Cholecystectomy
David Ray Velez, MD
The Operative Review of Surgery. 2023; 1:63-76.
Table of Contents
Minimally Invasive Cholecystectomy (Laparoscopic or Robotic)
Basics
- Removal of the Gallbladder by Minimally Invasive Means
- Can be Done by Traditional Laparoscopy or Robotically
Initial Positioning
- Patient Positioned Supine
- Arms Extended
- Prep Nipples-to-Groin
- Monitors are Placed with One at Each Shoulder
Abdominal Access
- Gain Pneumoperitoneum (Veress or Hasson Technique)
- At Umbilicus or Palmer’s Point
- Traditionally Done Using 4 Trocars
- 3-Port, 2-Port, and Single-Port Techniques are Evolving 2-4
- Initial 5-mm Port Generally Placed at Umbilicus
- Position Table in Reverse Trendelenburg (Head Up) with Right-Side Up
- Allows Bowel to Fall Dependently Out of the Field of View
- Position Prior to Placing Additional Ports – Liver May Fall Dependently and Necessitate Lower Port Placement than if Placed Prior to Positioning
- Place Additional Ports
- 12-mm Port at the Subxiphoid Site
- Placed Immediately to the Right of the Falciform Ligament
- Will Cause Difficulty Exchanging Instruments if Placed to the Left Due to Falciform Ligament Being in the Way
- Two Additional 5-mm Ports Along the Right Subcostal Margin
- Placed Below the Edge of the Liver
- 12-mm Port at the Subxiphoid Site
Procedure
- Expose the Gallbladder
- Retract the Fundus Cephalad
- Retract the Body Laterally
- *If Difficult to Grab – Consider Decompressing the Gallbladder by Needle-Aspiration
- Expose the Critical View of Safety
- *See Below
- Divide the Cystic Duct & Cystic Artery
- Two Clips Away from the Gallbladder & One Clip Near the Gallbladder
- *Terms Proximal & Distal are Generally Discouraged Due to Variability in Meaning (Proximal to the Gallbladder vs Proximal from the Origin) 5,6
- Dissect the Gallbladder Off the Liver Bed and Remove
- Consider Using an Endoscopic Retrieval Bag
- Ensure Hemostasis
- Close Incision Sites
Endoscopic Retrieval Bag
- Minimize Risk of Tumor Dissemination in Gallbladder Cancer 7
- Minimize Risk of Spilling Infected Bile, Stones, or Purulence in Acute Cholecystitis 8-10
- No Proven Benefit in Reducing Infection Rate After Elective Surgery 11
- May Consider Avoiding in Absence of Acute Cholecystitis, Accidental Intraoperative Perforation, or Suspected Carcinoma 11
Critical View of Safety 14
- Hepatocytic Triangle (Triangle of Calot) Cleared of All Fat & Fibrous Tissue
- Lower Third of the Gallbladder Separated from Liver to Expose the Cystic Plate
- Only Two Structures Are Seen Entering Gallbladder (Cystic Artery and Cystic Duct)
- “Doublet View” – Seen from Both the Anterior and Posterior Views to Confirm the Critical View
- *See the SAGES Safe Cholecystectomy Program
Intraoperative Cholangiogram (IOC) & Common Bile Duct Exploration (CBDE)
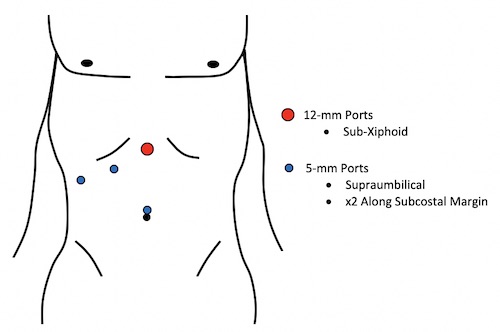
Trocar Placement 1

Critical View of Safety 12
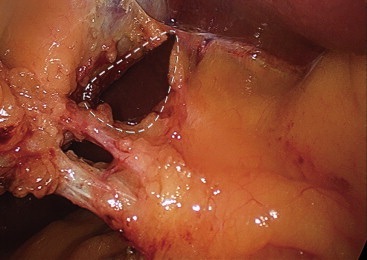
Critical View of Safety 13
Open Cholecystectomy
Indications 15
- Indications:
- Patient’s Informed Request for an Open Procedure
- Known Dense Adhesions in the Upper Abdomen
- Known Gallbladder Cancer
- Surgeon Preference
- Relative Contraindications for Laparoscopic Cholecystectomy:
- Generalized Peritonitis
- Septic Shock from Cholangitis
- Severe Acute Pancreatitis
- Untreated Coagulopathy
- Lack of Equipment
- Lack of Surgeon Expertise
- Prior Abdominal Operations Which Prevent Safe Abdominal Access or Progression of the Procedure
- Advanced Cirrhosis with Hepatic Failure
- Suspected Gallbladder Cancer
Procedure
