Ostomy
Ostomy
David Ray Velez, MD
Table of Contents
Definitions
Ostomy: A Surgically Created Anastomosis of the GI Tract and Skin to Allow Fecal Diversion
Stoma: The Physical End of Bowel Protruding Through the Abdominal Wall
- The Terms “Ostomy” and “Stoma” are Often Used Interchangeably in Practice
Bowel Segment
- Ileostomy: Segment of Ileum Used for Ostomy
- Generally Higher Output with More Liquid Contents
- Colostomy: Segment of Colon Used for Ostomy
- Generally Lower Output with More Foul-Smelling Feculent Contents
Bowel End
- Loop-Ostomy: A Loop of Bowel is Brought to the Skin with Two Openings (One Proximal and One Distal)
- Defunctionalized Distal Limb: The Proximal Functional Limb is Everted to Occupy the Majority of the Aperture and the Distal Limb is Not Everted
- Double Barrel: Both Limbs are Everted to Occupy Similar Spaces
- End-Ostomy: A Single End of Bowel is Brought to the Skin for Drainage
Permanence
- Permanent Ostomy: No Plans for Later Takedown
- *A Permanent Colostomy is Preferred Over a Permanent Ileostomy if Able (Lower Risk of Dehydration and Electrolyte Abnormalities)
- Temporary/Diverting Ostomy: Used to Allow Healing of a Distal Site Due to a High-Risk Anastomosis, Injury, or Wound with Plans for Later Takedown
- *A Temporary Loop-Ileostomy is Generally Preferred Over a Temporary End-Ostomy if Able Because it is Easier to Takedown in the Future

Colostomy
Site Selection
General Preferred Site
- 4-5 cm Circular Site
- Just Inferolateral to the Umbilicus on Either Side
- Within the Rectus Abdominis Muscle
- Provides Support and Stability
- *May Consider Other Sites Dependent on Body Habitus – Obese May Be Better Suited in the Upper Abdomen
“Ostomy Triangle”
- A Conceptual Area of the Abdominal Wall Used to Guide Placement of an Ostomy
- Landmarks:
- Umbilicus
- Pubic Tubercle
- ASIS
Patient Must Be Able to Visualize and Access the Stoma Easily
- Obese Often Require Placement Higher Above the Umbilicus
Ostomy Site Must Be Flat to Avoid Interference of Appliance Adherence
- Avoid Creases, Folds, Beltline, Previous Incisions, Umbilicus, and Bony Prominences
Ensure ≥ 2 Inch Perimeter of Clear Intact Skin for Stoma Appliance Application
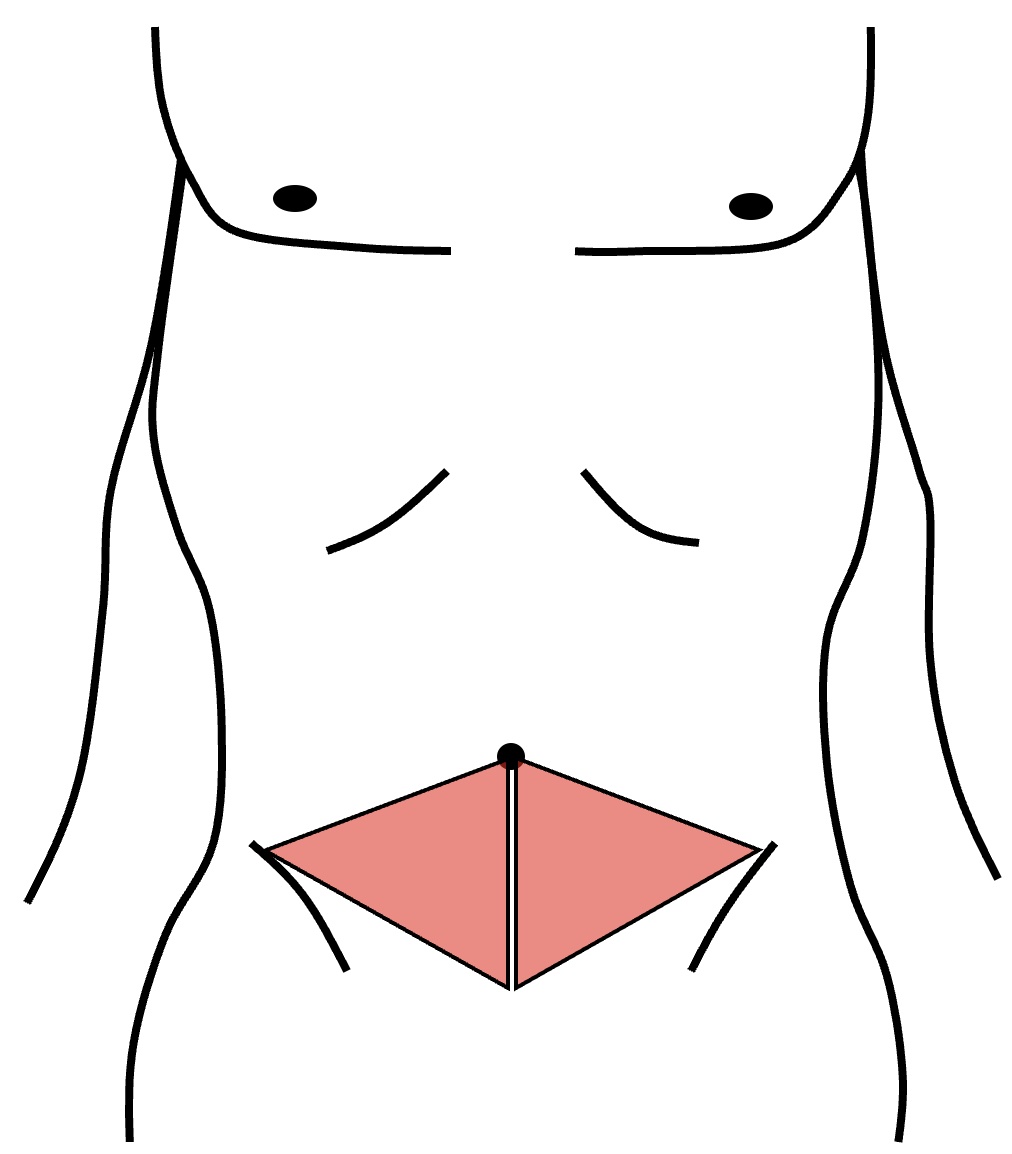
Ostomy Triangle
Procedure
General Procedure
- Mobilize the Bowel
- Create the Abdominal Wall Opening
