Carotid Endarterectomy (CEA)
Derek Edward Jones, MD
The Operative Review of Surgery. 2023; 1:243-252.
Table of Contents
Indications
Definition
- Open Surgery to Remove Plaque from the Carotid Artery
- Goal: Prevent Future Stroke
Indications
- Indicated for Carotid Artery Stenosis
- Cutoff Values:
Contraindications
- Absolute Contraindications:
- Asymptomatic Complete Occlusion – The Only Absolute Contraindication
- Relative Contraindications:
- “Hostile Neck” (Prior Neck Radiation, Tracheostomy, or Surgery)
- Contralateral Vocal Cord Paralysis
- High Lesions (Above C2 Vertebrae) – Avoid Mandibular Subluxation Required for Open CEA
- Low Lesions (Below Clavicle)
- Recurrent Severe Stenosis
- High Surgical Risk
- *May Consider Carotid Artery Stenting for Patient with Relative Contraindications Instead
Bilateral Repairs
- Combined Surgery (Bilateral Repair in Same Surgery) is Generally Contraindicated
- Generally Perform a Staged Repair if Indicated
- Repair the Symptomatic Side First
- If Asymptomatic: Repair the Side with Greatest Stenosis First
- If Both Sides Equal: Perform the Dominant Side First
- Evaluate for Vocal Cord Paralysis Prior to Proceeding with the Second Side
Technique
Positioning
- Neck Extended, Often Using a Bump Under the Shoulders
- Neck Rotated to the Contralateral Side
- Arms at the Side
- Standard Incision: Longitudinal Along the Medial Border of the Sternocleidomastoid Muscle (SCM)
- Transverse Incision: 1-2 cm Below the Angle of the Jaw
- Technically May Be More Difficult
- Primarily Used for Cosmesis
- Expose the Carotid Sheath
- Divide Platysma
- Mobilize Medial Border of SCM
- *Avoid Injury to External Jugular Vein
- *Avoid Injury to Greater Auricular Nerve
- Enter the Carotid Sheath
- Minimize Carotid Artery Manipulation (Embolization Risk)
- Dissect Medial Border of the Internal Jugular Vein
- Divide Facial Vein (Seen Crossing Medially)
- Retract Internal Jugular Vein Laterally
- *Identify and Preserve the Vagus Nerve (Generally Posterior Between the IJ and Carotid; May Lie Anterior)
- Dissect the Carotid Artery
- Identify Common Carotid Artery (CCA), External Carotid Artery (ECA), and Internal Carotid Artery (ICA)
- Dissect ICA Past the Area of Stenosis
- Avoid Injury to the Carotid Body at the Bifurcation
- Identify Structures
- Ansa Cervicalis (Medial to CCA)
- Superior Thyroid Artery (Off Proximal ECA)
- Hypoglossal Nerve (Superior Extent)