- Right Subcostal Incision (Kocher Incision)
- 15-cm Incision 2-cm Below the Costal Margin
- Can Connect Laparoscopic Incisions if Converted
- Can Also Perform by an Upper Midline Incision
- Dissect and Remove the Gallbladder
- Retrograde/Anterograde Approaches – See Below
- Ensure Hemostasis
- Venous Bleeding Can Generally Be Controlled by Holding Constant Pressure for 5-10 Minutes
- Other Options: Hemostatic Agents, Hemostatic Sutures
- Close Fascia in Two-Layers
- Use Running Slowly Absorbable Suture (PDS)
- Posterior Layer: Transversalis Fascia and Peritoneum
- Anterior Layer: Anterior Fascia
- Do Not Include the Muscle – Increases Risk for Muscle Necrosis with No Increased Strength to Closure
- Close Skin
Retrograde (“Bottom-Up”) Approach
- *Similar Approach as a Laparoscopic Cholecystectomy
- Start Dissection at the Infundibulum
- Identify the Critical View of Safety
- Divide the Cystic Duct and Cystic Artery
- Ligate with Clips or Sutures
- Dissect the Gallbladder Off the Liver Bed and Remove
Antegrade (“Top-Down”) Approach
- Also Known as “Fundus-Down” or “Dome-Down” Approach
- *Most Commonly Preferred Approach
- Start Dissection at the Fundus
- Place a Clamp on the Gallbladder Fundus to Provide Traction
- Free the Gallbladder Posteriorly and Laterally from the Cystic Plate
- Expose the Cystic Duct and Cystic Artery
- Divide the Cystic Duct and Cystic Artery
- Ligate with Clips or Sutures
Management of the Difficult Gallbladder
Grading Systems
- Nassar Grading 17
- Parkland Grading Scale for Cholecystitis 18
- The Tokyo Guidelines 2018 for Acute Cholecystitis 19
- American Association for the Surgery of Trauma (AAST) Emergency General Surgery (EGS) Score 20
- *No Single Scoring System Universally Adopted – AAST EGS Score is Commonly Accepted
Intraoperative Cholangiogram (IOC)
- Should Be Used Liberally, Especially in Difficult Cases with Unclear Anatomy
- Routine Use is Controversial – Evidence is Insufficient 21,22
- Currently Considered Not Mandatory, Although Practice May Improve Outcomes in More Challenging Cases
- *See Intraoperative Cholangiogram (IOC)
Options if Approaching a Zone of Significant Risk 14
- Conversion to an Open Procedure
- Subtotal Cholecystectomy After Removal of All Stones
- *See Below
- Cholecystostomy Tube
- Low Threshold for Calling in Help of Other Experienced Surgeons
Conversion to Open Procedure
- Conversion to an Open Procedure Should Not Be Considered a “Complication”
- Rate of Conversion: Generally Reported as 1-15% 23,24
- Modern Rates Lower and Decreasing
- Conversion Increases Operative Time, Complication Rates, and Length of Stay 25,26
- Risk Factors for Conversion: 27,28
- Older Age (≥ 50-65 Years)
- American Society of Anesthesiologists (ASA) Classification
- Male Gender
- Emergency Admission
- Acute Cholecystitis
- Gallbladder Wall Thickness
- CBD Stones/Jaundice
- Dilated CBD
- Low Albumin
- Cirrhosis
- Previous Abdominal Surgery
- Modern Surgeons are Generally More Comfortable with Laparoscopic Approaches with Conversion Often Providing Less Benefit
- All Surgeons, However, Should Be Comfortable Opening if Necessary
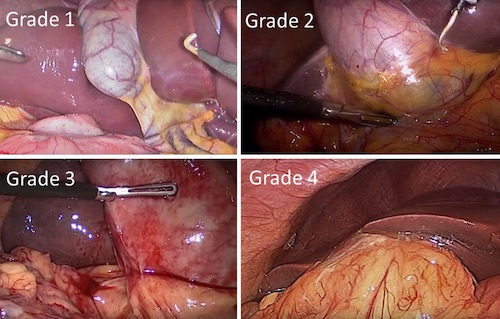
Nasser Grading 16
Subtotal Cholecystectomy
Definitions
- Definitions: 29
- Subtotal Cholecystectomy: Removal of Almost All of the Gallbladder
- Partial Cholecystectomy: Removal of Only Part of the Gallbladder
- Quantitively Less Than a Subtotal Cholecystectomy Although Often Used Interchangeably
- Fundectomy: Removal of Only the Top-Half or Less of the Gallbladder
- Types of Subtotal Cholecystectomy: 29
