Appendicitis
David Ray Velez, MD
The Operative Review of Surgery. 2023; 1:77-92.
Table of Contents
Pathophysiology
Normal Appendix Anatomy
- Maximal Outer Diameter: 6-mm 1
- Considered the Most Important Diagnostic Criteria to Exclude Appendicitis 1
- Maximal Mural Thickness: 3-mm 2,3
- Length: 8-10-cm 1
- Luminal Capacity: 1 cc 4
- Fluid > 0.5 cc Raises Intraluminal Pressure 4
- “Vermiform Appendix” Simply References the “Worm-Like” Appearance
- Blood Supply:
- Appendicular Artery within the Mesoappendix (Off the Ileocolic Artery)
- Venous Drainage Goes to the Portal System
Function of the Appendix
- Reservoir for Good Bacteria After Diarrheal Infection Cleans Out the Colon 6
- *Historically Thought to Be a Vestigial Structure without Function
- Secretes IgA and Mucin to Assist in this Biofilm Creation 7
Anatomical Positioning 8,9
- Retrocecal (32-62%) – Behind the Cecum (Most Common)
- Pelvic (10-37%) – Within Pelvis
- Subcecal (2-24%) – Inferior to & Extending from the Cecum
- Preileal (1-19%) – Anterior to Ileum
- Postileal (0.4-16%) – Posterior to Ileum
Appendicitis Pathology
- Primarily Caused by Luminal Obstruction and Stasis
- *Exact Cause is Poorly Understood 11
- Causes of Luminal Obstruction: 11
- Appendicolith (Fecalith at the Appendiceal Orifice)
- Impacted Stool
- Appendiceal/Cecal Tumor
- Effects of Luminal Obstruction: 12
- Swelling and Mucous Secretion
- Increased Luminal and Intramural Pressures
- Small Vessel Thrombosis and Lymphatic Stasis
- Impaired Blood Flow and Venous Congestion
- Bacterial Infection
- Can Progress to Ischemia and Necrosis
- Lymphoid Hyperplasia was Previously Believed to Be a Primary Cause of Appendicitis but Now Disproven – *See Below

Appendix 5

Anatomic Position of the Appendix 10
Presentation
Epidemiology 13
- Most Common in Age 20-30’s
- More Common in Men
- More Common in Patients with Low Socioeconomic Status
Perforation
- 13-20% Present with Perforation 14
- Can Present with a Contained Walled-Off Abscess or Free Perforation
- Most Common Site of Perforation: Antimesenteric Border Just Beyond the Point of Obstruction 15
- Typically in the Middle Third of the Appendix
- This Area Has the Poorest Blood Supply
- Risk Factors for Perforation:
- Pediatrics 16,17
- Can Be Significantly Higher for Younger Children < 3-5 Years 17,18
- Possibly Due to Delayed Diagnosis
- Due Underdeveloped Omentum it is More Difficult to Wall Off an Abscess After Perforation 19
- Age > 50 Years 20
- Symptom Duration > 24 Hours 21
- Presence of a Fecalith 22,23
- WBC > 15,000 24
- CRP > 30,000 25
- HIV 26
- In-Hospital Delay to Surgery May Be Associated with Increased Risk of In-Hospital Perforation – Studies Contradictory 27-29
- Pediatrics 16,17
- Increased Mortality Rate: 5% 30
- Compared to 0.1% for Non-Gangrenous Appendicitis and 0.6% for Gangrenous Appendicitis 30
Presentation
- Lifetime Risk of Developing: 7-8% 31
- Initial Periumbilical Pain that Migrates to the Right Lower Quadrant
- 50-60% Demonstrate Migration 13
- Initial Periumbilical Pain Caused Appendix Stretching Leading to Stimulation of T8-10 Visceral Nerve Fibers 32
- Migrating Right Lower Quadrant Pain Caused by Inflammation of the Surrounding Parietal Peritoneum Leading to Stimulation of the Somatic Nerve Fibers 13
- Pain Worse with Walking, Jumping or Coughing
- Anorexia (80-85%) 13
- Nausea and Vomiting (40-60%) 13
- Nausea and Anorexia Occur After Pain Once Secondary Visceral Afferent Fibers Stimulate the Medullary Vomiting Center (Occurs Before Pain in Gastroenteritis)
- Fever

Appendicitis After Resection 33
Diagnosis
- McBurney Sign
- Right Lower Quadrant Tenderness at McBurney’s Point
- McBurney’s Point: 1/3 the Distance from the Anterior-Superior Iliac Spine (ASIS) to the Umbilicus
- Sensitivity: 50-94%; Specificity: 75-86% 13
- Most Reliable Finding
- Rovsing Sign
- Right Lower Quadrant Pain with Left Lower Quadrant Palpation
- Sensitivity: 22-68%; Specificity: 58-96% 13
- Iliopsoas/Psoas Sign
- Right Lower Quadrant Pain on Extension of the Right Thigh
- Indicates: Retrocecal Appendix
- Sensitivity: 13-42%; Specificity: 79-97% 13
- Obturator Sign