- Control Inflow and Outflow Circumferentially (Vessel Loops, Rummel Tourniquet, or Vascular Clamps)
- Superior Thyroid Artery (First Branch of ECA) May Need to Be Controlled or Ligated
- Identify Common Carotid Artery (CCA), External Carotid Artery (ECA), and Internal Carotid Artery (ICA)
- Clamping: Mn
- Administer 70-100 U/kg Heparin Prior to Clamping
- Allow 3 Minutes for Circulation
- First Clamp ICA (Prevent Embolization to Brain)
- Ensure Clamping on a Normal Portion of Artery, Distal to Plaque
- Second Clamp CCA
- Third Clamp ECA
- Administer 70-100 U/kg Heparin Prior to Clamping
- Preform Endarterectomy
- Consider Shunt Placement – *See Below
- Close
- Close Platysma
- Close Skin
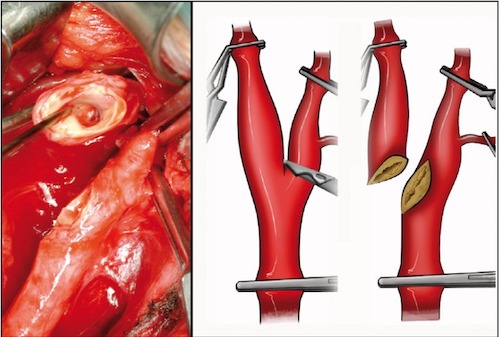
- Vertical Arteriotomy
- From CCA into ICA
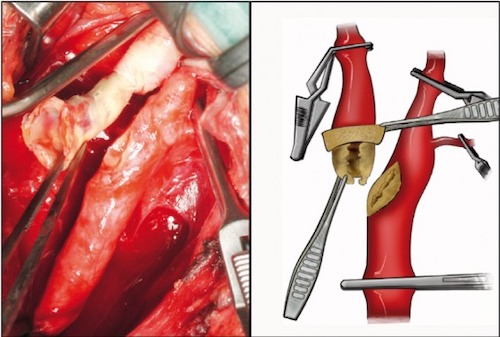
- Endarterectomy
- Begin Proximally in the CCA (Between Media and Adventitia)
- Remove Intima and Part of Media
- Continue Distally into the ICA
- Primary Concern: Ensure a Good Distal End Point
- Endpoint at Normal Intima with Gradual Tapering
- Extend into the ECA Orifice with Gradual Tapering
- Begin Proximally in the CCA (Between Media and Adventitia)
- Close with a Patch
- Options: Autologous, PTFE, Dacron, or Bovine
- Back Bleed Vessels and Irrigate with Heparinized Saline Prior to Final Closure
- Goal of a Patch: Prevent Narrowing and Restenosis
- *In General Patch Represents the Standard of Care Although Some Now Suggest Selective Patching if Diameter ≥ 6 mm (Debated) 3
- Release Clamps Mn
- First Release ICA Clamp Briefly to Back Bleed then Replace
- Then Release Clamps on ECA and CCA (Diverting Any Residual Air/Debris to ECA)
- Finally Remove the ICA Clamp
- Completely Transect the ICA at the Bifurcation
- ICA Adventitia is Then Everted Circumferentially (“Circumcised”) Off the Carotid Plaque
- Plaque is Then Removed from the CCA
- ICA is then Re-Anastomosed to the Bifurcation by Simple End-to-End Anastomosis
- No Patch Required
- *Similar Results and Complications Between Conventional and Eversion Techniques 4
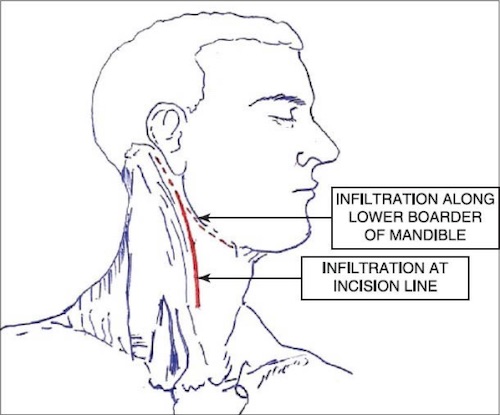
CEA Incisions; Standard (Solid Line) and Transverse (Dashed Line) 1
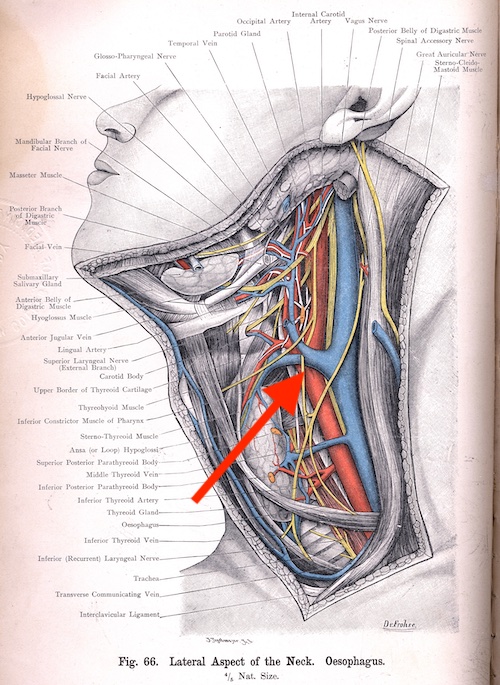
Facial Vein 2
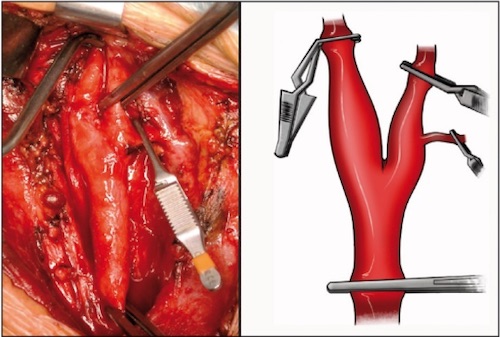
CEA Clamping (I.C.E.) 5
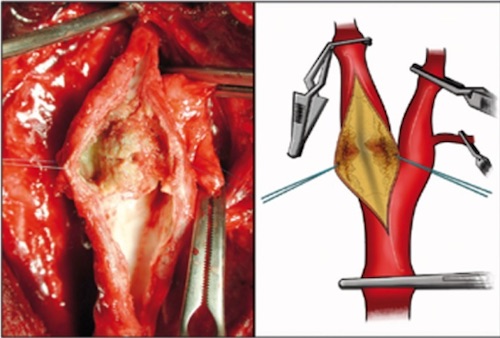
Conventional Endarterectomy 5
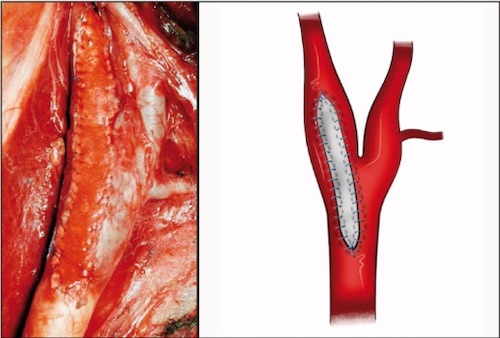
Patch Angioplasty 5
Eversion Arterial Transection 5
Eversion Endarterectomy 5