- Create a 4-5 cm Circular Skin Incision at the Selected Site
- Carry Incision Down Through the Subcutaneous Tissue to the Fascia
- Create a Cruciate (Cross) Incision Through the Fascia
- Spread the Rectus Muscle and Create an Incision Through the Posterior Fascia/Peritoneum
- Spread the Fascial Opening to Ensure Bowel Can Easily Pass Through – Often Dilated Until 2-3 Fingers Can Pass
- May Consider Placing Prophylactic Mesh – Debated
- Deliver the Bowel Segment Through the Opening
- Close the Remaining Abdominal Incisions (Midline, etc.)
- “Mature” the Ostomy
- Consider Placing an Ostomy Bridge for Loop-Ostomies
- Open the Bowel
- For Loop-Ostomy: Transect 80% of the Circumference of the Bowel at Antimesenteric Side
- Place Four Stay-Sutures
- Evert by Placing Brooke Sutures Throughout
- Ileostomy: 3 cm Proximal Seromuscular Bite
- Colostomy: 1-2 cm Proximal Seromuscular Bite
- Place an Ostomy Appliance Over the Stoma
The Difficult Ostomy – Options to Gain Bowel Length if Difficult to Reach
- Always Mark Site Beforehand (Obese Require a More Cephalad Site)
- Fully Mobilize the Bowel (Splenic Flexure, Lateral Attachments, Omental Attachments, Retroperitoneal Attachments, and Any Adhesions)
- “Pie Crust”/“Score” the Mesentery – Creating Sequential “Windows” within the Mesentery
- Divide Mesentery/Blood Supply Proximally
- *First Ensure that There are Adequate Distal Arcades to Supply Blood for the Ostomy
- Divide IMA Close to its Base
- Divide IMV Just Lateral to the Ligament of Treitz
- Ensure the Trephine/Opening is Large Enough
- Consider a “Loop-End” Ostomy if the End Will Still Not Reach – Closed Blind End is Just Under the Skin if a Point a Few cm More Proximal Has Better Reach
- Also Known as an “End-Loop” or “Pseudo-Loop”
- Subcutaneous Lipectomy – Remove Subcutaneous Fat and Fix Skin to the Fascia
Ostomy Bridge (Stoma Rod)
- A Bar Placed Under a Loop-Ostomy to Stabilize at the Skin Level While Ostomy Granulates
- Removed After 3-5 Days
- Goal: Prevent Stoma Retraction
- Outcomes:
- No Evidence of Reduced Risk of Stoma Retraction
- Increased Risk of Local Complications (Edema, Skin Necrosis, Irritant Dermatitis, Peristomal Abscess, and Bleeding)
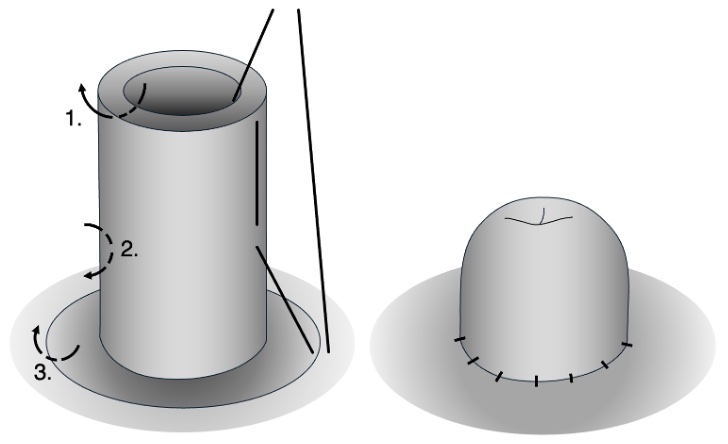
Brooke Suture: (1) Full-Thickness Including Mucosa and Serosa; (2) Seromuscular Bite 2-3 cm Proximal; (3) At the Skin Edge