- Right Lower Quadrant Pain on Internal Rotation of Right Thigh
- Indicates: Pelvic Appendix
- Likely to Associated with Dysuria & Diarrhea
- Sensitivity: 8%; Specificity: 94% 13
- Labs: WBC and CRP
- First-Line Imaging: Computed Tomography (CT)
- Study of Choice by the American College of Radiology 34,35
- IV Contrast Preferred, Oral Contrast Not Necessary 36
- Sensitivity: 91%; Specificity 90% 13
- Alternative Imaging Modalities:
- Ultrasound (US)
- Some Consider as an Initial Imaging Test Although Negative US Does Not Rule Out Appendicitis and Should Be Followed by CT if US Equivocal 37
- Preferred for Pediatrics or Pregnant Women to Limit Radiation Exposure 13
- Sensitivity: 78%; Specificity: 83% 13
- Magnetic Resonance Imaging (MRI)
- Most Commonly Used in Pediatrics or Pregnant Women if US Equivocal 13
- More Expensive and Less Familiarity
- Ultrasound (US)
- Radiographic Findings:
- Appendix Noncompressible
- Appendix Distended ≥ 6-7 mm
- Appendix Wall Thickening ≥ 3 mm
- Appendicolith (40%) 38
- Associated with More Severe Inflammation and Increases Risk for Perforation
- Periappendiceal Fluid and Fat Stranding
- Gangrenous Appendicitis with or without Perforation
- Appendicitis with an Intraabdominal Abscess
- Appendicitis with Periappendicular Contained Phlegmon
- Appendicitis with Periappendicular Purulent/Free Fluid
- Alvarado Scoring System 41 Mn
- The Most Commonly Used System in Adults
- Points:
- Tenderness in RLQ (2)
- Migration to RLQ (1)
- Rebound Tenderness (1)
- Anorexia (1)
- Nausea/Vomiting (1)
- Elevated Temperature (1)
- Leukocytosis; WBC > 10,000 (2)
- Shift of Neutrophils (1)
- Interpretation: 42
- Low Scores (0-3): Evaluate Other Etiologies (No CT Indicated)
- Intermediate Scores (4-6): CT Scan
- High Scores (7-10): Surgical Consultation
- Low Scores Are Better to “Rule-Out” Appendicitis than High Scores Are to “Rule-In”
- Score < 3-4 to “Rule-Out” Appendicitis Has 96% Sensitivity
- Score > 6-7 to “Rule-In” Appendicitis Has 58-88% Sensitivity
- Pediatric Appendicitis Score (PAS) 43
- Most Commonly Used in Pediatrics
- Points:
- RLQ Tenderness (2)
- Pain with Cough, Percussion or Hopping (2)
- Anorexia (1)
- Nausea/Emesis (1)
- Migration of Pain (1)
- Fever (1)
- Leukocytosis; WBC > 10,000 (1)
- Neutrophilia; ANC > 7,500 (1)
- Interpretation: 44
- Low Scores (0-3): Evaluate Other Etiologies
- Intermediate Scores (4-6): Imaging
- High Scores (7-10): Imaging vs Surgery
- Additional Scoring Systems:
- Appendicitis Inflammatory Response (AIR) Score 45
- RIPASA (Raja Isteri Pengiran Anak Saleha Appendicitis) Score 46
- Eskelinen Score 47
- Ohmann Score 48
- Tzanakis Score 49
- Lintula Score 50
- Fenyo-Lindberg Score 51
- Karaman Score 52

Appendicitis with Fecalith 39
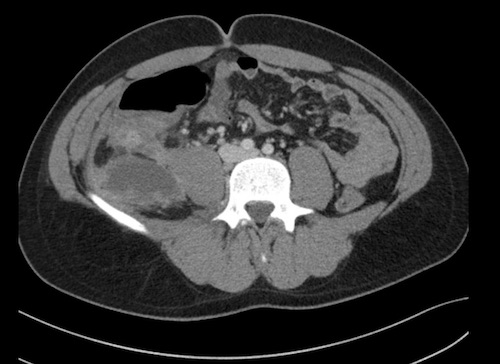
Perforated Appendicitis 39
Treatment
Definitive Management
- Uncomplicated Appendicitis: Laparoscopic Appendectomy
- *See Appendectomy
- May Consider Nonoperative Management with Antibiotics Alone for Select Patients – *See Below
- Complicated Appendicitis (Phlegmon/Abscess): Antibiotics & Interval Appendectomy at 6-8 Weeks
- Percutaneous Drainage if Abscess > 3-4 cm
- Antibiotic Course:
- After Percutaneous Drainage: 4 Days 54
- If Unable to Perform Percutaneous Drainage: 7 Days
- 80% Successful in Avoiding Appendectomy on Initial Admission 55
- Free Perforation: Appendectomy
Intraoperative Findings
- Normal Appendix: Historically Recommended That the Appendix was Always Resected Even if Normal at Diagnostic Laparoscopy for Acute Right Iliac Fossa Pain
- Goal: Prevent Risk of Diagnostic Confusion in the Future
- Debated in Modern Practice 56
- Friable Base: Partial Cecectomy
- Take Care to Preserve the Ileocecal Valve
- Suspect Chron’s Disease and Cecum Inflamed: No Intervention
Nonoperative Management
- Some Promote Antibiotic Treatment Alone for Uncomplicated Acute Appendicitis 57
- Not Recommended for Complicated Appendicitis
- *In General, Surgical Management is Preferred but May Consider Nonoperative Management if Unfit for Surgery or the Patient Refuses Surgery
- Benefits:
- Most Respond Clinically
- Faster Return to Work (Not for Complicated/Perforated Cases)