- Subtotal Fenestrating Cholecystectomy: Does Not Produce a Remnant Gallbladder
- Generally the Preferred Technique in These Situations
- Higher Risk of Bile Leak and Bile Fistula – Most Resolve Spontaneously
- Subtotal Reconstituting Cholecystectomy: Produces a Remnant Gallbladder
- Higher Risk for Recurrent Stones or Cholecystitis from the Remnant
- Subtotal Fenestrating Cholecystectomy: Does Not Produce a Remnant Gallbladder
Fenestrating Technique
- Gallbladder is Opened and Drained at the Fundus
- Bile, Stones, and Debris are Suctioned or Removed
- The Gallbladder Incision is Extended Posteriorly Around the Gallbladder Neck
- Cystic Duct/Artery are Not Dissected
- All Dissection Should Remain Superior to the “Line of Safety” Extending from Rouviere’s Sulcus
- “Shield” of McElmoyle: The Bottom Lip of the Free Peritonealized Gallbladder is Left Behind to Protect from Entering the Hepatocytic Triangle
- The Anterior Wall of The Gallbladder is Completely Removed
- The Posterior Wall is Generally Left on the Cystic Plate Although the Superior-Most Portion May Be Excised
- Remnant Mucosa is Ablated by Cautery or Argon Beam
- May Consider Purse-String Closure of the Cystic Duct from the Inside if Feasible – Often Foregone Due to Safety Concerns
- Leave a Drain Near the Stump to Drain the Presumed Bile Leak (3x Risk)
Reconstituting Technique
- Similar to a Fenestrating Technique
- Instead of Leaving Open, The Lumen is Closed with Sutures or Staplers
- Produces a Small Remnant Gallbladder
Complications
Postcholecystectomy Diarrhea
- Definition: ≥ 3 Loose Stools Per Day After Cholecystectomy
- Risk: 2.1-57.2% 30
- Most Often Stops After Days-Weeks but Can Last for Years
- Causes:
- Increased Enterohepatic Circulation 31
- Increased Bile Salts in the Colon – From Interruption of a Negative Feedback Loop in Bile Acid Synthesis 32
- Altered Gut Microbiome 33
- Patients with Prior Gastrointestinal Symptoms are at Higher Risk 30
- Treatment Options:
- Dietary Modifications
- Cholestyramine (Bile Acid Sequestrant)
- Loperamide
Postcholecystectomy Syndrome
- Definition: Complex of Heterogenous Symptoms That Persist/Recur Colic After Cholecystectomy 34
- Risk: 5-30% 35
- Symptoms: 34
- Abdominal Pain
- Dyspepsia
- Nausea and Vomiting
- Jaundice
- Fever
- Risk Factors: 36,37
- Urgent Surgery
- Lack of Gallstones
- Increased Duration of Preoperative Symptoms
- Female Sex
- Younger Age (20-29 Years)
- Biliary Causes: 34
- Retained Stones
- Biliary Injury
- Bile Leak
- Bile Duct Stricture
- Remnant Gallbladder with Stones/Inflammation
- Remnant Cystic Duct with Stones/Inflammation
- Biliary Dyskinesia
- Non-Biliary Causes: 34
- Pancreatitis
- Pancreatic Tumor
- Pancreatic Divisum
- Hepatitis
- Peptic Ulcer Disease
- Mesenteric Ischemia
- Diverticulitis
- Esophageal Disorders
- Intestinal Motility Disorders
- Coronary Artery Disease
- Intercostal Neuritis
- Wound Neuroma
- Psychiatric Disorders
- Diagnosis Can Be Difficult
- Options: US, CT, or MRCP
- May Require Sphincter of Oddi Manometry
- Treatment: Based on Specific Cause
Biliary Injury
- Risk for Major Bile Duct Injuries: 38
- Elective Surgery: 0.1%
- Emergent Surgery: 0.3%
- 30-Day Mortality: 2% 39
- Effort to Avoid:
- Use of the Critical View of Safety Prior to Transection
- Liberal Use of Intraoperative Cholangiogram – Studies Show Higher Incidence When IOC is Performed but Confounded by the Fact that IOC is More Frequently Used in Difficult Cases 40,41
- *See Management of the Difficult Gallbladder Above
- One of the Most Feared and Morbid Complication of Cholecystectomy
