Breast: Lymph Node Management
Lymph Node Management
Specific Lymph Node Concerns
- Suspicious Lymph Node Found on Physical Exam: US & FNA Prior to Surgery
- Supraclavicular Lymph Node: Chemotherapy, Radiation Therapy & Resect the Primary Breast Lesion
- Resect Lymph Node Only if Not Fully Treated
Lymph Node Metastases
- Isolated Tumor Cells (ITC): < 0.2 mm
- Micrometastases: 0.2-2.0 mm
- Slightly Worse Prognosis
- May Predict Recurrence (Debated)
- Micrometastases: ≥ 2.0 mm
- Significantly Effects Survival
Sentinel Lymph Node Biopsy (SLNB)
- Definition: Surgical Removal of Axillary Sentinel Lymph Nodes
- Indications:
- Invasive Carcinoma if Early (T1 or T2) with Clinically Negative Nodes
- DCIS if Mastectomy is Performed
- Contraindications:
- Clinically Positive Nodes
- Inflammatory Breast Cancer
- Locally Advanced Disease (T3 or T4)
- May Still Consider SLNB for T3 Disease (Debated)
- Debated Contraindications
- Large Tumors (T3)
- After Neoadjuvant Chemotherapy
- Prior Axillary Surgery
- False Negative Rate: 5-10%
Axillary Lymph Node Dissection (ALND)
- Definition: Surgical Removal of Axillary Lymph Node Levels I & II
- Does Not Include Level III
- Indications:
- If SLNB is Contraindicated
- After SLNB If:
- No Radiotracer/Dye is Found (Rate < 5%)
- ≥ 3 Positive Lymph Nodes are Pathologically Confirmed (ACOSOG Z0011 Trial)
- *Specifically Referring to Lumpectomy
- Any Positive Lymph Nodes After a Mastectomy – Debated
Complications
- Decreased Arm Range-of-Motion (40%) – Most Common Complication After Axillary Surgery
- Infection (7%)
- Hematoma (2-10%)
- Seroma
- Nerve Injury (< 1%)
- Arm Swelling
- Sudden/Early: Concern for Axillary Vein Thrombosis
- Slow/Late: Concern for Lymphatic Fibrosis
- Lymphedema
- SLNB Risk: < 5%
- ALND Risk: 20%
- Stewart-Treves Syndrome
- Lymphangiosarcoma Due to Chronic Lymphedema
- *See Vascular: Lymphatic Pathology
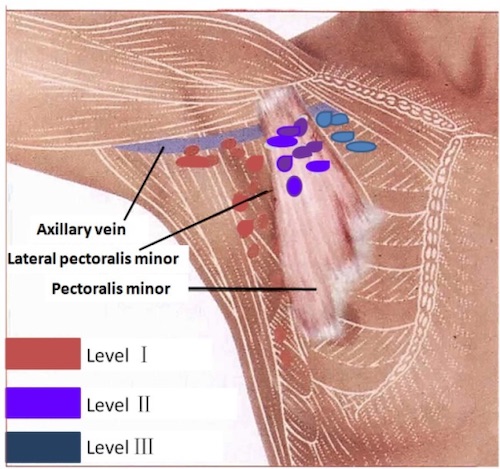
Axillary Lymph Nodes Levels 1
Sentinel Lymph Node Biopsy (SLNB)
Injection
- Agents:
- 1% Isosulfan Blue Dye
- Inject 3-5 cc & Massage the Area for 5 Minutes to Dilate Lymphatics
- Creates a Visible Blue Tint to the Node
- Teratogenic & Contraindicated in Pregnancy
- Can Cause a Severe Anaphylactic Reaction (0.7-1.1%)
- Radiotracer (Technetium-99)
- 0.5 mCi Injected the Day of Surgery
- Identified Using a Gamma Probe Intraoperatively
- Safe in Pregnancy
- Using Both Dye & Radiotracer Results in Highest Success Rates
- 1% Isosulfan Blue Dye
- Injection Locations:
- Around the Tumor Periphery (Not into the Tumor Itself – Lymphatics May Be Occluded)
- Palpable Edge of the Biopsy Cavity
- Sappey Plexus
Retrieval Indications
- Dye: Retrieve All Nodes That Have Taken Up Dye
- Radiotracer: Retrieve All Nodes with > 10% the Highest Ex-Vivo Count
- Ex-Vivo Count – Count of the Highest Lymph Node Once Removed from the Body
- Retrieve Any Firm Node (Regardless of Dye/Radiotracer)
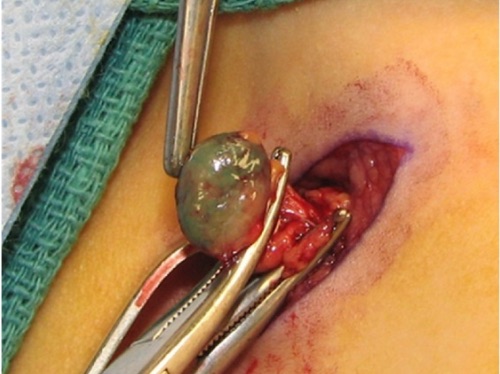
Blue Node 2
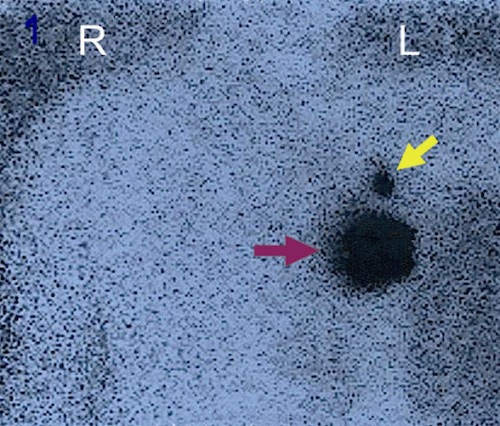
Breast Lymphoscingigraphy; Injection Site (Red Arrow), One Sentinel Lymph Node (Yellow Arrow) 3
Axillary Lymph Node Dissection (ALND)
