Endocrine: Thyroid Nodule Management
Thyroid Nodule Management
Thyroid Nodules
- High-Prevalence in General Population: 37-57%
- Majority (90%) are Benign
- Only 50% in Peds
- Carcinoma Risk Factors:
- Age Extremes (Pediatrics & Elderly)
- Male Sex
- History of Radiation to Head & Neck
- Most Likely Papillary if From a History of XRT
- Solitary Nodule (vs Multinodular)
- Large ≥ 2 cm
Initial Management
- Initial Testing: Thyroid Function Tests (TFTs) & Ultrasound (US)
- If Patient Is Hyperthyroid May First Consider Scintigraphy (Radioiodine Uptake Scan)
- Hot Nodule/Hyperfunctioning: Benign – No Further Testing
- Cold Nodule: Risk for Malignancy – Further Testing/US is Indicated
Ultrasound (US) – Concerning Features
- Most Specific:
- Taller > Wide (Normal Grows Radially)
- Microcalcifications
- Heterogenous
- Hypoechoic
- Solid (vs Cystic)
- Lobulated/Irregular Margins
- Hypervascular
Indications for Fine Needle Aspiration/FNA (Based on US)
- Intermediate-High Suspicion: ≥ 1.0 cm
- Low Suspicion: ≥ 1.5 cm
- Very-Low Suspicion: ≥ 2.0 cm
- Purely Cystic: FNA Not Indicated
Bethesda System for Reporting Thyroid Cytopathology (Based on FNA)
- Category I: Nondiagnostic or Unsatisfactory
- Category II: Benign
- Category III: Undetermined Significance
- Atypia of Undetermined Significance (AUS)
- Follicular Lesion of Undetermined Significance (FLUS)
- Category IV: Follicular Neoplasm or Suspicious for a Follicular Neoplasm
- Category V: Suspicious for Malignancy
- Category VI: Malignant
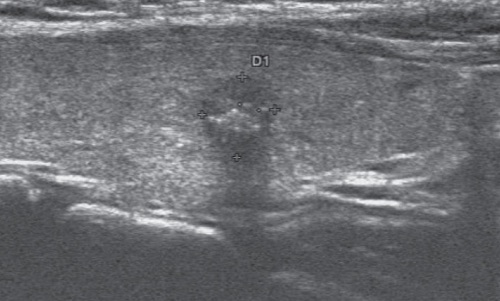
Thyroid Nodule Malignant Findings: Solid, Heterogenous, Hypoechoic, Microcalcifications 1
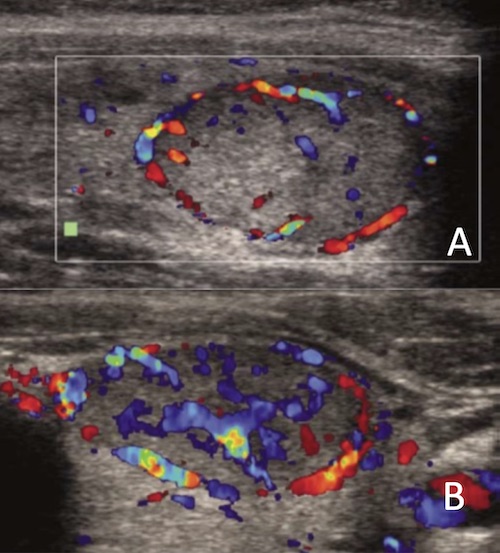
Thyroid Nodule Vascularity; (A) Normal/Benign, (B) Hypervascular/Malignant 2
Risk of Malignancy
| Category | Risk if NIFTP ≠ CA | Risk if NIFTP = CA |
| I | 5-10% | 5-10% |
| II | 0-3% | 0-3% |
| III | 6-18% | 10-30% |
| IV | 10-40% | 25-40% |
| V | 45-60% | 50-75% |
| VI | 94-96% | 97-99% |
- NIFTP = Noninvasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features
- CA = Carcinoma
Management (Based on Bethesda Category)
- Category I: Repeat FNA
- Consider Excision if Repeat FNA Again Results Category I
- Category II: Clinical Follow Up
- Category III: Repeat FNA (May Consider Molecular Testing)
- Category IV: Lobectomy/Hemithyroidectomy (May Consider Molecular Testing)
- Category V: Lobectomy/Hemithyroidectomy vs. Total Thyroidectomy
- Category VI: Lobectomy/Hemithyroidectomy vs. Total Thyroidectomy
Molecular Testing (Afirma, ThyroSeq, etc.)
- Recent Advancement that Has Reduced the Need for Unnecessary Surgery
- Tests for High-Risk Mutations (RET, BRAF, VEGFR, etc.)
- Better Used to Rule-Out Malignancy than to Rule-In
- Negative Predictive Value (NPV): > 95%
- Positive Predictive Value (PPV): 40-80%
- Sensitivity: 90%
- Specificity: 50-90%
References
- Chen M, Zhang KQ, Xu YF, Zhang SM, Cao Y, Sun WQ. Shear wave elastography and contrast-enhanced ultrasonography in the diagnosis of thyroid malignant nodules. Mol Clin Oncol. 2016 Dec;5(6):724-730. (License: CC BY-NC-ND-4.0)
- Salehi M, Nalaini F, Izadi B, Setayeshi K, Rezaei M, Naseri SN. Gray-scale vs. color doppler ultrasound in cold thyroid nodules. Glob J Health Sci. 2014 Nov 26;7(3):147-52. (License: CC BY-3.0)