- No Increased Perforation Rate
- 89-91% Are Able to Avoid Surgery at Initial Admission
- Negatives:
- High Recurrence Rates
- 29% Require Appendectomy by 90 Days 57
- 25% Without Appendicolith 57
- 41% With Appendicolith 57
- 14-40% Require Appendectomy within the First Year 57-60
- 40-50% Require Appendectomy within the First 5-Years 57,61
- 28x Higher Rates of Complications 57
- 29% Require Appendectomy by 90 Days 57
- Treatment Efficacy at 1-Year: 62
- Nonoperative Management: 63.8%
- Surgical Management: 93%
- Contraindicated if Fecalith Present – High Rate of Complicated Appendicitis that May be Underestimated on Imaging
- High Recurrence Rates
- Immunocompromised and Significant Comorbidity Patients Have Mostly Been Excluded from Prior Studies with Uncertain Efficacy
Interval Appendectomy
- Definition: Appendectomy Done After a Trial of Nonoperative Management with Antibiotics
- Generally Done After 6-8 Weeks
- Comparison to an Immediate Appendectomy for Complicated Appendicitis:
- Decreased Risk of Complications (SBO, Prolonged Ileus, Surgical Site Infection & Reoperation) 63
- May Have Longer Return to Activity (Debated) 63,64
- Some Recommend Against Interval Appendectomy Due to Low Recurrence Rate, Although One of the Most Compelling Reason for Interval Appendectomy is the Increased Risk of Neoplasm After Perforation
- Risk of Recurrence: 5-38%
- Risk of Neoplasm After Interval Appendectomy for Complicated Appendicitis: 11% 65
- If Interval Appendectomy is Forgone, Patients Over 40 Years Old Should Have an Interval Colonoscopy and CT 30
Incidental (Prophylactic) Appendectomy
- Definition: Appendectomy During Another Separate Procedure without Evidence of Appendicitis
- Goal: Eliminate Future Risk of Appendicitis
- Indications Not Defined
- Associated with Complications and Generally Avoided 66
- Contraindications: 67
- Unstable Hemodynamics
- Established Crohn’s Disease
- Inaccessible Appendix
- Predetermined Plan for Radiation Treatment
- Pathologically or Iatrogenically Immunosuppressed
- Most Often Done for Patients Under Age 30-35 Years (Highest Incidence) During Hysterectomy, Cholecystectomy, Sigmoidectomy, or Trauma Laparotomy

Laparoscopic Appendectomy 53
Appendicitis in Pregnancy
General Information
- Overall Pregnant Women are Less Likely than Nonpregnant Women to Have Appendicitis 68
- The Most Common Non-Obstetric Indication for Surgery During Pregnancy
- Appendix Perforation is More Common – Possibly Due to Diagnostic Challenges and Hesitancy to Operate on Pregnant Women 69,70
Considerations by Trimester
- First Trimester:
- Appendicitis is the Most Common Cause of Acute Abdominal Pain
- Second Trimester:
- Most Frequent Trimester 68
- Third Trimester:
- Lowest Overall Rate of Appendicitis 71
- Most Likely to Perforate 69,70
Risks/Outcomes
- Maternal Morbidity and Mortality are Similar to Nonpregnant Women 72
- Uncomplicated Appendicitis: 73,74
- Fetal Loss: 1.5-2.0%
- Preterm Labor: 6%
- Complicated Appendicitis: 73,74
- Fetal Loss: 8-36%
- Preterm Labor: 11%
- Highest Risk for Fetal Mortality: Appendix Rupture
- In General, Appendectomy During Pregnancy Does Not Negatively the Child 75
Presentation
- Only 50-60% Have a Classical Clinical Presentation
- May Instead Present with Heartburn, Flatulence, or Diarrhea
- Location of Pain:
- Most Commonly at McBurney’s Point Regardless of Trimester 76,77
- May Migrate to the Right Mid-Upper Quadrant in the Third Trimester Due to a Gravid Uterus 78,79
- Leukocytosis May Be Normal in Pregnancy 80
Treatment
- Uncomplicated Appendicitis: Appendectomy
- Optimal Approach Remains Inconclusive 81
- Laparoscopic vs Open Appendectomy
- Laparoscopic Associated with Lower Overall Complications and Shorter Length of Stay 81
- Laparoscopic Associated with Higher Rate of Fetal Loss (Odds Ratio 1.82) 81,82
- Similar Rates of Preterm Labor 82
- Laparoscopic Trocar Placement: *See Appendectomy
- Open Incision: Generally Recommended to Make at McBurney’s Point or the Site of Maximal Pain (Possibly More Cephalad)
- Complicated Appendicitis:
- Phlegmon/Abscess: Debated
- Poor Evidence to Guide Decision Making