- *See Biliary Injury
Intraoperative Gallbladder Perforation
- Incidence: 10-33% 42
- Possibly Under-Reported in Literature Due to Poor Documentation in Operative Reports with Retrospective Analysis 42
- Risk Factors: 42-44
- Acute Cholecystitis
- Dense Adhesions
- Tense Distended Gallbladder Not Decompressed
- Difficult Operation
- Learning Surgeons/Residents
- Steps When Gallbladder is A Risk for Perforation: 42,45
- During Dissection Off the Liver Bed – Most Common
- Manipulation by Laparoscopic Instruments
- Slippage of Cystic Duct Clips
- Gallbladder Tearing During Retrieval from a Port Site
- Generally Harmless with No Adverse Consequences in Most Cases 42
- Perforation is a Risk for Spilled Stones and Postoperative Abscess 45
- Bile Can Cause a Chemical Peritonitis 42
Retained Stone
- Definitions Vary:
- Retrained Stone: Refers to Any Stone Left Behind and Not Removed During Cholecystectomy
- Can be in the Peritoneal Cavity or in the Common Bile Duct
- Spilled/Dropped Stone: Specifically Refers to a Stone Left in the Peritoneal Cavity After Gallbladder Perforation
- Retrained Stone: Refers to Any Stone Left Behind and Not Removed During Cholecystectomy
- Retained Common Bile Duct Stone
- Mechanisms: 46
- Spontaneous Migration from the Gallbladder Between Preoperative Imaging and Surgery
- Migration During Gallbladder Manipulation
- Asymptomatic Radiolucent Stones Already Present in the CBD but Not Detected by Preoperative Imaging
- Preoperative Imaging Missed a CBD Stone Already Present
- Primary CBD Stone Developed After Surgery
- Can Present Days-Years After Surgery
- Risk for a Clinically Significant Retained CBD Stone: 1-3% 46,47
- No Proven Benefit to Routine Use of IOC in Reducing Rates of Retained Stones
- Treatment: ERCP
- Mechanisms: 46
- Spilled/Dropped Stone (Gallstone Expectoration)
- Stones Serve as a Nidus for Infection and Can Cause Abscess 42
- Risk Factors for Complications After Spilled Stones: 48
- Infected Bile
- Spillage of Pigmented Gallstones – High Likelihood of Harboring Bacteria
- Multiple Stones (> 15)
- Large Stones (> 1.5 cm)
- Old Age
- Surgeon Should Attempt to Retrieve All Spilled Stones at the Index Operation
- Treatment of Abscess: Laparoscopic Drainage and Stone Removal
- If Abscess is Drained Percutaneously, the Stone Should Be Eventually Retrieved Laparoscopically – High Risk of Recurrence if Left
Remnant Gallbladder
- Risk: 0.18% 49
- Present with Symptoms of Postcholecystectomy Syndrome
- *See Above
- May Arise Days-Years After Surgery
- Diagnosis is Often Difficult to Make Due to Rarity
- Options: US, CT, MRCP, or ERCP
- Treatment: Completion Cholecystectomy
- Can Be Performed Open or Laparoscopic 50
- Surgery is Often Challenging Due to Complexity of the Reoperative Field – May Require a Subtotal Fenestrating Cholecystectomy if Unable to Safely Identify the Critical View to prevent Another Remnant Gallbladder 50
Non-Biliary Complications
- Bleeding
- Risk for Clinically Significant Bleeding: 0.1-1.9% 51
- Sources of Bleeding: 52
- Vessel Injury
- Slippage of Clips/Ligatures Off the Cystic Artery
- Liver Bed
- Port Sites
- Treatment Depends on Source
- Bowel Injury
- Risk: 0.07-0.7% 53
- Burn/Thermal Injuries May Present in a Delayed Fashion
- Pneumothorax
- Surgical Site Infection/Abscess
- Mortality
- 30-Day Risk: 0.1-0.7% 54
- Risk Factors: 54
- Elderly
- Underlying Comorbidity
- Acute Surgery
- Perioperative Complications
References
- Velez DR. Cholecystectomy Port Positioning. The Operative Review of Surgery. 2023.