Borders Mn
- Superior: Axillary Vein
- Inferior: Tail of Breast
- Medial: Serratus Anterior
- Lateral: Latissimus Dorsi
Procedure
- Positioning
- Supine
- Arms Abducted ≤ 90 Degrees (> 90 Degrees Increases Risk of Stretching Brachial Plexus)
- Incision
- If Performed During a Lumpectomy or Only ALND:
- Curvilinear Incision
- 1-2 cm Below Axillary Hair Line
- Extend from Anterior to Posterior Axillary Folds
- If Performed During a Modified Radical Mastectomy:
- Attempt to Use Same Mastectomy Incision
- Extend Laterally if Needed
- Separate Incision if Not Able
- If Performed During a Lumpectomy or Only ALND:
- Define Borders
- Define Pectoralis Major (Anterior)
- Take Care to Preserve the Medial Pectoral Neurovascular Bundle (Found Through or Lateral to the Pectoralis Minor)
- Define Latissimus Dorsi (Lateral)
- Extend Inferiorly Until It Pulls to the Chest Wall
- Extend Superiorly to the Insertion
- Take Care to Preserve the Intercostobrachial Nerve (Crosses 1-2 cm Below the Axillary Vein)
- Visualize Axillary Vein (Superior)
- Divide Clavipectoral Fascia
- Extend Posteriorly to Visualize the Vessel
- Bifurcations are Frequent – Never Ligate Transverse Veins High in Axilla
- Do Not Skeletonize or Open the Sheath Unless Indicated (Increases Lymphedema Risk)
- Define Pectoralis Major (Anterior)
- Identify & Protect Nerves
- Intercostobrachial Nerve – Lateral by the Latissimus Dorsi 1-2 cm Below Axillary Vein
- If Unable to Spare: Sharply Ligate
- Long Thoracic Nerve – Along the Lateral Chest Wall
- Found Just Below Medial Axillary Vein & Extending Inferiorly
- Do Not Incise Fascia of Serratus Anterior
- Thoracodorsal Nerve – Along the Mid-Axilla with the Associated Neurovascular Bundle
- Found Just Below the Mid-Axillary Vein
- Intercostobrachial Nerve – Lateral by the Latissimus Dorsi 1-2 cm Below Axillary Vein
- Dissection
- Mobilize Fat Pad by Blunt Dissection
- Dissect to Defined Borders
- Medial: Serratus Anterior
- Lateral: Latissimus Dorsi
- Superior: Axillary Vein
- Inferior: Tail of Breast
- Include Level I & Level II Nodes
- Closure
- Secure Hemostasis
- Place a JP Drain (Debated)
Axillary Lymph Node Dissection (ALND) 4
Mnemonics
Borders of an ALND
- Medial (M): Think ‘M’ Shaped Serrations Over the Lateral Chest Wall (Serratus Anterior)
- Lat-Lat: Latissimus Dorsi is Lateral
References
- Lu Q, Hua J, Kassir MM, Delproposto Z, Dai Y, Sun J, Haacke M, Hu J. Imaging lymphatic system in breast cancer patients with magnetic resonance lymphangiography. PLoS One. 2013 Jul 5;8(7):e69701. (License: CC Not Specified)
- Carson J, Bedrnicek J, Abdessalam S. Radiographically negative, asymptomatic, sentinel lymph node positive cutaneous T-cell lymphoma in a 3-year-old male: a case report. Case Rep Pediatr. 2012;2012:791602. (License: CC BY-3.0)
- Mathelin C, Salvador S, Croce S, Andriamisandratsoa N, Huss D, Guyonnet JL. Optimization of sentinel lymph node biopsy in breast cancer using an operative gamma camera. World J Surg Oncol. 2007 Nov 17;5:132. (License: CC BY-2.0)
- Soares EW. Anatomical variations of the axilla. Springerplus. 2014 Jun 24;3:306. (License: CC BY-4.0)