- Consider Antibiotics with Percutaneous Drainage and Interval Appendectomy (Similar to Nonpregnant Patients) vs Immediate Appendectomy
- Free Perforation: Open Appendectomy
- Phlegmon/Abscess: Debated
Similar Pathology
Appendiceal Lymphoid Hyperplasia
- Definition: Increased Size of Lymphoid Tissue within the Appendix
- A Physiologic Response to Inflammation 83
- Often Associated with Inflammatory Conditions Such as Viral Gastroenteritis or Mesenteric Adenitis 83
- Previously Believed to Be a Primary Cause of Appendicitis but Now Disproven 83
- Can Mimic Appendicitis with a Noncompressible and Dilated Appendix 84
- Most Successful Parameters to Distinguish Appendicitis from Lymphoid Hyperplasia: 84
- Periappendiceal Fluid Collection
- Lamina Propria Thickness ≤ 1 mm
Mesenteric Lymphadenitis (Mesenteric Adenitis)
- Also Known as “Pseudoappendicitis”
- Definition: Mesenteric Lymph Node Inflammation
- A Self-Limiting Inflammatory Condition that Resolves Over 1-10 Weeks
- Can Be a Primary/Nonspecific Etiology or Secondary
- Often Presents Similar to Appendicitis
- Most Common in Pediatrics
- More Common than Appendicitis in the First Decade of Life 85
- Secondary Causes: 86
- Viral Infection – Most Common Cause
- Gastroenteritis
- Upper Respiratory Infection (URI)
- Bacterial Infection
- Inflammatory Bowel Disease
- Lymphoma
- Viral Infection – Most Common Cause
- Diagnosis: Generally Made by Imaging (US or CT) 85
- Must First Rule Out Other Diagnoses
- Treatment: Supportive Care (Fluid Resuscitation and NSAID’s) 85,86
- No Biopsy or Surgery Necessary
Periappendicitis
- Definition: Appendiceal Serosal Inflammation without Mucosal Inflammation
- Caused by Non-Appendiceal Inflammation
- Often Presents Similar to Appendicitis
- 1-5% of Appendices Resected for Clinical Acute Appendicitis are Found to Have Periappendicitis Alone 87
- Causes: 87
- Salpingitis (Gonococcal or Chlamydial) – Most Common Cause 87
- Pelvic Inflammatory Disease (PID)
- Peritoneal Tuberculosis
- Inflammatory Bowel Disease (IBD)
- Infectious Colitis
- Diverticulitis
- Urologic Disease
- Distant Perforation Elsewhere
- Colonic Neoplasia
- Valentino’s Syndrome: Periappendicitis Caused by a Perforated Gastric/Duodenal Ulcer 88
- Diagnosis May Be Difficult to Make Preoperatively
- Treatment: Based on Underlying Cause
Appendiceal Mucocele (Non-Neoplastic Mucinous Lesion/Retention Cyst)
Appendix Cancer
Mnemonics
Signs of Appendicitis
- McBurney Sign – “Burns” Right Over the Appendix
- Rovsing Sign – Think “Roving” Pain Elicited from a Distant Site
- Psoas Sign (Pso-Po) – Posterior (Retrocecal Position)
- Obturator Sign (Ob-Ob) – Obstetrics (Pelvic Location & Internal Rotation to Pelvis)
Alvarado Score
- Often Referred to as “MANTRELS” Score
- M: Migration to RLQ (1)
- A: Anorexia (1)
- N: Nausea/Vomiting (1)
- T: Tenderness in RLQ (2)
- R: Rebound Tenderness (1)
- E: Elevated Temperature (1)
- L: Leukocytosis; WBC > 10,000 (2)
- S: Shift of Neutrophils (1)
References
- Park NH, Oh HE, Park HJ, Park JY. Ultrasonography of normal and abnormal appendix in children. World J Radiol. 2011 Apr 28;3(4):85-91.
- Simonovský V. Normal appendix: is there any significant difference in the maximal mural thickness at US between pediatric and adult populations? 2002;224:333–337.
- Wiersma F, Srámek A, Holscher HC. US features of the normal appendix and surrounding area in children. 2005;235:1018–1022.
- Bernard M. Jaffe,Chapter 30, The Appendix ,Schwartz’s Principles of Surgery, ninth edition. 2010. p. 2043-2047.
- Gray H. Anatomy of the Human Body (1918). Public Domain.
- Bollinger RR, Barbas AS, Bush EL, Lin SS, Parker W. 2007. Biofilms in the normal human large bowel: fact rather than fiction. Gut56:1481–1482
- Kooij IA, Sahami S, Meijer SL, Buskens CJ, Te Velde AA. The immunology of the vermiform appendix: a review of the literature. Clin Exp Immunol. 2016 Oct;186(1):1-9.
- De Souza SC, da Costa SR. de Souza IG. Vermiform appendix: positions and length – a study of 377 cases and literature reviewApêndice vermiforme: posições e comprimento – estudo de 377 casos e revisão de literatura. J Coloproctology. 2015.