- Kumar M, Agrawal CS, Gupta RK. Three-port versus standard four-port laparoscopic cholecystectomy: a randomized controlled clinical trial in a community-based teaching hospital in eastern Nepal. JSLS. 2007 Jul-Sep;11(3):358-62.
- Lee SC, Choi BJ, Kim SJ. Two-port cholecystectomy maintains safety and feasibility in benign gallbladder diseases: a comparative study. Int J Surg. 2014;12(9):1014-9.
- Casaccia M, Ponzano M, Testa T, Martigli SP, Contratto C, De Cian F. Single-Port Cholecystectomy for Cholecystitis Versus Non-Cholecystitis. JSLS. 2022 Jul-Sep;26(3):e2022.00020.
- Skillicorn CJ. Do the terms “proximal” and “distal” cause confusion amongst radiologists and other clinicians? Clin Radiol. 2009 Apr;64(4):397-402.
- Khara HS, Kothari TH, Johal AS, Kothari ST, Ahuja N, Bhanushali A, Kotru A, Berger A, Kaul V, Gross SA, DiMaio CJ, Hale WB, Abbass R, Ryou M, Sethi A, Turner BG, Fockens P, Diehl DL. Heads or tails: confusion about “proximal” and “distal” terminology for pancreaticobiliary anatomy. Endosc Int Open. 2018 Jul;6(7):E801-E805.
- Goetze TO, Paolucci V. Use of retrieval bags in incidental gallbladder Cancer cases. World J Surg. 2009;33:2161–5.
- Bonjer J. Surgical principles of minimally invasive procedures. Springer. 2017.
- Soper NJ, Scott-Conner C. The SAGES Manual .Volume 1: basic laparoscopy and endoscopy. Springer. 2012;1:265.
- Navez B, Mutter D, Russier Y, Vix M, Jamali F, Lipski D, et al. Safety of laparoscopic approach for acute cholecystitis: retrospective study of 609 cases. World J Surg. 2001;25(10):1352–6.
- La Regina D, Mongelli F, Cafarotti S, Saporito A, Ceppi M, Di Giuseppe M, Ferrario di Tor Vajana A. Use of retrieval bag in the prevention of wound infection in elective laparoscopic cholecystectomy: is it evidence-based? A meta-analysis. BMC Surg. 2018 Nov 19;18(1):102.
- Velez DR. Critical View of Safety. The Operative Review of Surgery. 2023.
- Dziodzio T, Weiss S, Sucher R, Pratschke J, Biebl M. A ‘critical view’ on a classical pitfall in laparoscopic cholecystectomy! Int J Surg Case Rep. 2014;5(12):1218-21. (License: CC BY-NC-ND 3.0)
- The Sages Safe Cholecystectomy Program. Strategies for Minimizing Bile Duct Injuries: Adopting a Universal Culture of Safety in Cholecystectomy. https://www.sages.org/safe-cholecystectomy-program/
- Guidelines for the Clinical Application of Laparoscopic Biliary Tract Surgery. SAGES. 2010
- Doherty G, Manktelow M, Skelly B, Gillespie P, Bjourson AJ, Watterson S. The Need for Standardizing Diagnosis, Treatment and Clinical Care of Cholecystitis and Biliary Colic in Gallbladder Disease. Medicina (Kaunas). 2022 Mar 5;58(3):388. (License: CC BY 4.0)
- Nassar AHM, Ashkar KA, Mohamed AY, Hafiz AA. Is laparoscopic cholecystectomy possible without video technology? Minim Invasive Ther Allied Technol. 1995;4:63-65.