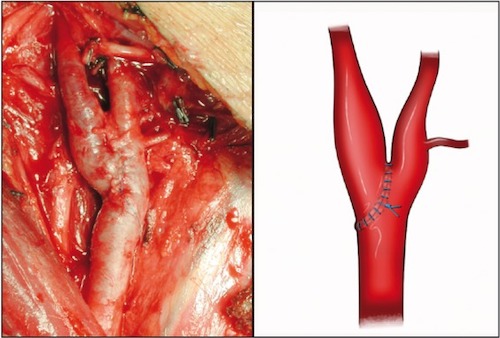
Eversion Closure 5
Shunting and Intraoperative Neuromonitoring
Shunting Definition
- Small Plastic Tube Used to Shunt Blood from the Common Carotid into the Internal Carotid Artery During Dissection
- Goal: Maintain Cerebral Perfusion
- Multiple Types of Commercially Available Shunts Exist
“Selective” Shunting Indications
- Any Evidence of Cerebral Ischemia
- Awake Patients Performed Under Local Anesthesia:
- Agitation
- Confusion
- Slurred Speech
- Weakness
- EEG Delta Waves or Disorganized Rhythms
- Carotid Stump Pressures (Mean Systolic Pressure < 50 mmHg) 6,7
Outcomes
- Routine Shunting (Compared to No Shunting): 8
- Lower Risk of Perioperative Stroke
- Lower Risk of Ipsilateral Stroke at 30 Days
- Lower Risk of Stroke-Related Death at 30 Days
- Selective Shunting (Compared to Routine Shunting): 9,10
- No Significant Difference
- Mostly Based on Surgeon Preference
Shunting Complications
- Plaque Dislodgement
- Intimal Flap/Dissection
- Air Embolism
Technique
- First Place Distal Segment into the Internal Carotid Artery
- Clamp to Prevent Blood Flow Around the Shunt
- Back Bleed to Clear Air and Debris
- Then Place Proximal Segment into the Common Carotid Artery
- Proceed with Endarterectomy
Complications
Mortality
- 30-Day All-Cause Mortality: 0.93% 11
- 40x Increased Risk After a Stroke 11
Perioperative Stroke
- Incidence: 2.15% 11
- Causes: 12,13
- Technical Causes:
- Residual Intimal Flap
- Thrombosis
- Plaque Emboli
- Platelet Aggregation
- Inadequate Cerebral Protection
- Improper Flushing
- Relative Hypotension
- Technical Causes:
- Mostly Reversible if Flow is Restored within 1-2 Hours
- Management: Immediate Reexploration in the OR vs Duplex Ultrasound (If Rapidly Available)
- Immediate Reexploration Often Recommended for a Presumed Intimal Flap or Thrombosis
- Other Evaluations if Duplex Negative:
- CT Head (Rule Out Hemorrhage)
- CTA Head and Neck
- Arteriography and Carotid Artery Stenting 14
Restenosis
- Risk: 2-10% 15-18
- *Historically Reported as High as 20% 19
- Causes: 20
- Immediate (< 4 Weeks): Technical Error
- Early (< 2 Years): Myointimal Hyperplasia
- Late (> 2 Years): Recurrent Atherosclerosis
- Treatment: 21
- Asymptomatic: Conservative Management vs Reintervention (Controversial)
- Symptomatic: Reintervention (Carotid Artery Stent vs Repeat CEA)
Myocardial Infarction (MI)
- Incidence: 0.87% 22
- Causes 25-50% of Perioperative Deaths
Cranial Nerve Injury (CNI) 23,34