- Kacprzyk A, DroŚ J, Stefura T, Krzysztofik M, JasiŃska K, PĘdziwiatr M, Major P, K Hołda M. Variations and morphometric features of the vermiform appendix: A systematic review and meta-analysis of 114,080 subjects with clinical implications. Clin Anat. 2020 Jan;33(1):85-98.
- Bakar SM, Shamim M, Alam GM, Sarwar M. Negative correlation between age of subjects and length of the appendix in Bangladeshi males. Arch Med Sci. 2013 Feb 21;9(1):55-67.(License: CC BY-NC-ND 3.0)
- Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015 Sep 26;386(10000):1278-1287.
- Moris D, Paulson EK, Pappas TN. Diagnosis and Management of Acute Appendicitis in Adults: A Review. JAMA. 2021 Dec 14;326(22):2299-2311.
- Oh SJ, Pimentel M, Leite GGS, et al. Acute appendicitis is associated with appendiceal microbiome changes including elevated Campylobacter jejuni BMJ Open Gastroenterol. 2020;7(1):e000412.
- Andersson RE, Hugander A, Thulin AJ. Diagnostic accuracy and perforation rate in appendicitis: association with age and sex of the patient and with appendicectomy rate. Eur J Surg. 1992;158:37–41.
- Liang MK, Andersson RE, Jaffe BM, Berger DH. The Appendix. In: Brunicardi F, Andersen DK, Billiar TR, Dunn DL, Hunter JG, Matthews JB, Pollock RE. eds. Schwartz’s Principles of Surgery, 10e. McGraw Hill; 2015.
- Erin C Howell, Emily D Dubina & Steven L Lee (2018) Perforation risk in pediatric appendicitis: assessment and management, Pediatric Health, Medicine and Therapeutics, 9:135-145.
- Zvizdic Z, Golos AD, Milisic E, Jonuzi A, Zvizdic D, Glamoclija U, Vranic S. The predictors of perforated appendicitis in the pediatric emergency department: A retrospective observational cohort study. Am J Emerg Med. 2021 Nov;49:249-252.
- Neilson IR, Laberge JM, Nguyen LT, et al. Appendicitisin children: Current therapeutic recommendations. J Pediatr Surg 1990; 25:1113–1116.
- Rasmussen OO, Hoffmann J. Assessment of the reliability of the symptoms and signs of acute appendicitis. J R Coll Surg Edinb. 1991;36:372–377.
- Kulvatunyou N, Zimmerman SA, Joseph B, Friese RS, Gries L, O’Keeffe T, Stroster JA, Tang AL. Risk Factors for Perforated Appendicitis in the Acute Care Surgery Era-Minimizing the Patient’s Delayed Presentation Factor. J Surg Res. 2019 Jun;238:113-118.
- United Kingdom National Surgical Research Collaborative; Bhangu A. Safety of short, in-hospital delays before surgery for acute appendicitis: multicentre cohort study, systematic review, and meta-analysis. Ann Surg. 2014 May;259(5):894-903.
- J J Atema, C C van Rossem, M M Leeuwenburgh, J Stoker, M A Boermeester, Scoring system to distinguish uncomplicated from complicated acute appendicitis, British Journal of Surgery, Volume 102, Issue 8, July 2015, Pages 979–990
- Miyauchi, H., Okata, Y., Hatakeyama, T., Nakatani, T., Nakai, Y. and Bitoh, Y. (2020), Analysis of predictive factors for perforated appendicitis in children. Pediatrics International, 62: 711-715.
- Kulvatunyou N, Zimmerman SA, Joseph B, Friese RS, Gries L, O’Keeffe T, Stroster JA, Tang AL. Risk Factors for Perforated Appendicitis in the Acute Care Surgery Era-Minimizing the Patient’s Delayed Presentation Factor. J Surg Res. 2019 Jun;238:113-118.
- Yamazaki S, Shimodaira Y, Kobayashi A, Takata M, Hayashibara K, Sakon M, Sekino Y, Okada M, Takahashi Y, Shimura M, Seki H, Soejima Y. Predictive factors of perforated appendicitis: Impact of the C-reactive protein level. Surg Open Sci. 2021 Jun 30;6:1-4.
- Wheeler N, Steel HC, Setlai BDP, Meintjes F, Mokoena T. Human immunodeficiency virus infection is associated with a differential increase in cytokine response and increased risk of perforation in acute appendicitis. Br J Surg. 2021 May 27;108(5):463-468.
- Drake FT, Mottey NE, Farrokhi ET, Florence MG, Johnson MG, Mock C, Steele SR, Thirlby RC, Flum DR. Time to appendectomy and risk of perforation in acute appendicitis. JAMA Surg. 2014 Aug;149(8):837-44.
- S T van Dijk, A H van Dijk, M G Dijkgraaf, M A Boermeester, Meta-analysis of in-hospital delay before surgery as a risk factor for complications in patients with acute appendicitis, British Journal of Surgery, Volume 105, Issue 8, July 2018, Pages 933–945
- Ditillo MF, Dziura JD, Rabinovici R. Is it safe to delay appendectomy in adults with acute appendicitis? Ann Surg. 2006 Nov;244(5):656-60.