- Madni TD, Leshikar DE, Minshall CT, Nakonezny PA, Cornelius CC, Imran JB, Clark AT, Williams BH, Eastman AL, Minei JP, Phelan HA, Cripps MW. The Parkland grading scale for cholecystitis. Am J Surg. 2018 Apr;215(4):625-630.
- Yokoe M, Hata J, Takada T, Strasberg SM, Asbun HJ, Wakabayashi G, Kozaka K, Endo I, Deziel DJ, Miura F, Okamoto K, Hwang TL, Huang WS, Ker CG, Chen MF, Han HS, Yoon YS, Choi IS, Yoon DS, Noguchi Y, Shikata S, Ukai T, Higuchi R, Gabata T, Mori Y, Iwashita Y, Hibi T, Jagannath P, Jonas E, Liau KH, Dervenis C, Gouma DJ, Cherqui D, Belli G, Garden OJ, Giménez ME, de Santibañes E, Suzuki K, Umezawa A, Supe AN, Pitt HA, Singh H, Chan ACW, Lau WY, Teoh AYB, Honda G, Sugioka A, Asai K, Gomi H, Itoi T, Kiriyama S, Yoshida M, Mayumi T, Matsumura N, Tokumura H, Kitano S, Hirata K, Inui K, Sumiyama Y, Yamamoto M. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018 Jan;25(1):41-54.
- Schuster KM, O’Connor R, Cripps M, Kuhlenschmidt K, Taveras L, Kaafarani HM, El Hechi M, Puri R, Schroeppel TJ, Enniss TM, Cullinane DC, Cullinane LM, Agarwal S Jr, Kaups K, Crandall M, Tominaga G. Revision of the AAST grading scale for acute cholecystitis with comparison to physiologic measures of severity. J Trauma Acute Care Surg. 2022 Apr 1;92(4):664-674.
- Brunt LM. Should We Utilize Routine Cholangiography? Adv Surg. 2022 Sep;56(1):37-48.
- Temperley HC, O’Sullivan NJ, Grainger R, Bolger JC. Is the use of a routine intraoperative cholangiogram necessary in laparoscopic cholecystectomy? Surgeon. 2023 Jan 27:S1479-666X(23)00003-3.
- Kaafarani HM, Smith TS, Neumayer L, Berger DH, Depalma RG, Itani KM (2010) Trends, outcomes, and predictors of open and conversion to open cholecystectomy in Veterans Health Administration hospitals. Am J Surg 200(1):32–40.
- Gholipour C, Fakhree MBA, Shalchi RA, Abbasi M (2009) Prediction of conversion of laparoscopic cholecystectomy to open surgery with artificial neural networks. BMC Surg 9(1):13.
- Tang B, Cuschieri A (2006) Conversions during laparoscopic cholecystectomy: risk factors and effects on patient outcome. J Gastrointest Surg 10(7):1081–1091
- Peters JH, Krailadsiri W, Incarbone R et al (1994) Reasons for conversion from laparoscopic to open cholecystectomy in an urban teaching hospital. Am J Surg 168(6):555–559
- Sutcliffe RP, Hollyman M, Hodson J et al (2016) Preoperative risk factors for conversion from laparoscopic to open cholecystectomy: a validated risk score derived from a prospective U.K. database of 8820 patients. HPB (Oxford) 18(11):922–928.
- Nassar AHM, Zanati HE, Ng HJ, Khan KS, Wood C. Open conversion in laparoscopic cholecystectomy and bile duct exploration: subspecialisation safely reduces the conversion rates. Surg Endosc. 2022 Jan;36(1):550-558.