- General Considerations:
- Most Are Transient and Resolve After 3-4 Weeks
- Overall Risk of Injury: 5-20%
- Risk of Permanent Injury: 0-1%
- Vagus Nerve Injury (Recurrent Laryngeal Nerve) (1-4%)
- The Most Feared/Dangerous Nerve Injury
- Location: Within the Carotid Sheath
- Presentation: Hoarseness (Vocal Cord Paralysis) and Dysphagia/Aspiration
- Typically Injured During Vascular Clamping
- Hypoglossal Nerve Injury (3-4%)
- Location: Just Above the Carotid Bifurcation
- Presentation: Speech and Mastication Deficit
- Tongue Deviates to the Ipsilateral Side of Injury
- Facial Nerve Injury (Marginal Mandibular Branch) (1-2%)
- Presentation: Smiling Deficit (Corner of Mouth Retraction)
- Typically Injured from Excessive Superior Retraction
- Glossopharyngeal Nerve Injury (0.2-0.5%)
- Presentation: Swallowing Difficulty
- Rare; Most Common with High Dissections
- Ansa Cervicalis Injury
- Presentation: Strap Muscle Deficits
- Greater Auricular Nerve Injury
- Presentation: Earlobe Numbness
Cerebral Hyperperfusion Syndrome (CHS)
- Definition: Impaired Autoregulation of Cerebral Perfusion After Chronic Hypoperfusion
- Increased Perfusion Causes Dilation of Vessels that are Unable to Appropriately Vasoconstrict – Result in Edema and Hemorrhage
- Risk: 0.75-3% 25
- Risk Factors: 25
- Preoperative High-Grade Stenosis (> 80%)
- Postoperative Hypertension
- Recent Contralateral CEA
- Contralateral Carotid Occlusion
- Intraoperative Ischemia
- Increased Peak Flow Velocity
- Low Stump Pressures (< 40 mmHg)
- Presentation: 26
- Hypertension
- Frontal Headache (Ipsilateral or Diffuse)
- Stroke and Seizure
- High Mortality (36-63%) 25
- Significant Morbidity (80%) Among Survivors 25
- Evaluate with Head CT or MRI for Potential Intracerebral Hemorrhage
- Management: Antihypertensives and Anti-Seizure Medications
- Strict Blood Pressure Control (< 140/90 mmHg) May Be Able to Prevent 27
Cervical Hematoma
- Incidence: 1-5% 28
- Risk Factors:
- Antiplatelet Therapy
- Non-Reversal of Heparin
- Most Often from Diffuse Oozing Rather than a Single Bleeding Site
- Creates a Risk Tracheal Compression and Airway Loss
- Treatment: Emergent Intubation and Immediate Reexploration/Evacuation in the OR
- Emergent Opening of the Incision with Hematoma Evacuation (As in Thyroidectomy) May Be Necessary if Airway Collapsing with Inability to Intubate
- *Note that There is Possibility of Graft Blowout that Requires Repair in the OR and Opening at Bedside Should Be Avoided Unless Emergently Necessary