- Di Saverio S, Podda M, De Simone B, Ceresoli M, Augustin G, Gori A, Boermeester M, Sartelli M, Coccolini F, Tarasconi A, De’ Angelis N, Weber DG, Tolonen M, Birindelli A, Biffl W, Moore EE, Kelly M, Soreide K, Kashuk J, Ten Broek R, Gomes CA, Sugrue M, Davies RJ, Damaskos D, Leppäniemi A, Kirkpatrick A, Peitzman AB, Fraga GP, Maier RV, Coimbra R, Chiarugi M, Sganga G, Pisanu A, De’ Angelis GL, Tan E, Van Goor H, Pata F, Di Carlo I, Chiara O, Litvin A, Campanile FC, Sakakushev B, Tomadze G, Demetrashvili Z, Latifi R, Abu-Zidan F, Romeo O, Segovia-Lohse H, Baiocchi G, Costa D, Rizoli S, Balogh ZJ, Bendinelli C, Scalea T, Ivatury R, Velmahos G, Andersson R, Kluger Y, Ansaloni L, Catena F. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.
- Stewart B, Khanduri P, McCord C, Ohene-Yeboah M, Uranues S, Vega Rivera F, Mock C. Global disease burden of conditions requiring emergency surgery. Br J Surg. 2014 Jan;101(1):e9-22.
- Guidry SP, Poole GV. The anatomy of appendicitis. Am Surg. 1994;60(1):68-71.
- Punguyire D, Iserson VK. Missed appendicitis after self-induced abortion. Pan Afr Med J. 2011;10:38. Epub 2011 Nov 13. (License: CC BY 2.0)
- Smith MP, Katz DS, Lalani T, et al. ACR Appropriateness Criteria® right lower quadrant pain—suspected appendicitis. Ultrasound Q. 2015;31(2):85-91.
- Garcia EM, Camacho MA, Karolyi DR, et al; Expert Panel on Gastrointestinal Imaging. ACR Appropriateness Criteria®right lower quadrant pain—suspected appendicitis. J Am Coll Radiol. 2018;15(11S):S373-S387.
- Rao PM, Rhea JT, Novelline RA, Mostafavi AA, McCabe CJ. Effect of computed tomography of the appendix on treatment of patients and use of hospital resources. N Engl J Med. 1998;338(3):141-146.
- Gorter RR, Eker HH, Gorter-Stam MA, et al. Diagnosis and management of acute appendicitis: EAES consensus development conference 2015. Surg Endosc. 2016;30(11):4668-4690.
- Ranieri DM, Enzerra MD, Pickhardt PJ. Prevalence of appendicoliths detected at CT in adults with suspected appendicitis. AJR Am J Roentgenol. 2021;216(3):677-682.
- Velez DR. Appendicitis. The Operative Review of Surgery. 2023.
- Vasileiou G., Ray-Zack M., Zielinski M., Qian S., Yeh D.D., Crandall M. Validation of the American Association for the Surgery of Trauma emergency general surgery score for acute appendicitis—An EAST multicenter study. Trauma Acute Care Surg. 2019;87:134–139.
- Alvarado A. “A practical score for the early diagnosis of acute appendicitis,” Annals of Emergency Medicine, vol. 15, no. 5, pp. 557–564, 1986.
- McKay R, Shepherd J. The use of the clinical scoring system by Alvarado in the decision to perform computed tomography for acute appendicitis in the ED. Am J Emerg Med. 2007 Jun;25(5):489-93.
- Samuel M. Pediatric appendicitis score. J Pediatr Surg. 2002 Jun;37(6):877-81.
- Shah SR, Sinclair KA, Theut SB, Johnson KM, Holcomb GW 3rd, St Peter SD. Computed Tomography Utilization for the Diagnosis of Acute Appendicitis in Children Decreases With a Diagnostic Algorithm. Ann Surg. 2016 Sep;264(3):474-81.
- Von-Mühlen B, Franzon O, Beduschi MG, Kruel N, Lupselo D. AIR score assessment for acute appendicitis. Arq Bras Cir Dig. 2015 Jul-Sep;28(3):171-3.
- Chong CF, Adi MI, Thien A, Suyoi A, Mackie AJ, Tin AS, Tripathi S, Jaman NH, Tan KK, Kok KY, Mathew VV, Paw O, Chua HB, Yapp SK. Development of the RIPASA score: a new appendicitis scoring system for the diagnosis of acute appendicitis. Singapore Med J. 2010 Mar;51(3):220-5.
- Eskelinen M, Ikonen J, Lipponen P. Contributions of history-taking, physical examination, and computer assistance to diagnosis of acute small-bowel obstruction. A prospective study of 1333 patients with acute abdominal pain. Scand J Gastroenterol. 1994;29:715–721.
- Ohmann C, Yang Q, Franke C. Diagnostic scores for acute appendicitis. Abdominal Pain Study Group. Eur J Surg. 1995;161:273–281.
- Tzanakis NE, Efstathiou SP, Danulidis K, Rallis GE, Tsioulos DI, Chatzivasiliou A, Peros G, Nikiteas NI. A new approach to accurate diagnosis of acute appendicitis. World J Surg. 2005 Sep;29(9):1151-6, discussion 1157.