Takedown/Reversal
Definition: Reconnecting the Intestines and Closure of the Stoma to Allow Stool to Exit Through the Rectum Again
Timing
- Minimum Time to Closure: 6-12 Weeks (12 Preferred)
- Allows Resolution of Acute Inflammation and Dense Adhesions
Preoperative Evaluation
- If Protecting a Distal Anastomosis: Obtain a Contrast Enema or Flexible Sigmoidoscopy Prior to Reversal to Ensure Anastomosis is Intact
- If After Hartmann’s Procedure for Perforated Diverticulitis:
- Consider a Flexible Sigmoidoscopy with Colonoscopy of the Remaining Proximal Colon if Symptomatic, if Otherwise Meets Normal Screening Criteria, if at High Risk (Crohn’s), or if Needed to Evaluate Anatomy
- May Consider Forgoing Preoperative Endoscopy in Asymptomatic Patients with No Other Indications
Considerations
- End-Ostomy Will Require a New Bowel Anastomosis to Reestablish Continuity
- Loop-Ostomy is Done Through a Peristomal Circumferential Incision and Can Be Closed Transversely or by a New Anastomosis
- Use Sharp Dissection and Avoid Serosal Tears from Blunt Dissection
Wound Closure Techniques
- Purse-String Closure (PSC)
- Generally Considered to Have One of the Lowest Risks of Surgical Site Infection (SSI)
- Allows Drainage Through the Small Central Opening
- Delayed Wound Healing by Secondary Intention Over Weeks
- Consistently Demonstrated Improved Cosmetic Outcomes to Primary Closure
- Primary Closure
- Fastest Healing
- Higher Rates of Surgical Site Infection (SSI)
- Some Prefer Primary Closure Over a Penrose Drain to Allow Continued Drainage – Evidence Shows No Benefit with Similar Rates of SSI
- Secondary Intention (Left Open)
- Lowest Risk of Surgical Site Infection (SSI) – Nothing Closed
- Longest Healing Time with the Greatest Need for Wound Care
- Negative Pressure Wound Therapy (NPWT)
- Consistently Demonstrated Improved Rates of SSI Over Primary Closure but No Proven Benefit Over Purse-String Closure
- Has Been Used in Conjunction with Purse String Closure (PSC-NPWT) but with No Proven Benefit
Complications
Loop-Ileostomy Has the Highest Overall Complication Rate
Most Common Complications: Dehydration and Skin Irritation
High-Ostomy Output
Stomal Ischemia/Necrosis
Mucocutaneous Separation (MCS)
Stomal Retraction
Parastomal Hernia
Stomal Prolapse
Stomal Stenosis/Stricture