Surgical Site Infection (SSI) 29-31
- Depth:
- Superficial SSI – Most Common
- Deep SSI Involving the Patch – Rare
- Presentation: Pain, Swelling, Fever, Erythema, and Drainage
- Management: Antibiotics and Drainage of Any Fluid Collection/Abscess
- If Fails, May Require Surgical Revision with Patch Excision and Carotid Ligation, Reconstruction, or Bypass
Post-Endarterectomy Pseudoaneurysm (PEPA) 32-34
- Rare (< 1%)
- Risk Factors:
- Suture Line Disruption
- Arterial Wall/Patch Degeneration
- Surgical Site Infection
- Clamp/Shunt-Induced Damage
- Complications: Rupture, Thrombus, Embolism, or Airway Compression
- Most Often Presents as a Pulsatile Mass
- Evaluate with Duplex US
- Other Options: CTA, MRI, or Angiography
- Treatment: Urgent Surgical Repair (Open or Endovascular)
Carotid Body Injury
- Can Result in Significant Hypertension
- Generally Transient
- Managed with Aggressive Blood Pressure Control to Prevent Cerebral Hyperperfusion Syndrome
Mnemonics
Clamping Order for CEA
- “I-C-E”
- ICA (First)
- CCA (Second)
- ECA (Last)
- Unclamp in the Opposite Order (E-C-I)
References
- Samanta S, Samanta S, Panda N, Haldar R. A unique anesthesia approach for carotid endarterectomy: Combination of general and regional anesthesia. Saudi J Anaesth. 2014 Apr;8(2):290-3. (License: CC BY-NC-SA 3.0)
- Bardeleben KH, Haeckel EH. Atlas of applied (topographical) human anatomy for students and practitioners. 1906. (License: Public Domain)
- Kapoor R, Evins AI, Marcus J, Rigante L, Kubota M, Stieg PE. Selective Patch Angioplasty and Intraoperative Shunting in Carotid Endarterectomy: A Single-Center Review of 141 Procedures. Cureus. 2015 Oct 28;7(10):e367.
- Cao P, Giordano G, De Rango P, Zannetti S, Chiesa R, Coppi G, Palombo D, Spartera C, Stancanelli V, Vecchiati E. A randomized study on eversion versus standard carotid endarterectomy: study design and preliminary results: the Everest Trial. J Vasc Surg. 1998 Apr;27(4):595-605.
- Chiesa R, Melissano G, Castellano R, Tshomba Y, Marone EM, Civilini E, Astore D, Calliari F, Catenaccio B, Coppi G, Carozzo A, Mennella R. Carotid Endarterectomy: experience in 8743 cases. HSR Proc Intensive Care Cardiovasc Anesth. 2009;1(3):33-45. (License: CC BY-NC 3.0)
- Ricotta JJ, Charlton MH, De Weese JA. Determining criteria for shunt for shunt placement during carotid endarterectomy: EEG vs back pressur. Ann Surg. 1993;198:642–645.
