature. Am J Transl Res. 2021 Jun 15;13(6):5786-5795.
- Hazewinkel Y, Reitsma JB, Nagengast FM, Vasen HF, van Os TA, van Leerdam ME, Koornstra JJ, Dekker E. Extracolonic cancer risk in patients with serrated polyposis syndrome and their first-degree relatives. Familial Cancer. 2013;12:669–73.
- Edelstein DL, Cruz-Correa M, Soto-Salgado M, Axilbund JE, Hylind LM, Romans K, Blair C, Wiley E, Tersmette AC, Offerhaus JA, Giardiello FM. Risk of colorectal and other cancers in patients with serrated polyposis. Clin Gastroenterol Hepatol. 2015;13:1697–9.
- Rosty C, Hewett DG, Brown IS, Leggett BA, Whitehall VL. Serrated polyps of the large intestine: current understanding of diagnosis, pathogenesis, and clinical management. J Gastroenterol. 2013 Mar;48(3):287-302. (License: CC BY-NC 2.0)
- Dekker E, Bleijenberg A, Balaguer F Dutch-Spanish-British Serrated polyposis Syndrome collaboration. Update on the world health organization criteria for diagnosis of serrated polyposis syndrome. 2020;158:1520–3.
- Vemulapalli KC, Rex DK. Failure to recognize serrated polyposis syndrome in a cohort with large sessile colorectal polyps. Gastrointest Endosc. 2012;75:1206–10.
- East JE, Atkin WS, Bateman AC, Clark SK, Dolwani S, Ket SN, Leedham SJ, Phull PS, Rutter MD, Shepherd NA, Tomlinson I, Rees CJ. British Society of Gastroenterology position statement on serrated polyps in the colon and rectum. 2017;66:1181–96.