- Lintula H, Kokki H, Kettunen R, Eskelinen M. Appendicitis score for children with suspected appendicitis. A randomized clinical trial. Langenbecks Arch Surg. 2009 Nov;394(6):999-1004.
- Enochsson L, Gudbjartsson T, Hellberg A, Rudberg C, Wenner J, Ringqvist I, et al. The Fenyö-Lindberg scoring system for appendicitis increases positive predictive value in fertile women—a prospective study in 455 patients randomized to either laparoscopic or open appendectomy. Surg Endosc Other Interv Tech. 2004;18:1509–1513.
- Karaman K, Ercan M, Demir H, Yalkın Ö, Uzunoğlu Y, Gündoğdu K, et al. The Karaman score: a new diagnostic score for acute appendicitis. Ulus Travma Acil Cerrahi Derg. 2018;24:545–551.
- Strzałka M, Matyja M, Rembiasz K. Comparison of the results of laparoscopic appendectomies with application of different techniques for closure of the appendicular stump. World J Emerg Surg. 2016 Jan 6;11:4. (License: CC BY 4.0)
- Sawyer RG, Claridge JA, Nathens AB, Rotstein OD, Duane TM, Evans HL, Cook CH, O’Neill PJ, Mazuski JE, Askari R, Wilson MA, Napolitano LM, Namias N, Miller PR, Dellinger EP, Watson CM, Coimbra R, Dent DL, Lowry SF, Cocanour CS, West MA, Banton KL, Cheadle WG, Lipsett PA, Guidry CA, Popovsky K; STOP-IT Trial Investigators. Trial of short-course antimicrobial therapy for intraabdominal infection. N Engl J Med. 2015 May 21;372(21):1996-2005.
- Fagenholz PJ, Peev MP, Thabet A, Michailidou M, Chang Y, Mueller PR, Hahn PF, Velmahos GC. Abscess due to perforated appendicitis: factors associated with successful percutaneous drainage. Am J Surg. 2016 Oct;212(4):794-798.
- Teh SH, O’Ceallaigh S, Mckeon JG, O’Donohoe MK, Tanner WA, Keane FB. Should an appendix that looks ‘normal’ be removed at diagnostic laparoscopy for acute right iliac fossa pain? Eur J Surg. 2000 May;166(5):388-9.
- CODA Collaborative; Flum DR, Davidson GH, Monsell SE, Shapiro NI, Odom SR, Sanchez SE, Drake FT, Fischkoff K, Johnson J, Patton JH, Evans H, Cuschieri J, Sabbatini AK, Faine BA, Skeete DA, Liang MK, Sohn V, McGrane K, Kutcher ME, Chung B, Carter DW, Ayoung-Chee P, Chiang W, Rushing A, Steinberg S, Foster CS, Schaetzel SM, Price TP, Mandell KA, Ferrigno L, Salzberg M, DeUgarte DA, Kaji AH, Moran GJ, Saltzman D, Alam HB, Park PK, Kao LS, Thompson CM, Self WH, Yu JT, Wiebusch A, Winchell RJ, Clark S, Krishnadasan A, Fannon E, Lavallee DC, Comstock BA, Bizzell B, Heagerty PJ, Kessler LG, Talan DA. A Randomized Trial Comparing Antibiotics with Appendectomy for Appendicitis. N Engl J Med. 2020 Nov 12;383(20):1907-1919.
- Vons C, Barry C, Maitre S, Pautrat K, Leconte M, Costaglioli B, Karoui M, Alves A, Dousset B, Valleur P, Falissard B, Franco D. Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet. 2011 May 7;377(9777):1573-9.
- Eriksson S, Granström L. Randomized controlled trial of appendicectomy versus antibiotic therapy for acute appendicitis. Br J Surg. 1995 Feb;82(2):166-9.
- Styrud J, Eriksson S, Nilsson I, Ahlberg G, Haapaniemi S, Neovius G, Rex L, Badume I, Granström L. Appendectomy versus antibiotic treatment in acute appendicitis. a prospective multicenter randomized controlled trial. World J Surg. 2006 Jun;30(6):1033-7.
- Salminen P, Tuominen R, Paajanen H, Rautio T, Nordström P, Aarnio M, Rantanen T, Hurme S, Mecklin JP, Sand J, Virtanen J, Jartti A, Grönroos JM. Five-Year Follow-up of Antibiotic Therapy for Uncomplicated Acute Appendicitis in the APPAC Randomized Clinical Trial. JAMA. 2018 Sep 25;320(12):1259-1265.
- Sakran JV, Mylonas KS, Gryparis A, Stawicki SP, Burns CJ, Matar MM, et al. Operation versus antibiotics – The “appendicitis conundrum” continues: A meta-analysis. J Trauma Acute Care Surg. 2017;82:1129–37.
- Simillis C, Symeonides P, Shorthouse AJ, Tekkis PP. A meta-analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon). Surgery. 2010 Jun;147(6):818-29.
- Blakely ML, Williams R, Dassinger MS, Eubanks JW 3rd, Fischer P, Huang EY, Paton E, Culbreath B, Hester A, Streck C, Hixson SD, Langham MR Jr. Early vs interval appendectomy for children with perforated appendicitis. Arch Surg. 2011 Jun;146(6):660-5.