- Mulaudzi TV, Biccard BM, Robbs JV, Paruk N, Pillay B, Rajaruthnam P. Carotid artery stump pressure and associated neurological changes in predominantly symptomatic carotid artery disease patients undergoing awake carotid endarterectomy. Cardiovasc J Afr. 2009 Mar-Apr;20(2):116-8.
- Chongruksut W, Vaniyapong T, Rerkasem K. Routine or selective carotid artery shunting for carotid endarterectomy (and different methods of monitoring in selective shunting). Cochrane Database Syst Rev. 2014 Jun 23;2014(6):CD000190.
- Squizzato F, Siracuse JJ, Shuja F, Colglazier J, Balachandran Wilkins P, Goodney PP, Sands Brooke B, DeMartino RR. Impact of Shunting Practice Patterns During Carotid Endarterectomy for Symptomatic Carotid Stenosis. Stroke. 2022 Jul;53(7):2230-2240.
- Aburahma AF, Stone PA, Hass SM, Dean LS, Habib J, Keiffer T, Emmett M. Prospective randomized trial of routine versus selective shunting in carotid endarterectomy based on stump pressure. J Vasc Surg. 2010 May;51(5):1133-8.
- Reddy RP, Karnati T, Massa RE, Thirumala PD. Association between perioperative stroke and 30-day mortality in carotid endarterectomy: A meta-analysis. Clin Neurol Neurosurg. 2019 Jun;181:44-51.
- Khattar NK, Friedlander RM, Chaer RA, Avgerinos ED, Kretz ES, Balzer JR, Crammond DJ, Habeych MH, Thirumala PD. Perioperative stroke after carotid endarterectomy: etiology and implications. Acta Neurochir (Wien). 2016 Dec;158(12):2377-2383.
- Riles TS, Imparato AM, Jacobowitz GR, Lamparello PJ, Giangola G, Adelman MA, Landis R. The cause of perioperative stroke after carotid endarterectomy. J Vasc Surg. 1994 Feb;19(2):206-14; discussion 215-6.
- Anzuini A, Briguori C, Roubin GS, Pagnotta P, Rosanio S, Airoldi F, Carlino M, Pagnotta P, Di Mario C, Sheiban I, Magnani G, Jannello A, Melissano G, Chiesa R, Colombo A. Emergency stenting to treat neurological complications occurring after carotid endarterectomy. J Am Coll Cardiol. 2001 Jun 15;37(8):2074-9.
- Léonore FT, Elsa F, David PC, Ludovic C, Pascal B, Charles Henri MA, Pierre A, Eric P. Short- and Long-Term Outcomes Following Biological Pericardium Patches Versus Prosthetic Patches for Carotid Endarterectomy: A Retrospective Bicentric Study. Ann Vasc Surg. 2021 Apr;72:66-71.
- Elsayed N, Ramakrishnan G, Naazie I, Sheth S, Malas MB. Outcomes of Carotid Revascularization in the Treatment of Restenosis After Prior Carotid Endarterectomy. Stroke. 2021 Oct;52(10):3199-3208.
- Goodney PP, Nolan BW, Eldrup-Jorgensen J, Likosky DS, Cronenwett JL; Vascular Study Group of Northern New England. Restenosis after carotid endarterectomy in a multicenter regional registry. J Vasc Surg. 2010 Oct;52(4):897-904, 905.e1-2; discussion 904-5.
- Lal BK, Beach KW, Roubin GS, Lutsep HL, Moore WS, Malas MB, Chiu D, Gonzales NR, Burke JL, Rinaldi M, Elmore JR, Weaver FA, Narins CR, Foster M, Hodgson KJ, Shepard AD, Meschia JF, Bergelin RO, Voeks JH, Howard G, Brott TG; CREST Investigators. Restenosis after carotid artery stenting and endarterectomy: a secondary analysis of CREST, a randomised controlled trial. Lancet Neurol. 2012 Sep;11(9):755-63.
