Vascular: Carotid Artery Stenosis
Carotid Artery Stenosis
Basics
- Most Common Site: Bifurcation
Presentation
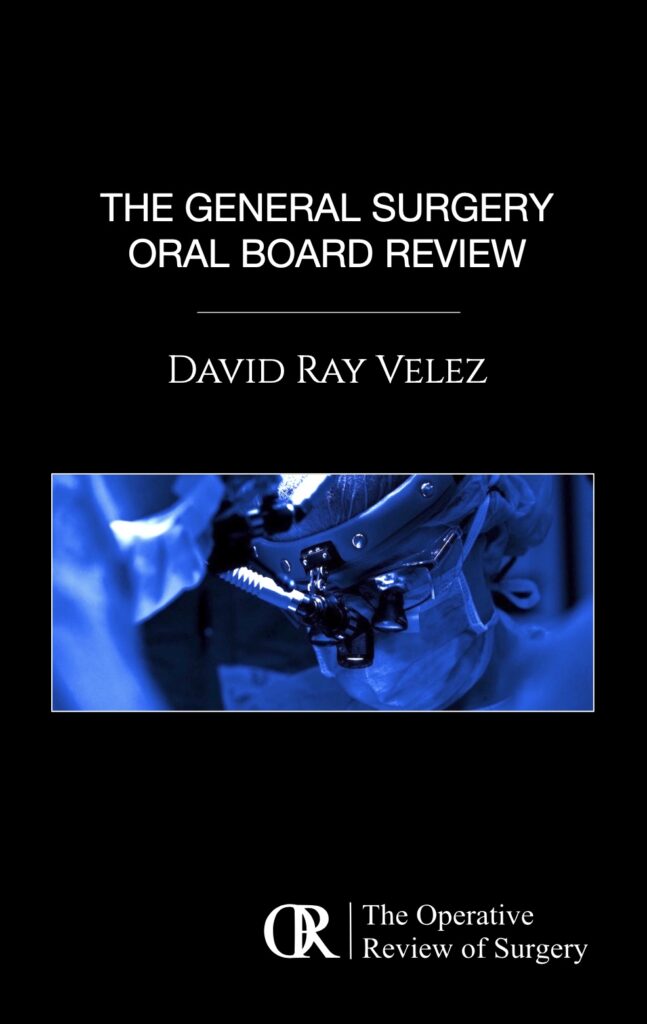
- Amaurosis Fugax – Transient Vision Changes to Ipsilateral Eye
- From Occlusion of the Ophthalmic Artery (First Branch of ICA)
- Cholesterol Embolus (Hollenhorst Plaque) Seen on Eye Exam
- Transient Ischemic Attacks (TIA)
- Ischemic Stroke
Characteristics with Increased Risk of Stroke
- Plaque Characteristics:
- Diameter/Area
- Progression
- Echolucent
- Ulceration
- Fibrous Cap Disruption
- Inflammation by MRI
- Patient Characteristics:
- Neurologic Symptoms
- Contralateral Carotid Occlusion (CCO)
- Past Contralateral Stroke
- Renal Insufficiency
- Smoking
- Clinically Silent Emboli
General Risk of Stroke (ACAS/NASCET Study Findings)
- Asymptomatic > 60% Stenosis:
- Medical Therapy: 11% at 5 Years
- CEA: 5.1% at 5 Years
- Symptomatic 50-69% Stenosis:
- Medical Therapy: 22.2% at 2 Years
- CEA: 15.7% at 2 Years
- Symptomatic > 70% Stenosis:
- Medical Therapy: 26% at 2 Years
- CEA: 9% at 2 Years

Carotid Plaque 1
Hollenhorst Plaque 2
Diagnosis
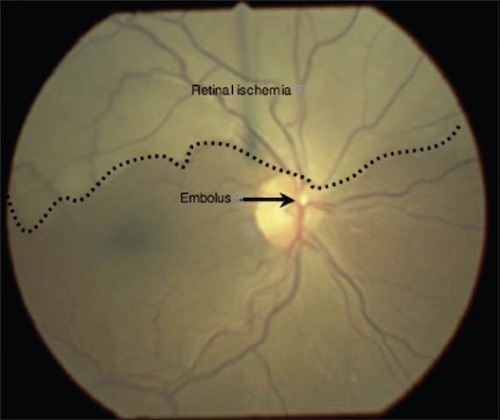
- First Line Imaging Modality: Duplex US
- Good for Stenosis 70-99% But Less Sensitive for Stenosis 50-69%
- Based Primarily on Velocities Opposed to Visualization of the Physical Plaque
- Ultrasound Criteria (Society of Radiologists in Ultrasound):
| Degree of Stenosis | Primary Parameters | Secondary Parameters | ||
| ICA PSV | Plaque Estimate | ICA/CCA PSV Ratio | ICA EDV | |
| Normal | < 125 cm/s | None | < 2.0 | < 40 cm/s |
| < 50% | < 125 cm/s | < 50% | < 2.0 | < 40 cm/s |
| 50-69% | 125-230 cm/s | ≥ 50% | 2.0-4.0 | 40-100 cm/s |
| > 70% | > 230 cm/s | ≥ 50% | > 4.0 | > 100 cm/s |
| Near Occlusion | High, Low or Undetectable | Visible | Variable | Variable |
| Total Occlusion | Undetectable | Visible with No Detectable Lumen | Not Applicable | Not Applicable |
- *ICA – Internal Carotid Artery, CCA – Common Carotid Artery, PSV – Peak Systolic Velocity, EDV – End Diastolic Velocity
- CTA Indicated if Concern for Anatomy:
- High Bifurcation
- Reoperative CEA
- Planned Carotid Stenting – US Alone Not Sufficient
- Gold Standard: Angiography
Normal ICA on Duplex US 3
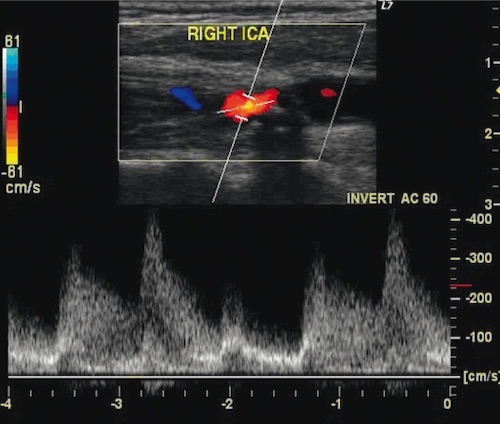
ICA Stenosis on Duplex US 3
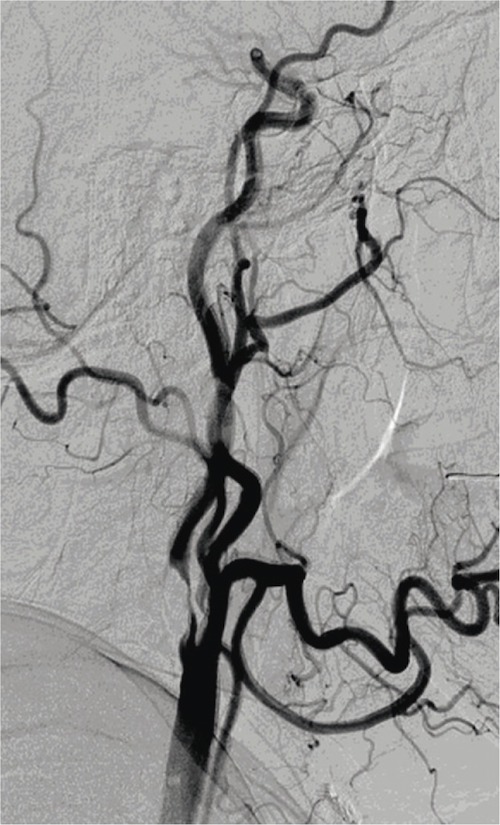
ICA Stenosis on Angiography 3