- Peltrini R, Cantoni V, Green R, Lionetti R, D’Ambra M, Bartolini C, De Luca M, Bracale U, Cuocolo A, Corcione F. Risk of appendiceal neoplasm after interval appendectomy for complicated appendicitis: A systematic review and meta-analysis. Surgeon. 2021 Dec;19(6):e549-e558.
- Davis CR, Trevatt A, Dixit A, Datta V. Systematic review of clinical outcomes after prophylactic surgery. Ann R Coll Surg Engl. 2016 Jul;98(6):353-7.
- Fisher KS, Ross DS. Guidelines for therapeutic decision in incidental appendectomy. Surg Gynecol Obstet. 1990 Jul;171(1):95-8.
- Andersson RE, Lambe M. Incidence of appendicitis during pregnancy. Int J Epidemiol. 2001 Dec;30(6):1281-5.
- Bickell NA, Aufses AH Jr, Rojas M, Bodian C. How time affects the risk of rupture in appendicitis. J Am Coll Surg. 2006 Mar;202(3):401-6.
- Weingold AB. Appendicitis in pregnancy. Clin Obstet Gynecol. 1983 Dec;26(4):801-9.
- Zingone F, Sultan AA, Humes DJ, West J. Risk of acute appendicitis in and around pregnancy: a population-based cohort study from England. Ann Surg. 2015 Feb;261(2):332-7.
- Silvestri MT, Pettker CM, Brousseau EC, Dick MA, Ciarleglio MM, Erekson EA. Morbidity of appendectomy and cholecystectomy in pregnant and nonpregnant women. Obstet Gynecol. 2011 Dec;118(6):1261-1270.
- McGory ML, Zingmond DS, Tillou A, Hiatt JR, Ko CY, Cryer HM. Negative appendectomy in pregnant women is associated with a substantial risk of fetal loss. J Am Coll Surg. 2007 Oct;205(4):534-40.
- Babaknia A, Parsa H, Woodruff JD. Appendicitis during pregnancy. Obstet Gynecol. 1977 Jul;50(1):40-4.
- Choi JJ, Mustafa R, Lynn ET, Divino CM. Appendectomy during pregnancy: follow-up of progeny. J Am Coll Surg. 2011 Nov;213(5):627-32.
- Mourad J, Elliott JP, Erickson L, Lisboa L. Appendicitis in pregnancy: new information that contradicts long-held clinical beliefs. Am J Obstet Gynecol. 2000 May;182(5):1027-9.
- Hodjati H, Kazerooni T. Location of the appendix in the gravid patient: a re-evaluation of the established concept. Int J Gynaecol Obstet. 2003 Jun;81(3):245-7.
- Pates JA, Avendiano TC, Zaretsky MV, McIntire DD, Twickler DM. The appendix in pregnancy: confirming historical observations with a contemporary modality. Obstet Gynecol. 2009 Oct;114(4):805-808.
- House JB, Bourne CL, Seymour HM, Brewer KL. Location of the appendix in the gravid patient. J Emerg Med. 2014 May;46(5):741-4.
- Lurie S, Rahamim E, Piper I, Golan A, Sadan O. Total and differential leukocyte counts percentiles in normal pregnancy. Eur J Obstet Gynecol Reprod Biol. 2008 Jan;136(1):16-9.
- Prodromidou A, Machairas N, Kostakis ID, Molmenti E, Spartalis E, Kakkos A, Lainas GT, Sotiropoulos GC. Outcomes after open and laparoscopic appendectomy during pregnancy: A meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2018 Jun;225:40-50.
- Walsh CA, Tang T, Walsh SR. Laparoscopic versus open appendicectomy in pregnancy: a systematic review. Int J Surg. 2008 Aug;6(4):339-44.
- Xu Y, Jeffrey RB, DiMaio MA, Olcott EW. Lymphoid Hyperplasia of the Appendix: A Potential Pitfall in the Sonographic Diagnosis of Appendicitis. AJR Am J Roentgenol. 2016 Jan;206(1):189-94.
- Aydin S, Tek C, Ergun E, Kazci O, Kosar PN. Acute Appendicitis or Lymphoid Hyperplasia: How to Distinguish More Safely? Can Assoc Radiol J. 2019 Nov;70(4):354-360.
- Helbling R, Conficconi E, Wyttenbach M, Benetti C, Simonetti GD, Bianchetti MG, Hamitaga F, Lava SA, Fossali EF, Milani GP. Acute Nonspecific Mesenteric Lymphadenitis: More Than “No Need for Surgery”. Biomed Res Int. 2017;2017:9784565.
- Mesenteric Lymphadenitis. Mayo Clinic. 2021. https://www.mayoclinic.org/diseases-conditions/mesenteric-lymphadenitis/symptoms-causes/syc-20353799
- Chaudhary P, Nabi I, Arora MP. Periappendicitis: our 13 year experience. Int J Surg. 2014;12(9):1010-3.
- Valentino loses battle with death: Greatest of screen lovers fought valiantly for life. The Plattsburgh Sentinel. 1926;1