- Zierler RE, Bandyk DF, Thiele BL, Strandness DE Jr. Carotid artery stenosis following endarterectomy. Arch Surg. 1982 Nov;117(11):1408-15.
- Sadideen H, Taylor PR, Padayachee TS. Restenosis after carotid endarterectomy. Int J Clin Pract. 2006 Dec;60(12):1625-30.
- Paraskevas KI, Dardik A, Gloviczki P. Management of Restenosis after Carotid Endarterectomy or Stenting. Angiology. 2023 Apr;74(4):305-307.
- Boulanger M, Camelière L, Felgueiras R, Berger L, Rerkasem K, Rothwell PM, Touzé E. Periprocedural Myocardial Infarction After Carotid Endarterectomy and Stenting: Systematic Review and Meta-Analysis. Stroke. 2015 Oct;46(10):2843-8.
- Kakisis JD, Antonopoulos CN, Mantas G, Moulakakis KG, Sfyroeras G, Geroulakos G. Cranial Nerve Injury After Carotid Endarterectomy: Incidence, Risk Factors, and Time Trends. Eur J Vasc Endovasc Surg. 2017 Mar;53(3):320-335.
- Fokkema M, de Borst GJ, Nolan BW, Indes J, Buck DB, Lo RC, Moll FL, Schermerhorn ML; Vascular Study Group of New England. Clinical relevance of cranial nerve injury following carotid endarterectomy. Eur J Vasc Endovasc Surg. 2014 Jan;47(1):2-7.
- Adhiyaman V, Alexander S. Cerebral hyperperfusion syndrome following carotid endarterectomy. QJM. 2007 Apr;100(4):239-44.
- Lin YH, Liu HM. Update on cerebral hyperperfusion syndrome. J Neurointerv Surg. 2020 Aug;12(8):788-793.
- Kim KH, Lee CH, Son YJ, Yang HJ, Chung YS, Lee SH. Post-carotid endarterectomy cerebral hyperperfusion syndrome : is it preventable by strict blood pressure control? J Korean Neurosurg Soc. 2013 Sep;54(3):159-63.
- Shakespeare WA, Lanier WL, Perkins WJ, Pasternak JJ. Airway management in patients who develop neck hematomas after carotid endarterectomy. Anesth Analg. 2010;110:588-593.
- Stone PA, Srivastava M, Campbell JE, Mousa AY, Hass SH, Kazmi H, Dearing DD, AbuRahma AF. A 10-year experience of infection following carotid endarterectomy with patch angioplasty. J Vasc Surg. 2011 Jun;53(6):1473-7.
- Wikkeling TM, van Gijssel SA, van der Laan MJ, Zeebregts CJ, Saleem BR. Treatment of patch infection after carotid endarterectomy: a systematic review. Ann Transl Med. 2021 Jul;9(14):1213.
- Fatima J, Federico VP, Scali ST, Feezor RJ, Berceli SA, Giles KA, Arnaoutakis DJ, Back MR, Upchurch GR, Huber TS. Management of patch infections after carotid endarterectomy and utility of femoral vein interposition bypass graft. J Vasc Surg. 2019 Jun;69(6):1815-1823.e1.
- Abdelhamid MF, Wall ML, Vohra RK. Carotid artery pseudoaneurysm after carotid endarterectomy: case series and a review of the literature. Vasc Endovascular Surg. 2009 Dec;43(6):571-7.
- Lopes A, Gomes ML, Sobrinho G, Pedro LM. Surgical Treatment of Post-Carotid Endarterectomy Carotid Pseudoaneurysm. EJVES Short Rep. 2019 Jul 5;46:12-13.
- Heskett C, Brake A, Fry L, De Stefano FA, Lei C, Chatley K, Peterson J, Ebersole K. Treatment Options for Pseudoaneurysm After Carotid Endarterectomy: A Systematic Review and Illustrative Case. World Neurosurg. 2022 Nov;167:131-146.