Treatment
General Treatment Approach
- Asymptomatic:
- < 80% Stenosis: Medical Therapy
- 80-99% Stenosis: Carotid Endarterectomy (CEA) vs Carotid Artery Stenting (CAS)
- *Cutoff is Debated and Older Major Studies Had Recommended 60%
- Symptomatic:
- < 50% Stenosis: Medical Therapy
- 50-99% Stenosis: Carotid Endarterectomy (CEA) vs Carotid Artery Stenting (CAS)
- Timing Post CVA:
- Fluctuating Neuro Status & Evolving TIA: Emergent
- TIA or Non-Disabling: < 2 Weeks
- Too Early (< 24 Hours) – Risk Reperfusion Injury
- Moderate-Large Stroke or Midline Shift: 4-6 Weeks
- Higher Reperfusion Risk
- Hemorrhagic Stroke: 6-8 Weeks
- Completely Disabling: None
- 100% Occlusion: Anticoagulation
- Do Not Open, Risk Reperfusion Injury
- May Consider Repair at a Lower Percentage if Ulcerated (Higher Risk)
Medical Therapy
- Antihypertensive Therapy
- Statin Therapy
- Antiplatelet Therapy
- Smoking Cessation
Carotid Endarterectomy (CEA)
- Stenosis Benefit of Major Studies:
- Symptomatic:
- NASCET: > 70%; > 50% to Lesser Degree
- ECST: > 60%
- Asymptomatic:
- ACAS: > 60%
- ACST: > 60%
- *Medical Managements were Outdated and Cutoff more Debated – Some Recommend as High as 80%
- Symptomatic:
- Contraindications:
- Poor Baseline Functional Status with No Benefit
- Short Life Expectancy
- Less Benefit in Women & Asymptomatic Disease
Carotid Artery Stenting (CAS)
- Potential Indications:
- “Hostile Neck” (Effected by Prior Radiation, Stoma or Surgery)
- Recurrent Stenosis
- High Lesions (Above C2 Vertebrae) – Avoid Mandibular Subluxation Required for Open CEA
- Low Lesions (Below Clavicle)
- Potential Contraindications:
- Symptomatic Disease – Inferior Outcomes to CEA
- Vessel Tortuosity
- Adverse Lesion Characteristics:
- Length > 15 mm
- Echolucent
- Circumferential Lesion
- Preocclusive Lesion
- Tandem Lesions
- Comparison to CEA (CREST Trial):
- Similar Overall Rates of Stroke, MI & Death
- CAS Has Higher Rates of Perioperative Stroke (4.1% vs 2.3%)
- CEA Has Higher Rates of Perioperative MI (2.3% vs 1.1%)
References
- Uthman E. Wikimedia Commons. (License: CC BY-2.0)
- Jones RG, Peall A. Sudden unilateral visual field loss. J Emerg Trauma Shock. 2009 Sep;2(3):211-2. (License: CC BY-NC-SA-3.0)
- Szczerbo-Trojanowska M, Jargiełło T, Drelich-Zbroja A. Management of carotid stenosis. History and today. J Ultrason. 2013 Mar;13(52):6-20. (License: CC BY-NC-ND-3.0)