- Strasberg SM, Pucci MJ, Brunt LM, Deziel DJ. Subtotal Cholecystectomy-“Fenestrating” vs “Reconstituting” Subtypes and the Prevention of Bile Duct Injury: Definition of the Optimal Procedure in Difficult Operative Conditions. J Am Coll Surg. 2016 Jan;222(1):89-96.
- Farrugia A, Attard JA, Khan S, Williams N, Arasaradnam R. Postcholecystectomy diarrhoea rate and predictive factors: a systematic review of the literature. BMJ Open. 2022 Feb 17;12(2):e046172.
- Fort JM, Azpiroz F, Casellas F, et al.. Bowel habit after cholecystectomy: physiological changes and clinical implications. Gastroenterology1996;111:617–22.
- Arlow FL, Dekovich AA, Priest RJ, Beher WT: Bile acid-mediated postcholecystectomy diarrhea. Arch Intern Med 1987; 147: pp. 1327-1329.
- Kang Z, Lu M, Jiang M, Zhou D, Huang H: Proteobacteria acts as a pathogenic risk-factor for chronic abdominal pain and diarrhea in post-cholecystectomy syndrome patients: a gut microbiome metabolomics study. Med Sci Monit 2019; 25: pp. 7312-7320.
- Girometti R, Brondani G, Cereser L, Como G, Del Pin M, Bazzocchi M, Zuiani C. Post-cholecystectomy syndrome: spectrum of biliary findings at magnetic resonance cholangiopancreatography. Br J Radiol. 2010 Apr;83(988):351-61.
- Zackria R, Lopez RA. Postcholecystectomy Syndrome. 2022 Aug 29. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–.
- Russello D, Di Stefano A, Scala R, Favetta A, Emmi S, Guastella T, Latteri F. Does cholecystectomy always resolve biliary disease? Minerva Chir. 1997 Dec;52(12):1435-9.
- FREUD M, DJALDETTI M, DE VRIES A, LEFFKOWITZ M. Postcholecystectomy syndrome: a survey of 114 patients after biliary tract surgery. 1960;93:288-93.
- de’Angelis N, Catena F, Memeo R, Coccolini F, Martínez-Pérez A, Romeo OM, De Simone B, Di Saverio S, Brustia R, Rhaiem R, Piardi T, Conticchio M, Marchegiani F, Beghdadi N, Abu-Zidan FM, Alikhanov R, Allard MA, Allievi N, Amaddeo G, Ansaloni L, Andersson R, Andolfi E, Azfar M, Bala M, Benkabbou A, Ben-Ishay O, Bianchi G, Biffl WL, Brunetti F, Carra MC, Casanova D, Celentano V, Ceresoli M, Chiara O, Cimbanassi S, Bini R, Coimbra R, Luigi de’Angelis G, Decembrino F, De Palma A, de Reuver PR, Domingo C, Cotsoglou C, Ferrero A, Fraga GP, Gaiani F, Gheza F, Gurrado A, Harrison E, Henriquez A, Hofmeyr S, Iadarola R, Kashuk JL, Kianmanesh R, Kirkpatrick AW, Kluger Y, Landi F, Langella S, Lapointe R, Le Roy B, Luciani A, Machado F, Maggi U, Maier RV, Mefire AC, Hiramatsu K, Ordoñez C, Patrizi F, Planells M, Peitzman AB, Pekolj J, Perdigao F, Pereira BM, Pessaux P, Pisano M, Puyana JC, Rizoli S, Portigliotti L, Romito R, Sakakushev B, Sanei B, Scatton O, Serradilla-Martin M, Schneck AS, Sissoko ML, Sobhani I, Ten Broek RP, Testini M, Valinas R, Veloudis G, Vitali GC, Weber D, Zorcolo L, Giuliante F, Gavriilidis P, Fuks D, Sommacale D. 2020 WSES guidelines for the detection and management of bile duct injury during cholecystectomy. World J Emerg Surg. 2021 Jun 10;16(1):30.
- Ismael HN, Cox S, Cooper A, Narula N, Aloia T: The morbidity and mortality of hepaticojejunostomies for complex bile duct injuries: a multi-institutional analysis of risk factors and outcomes using NSQIP. HPB 2017; 19: pp. 352-358.
- Flum DR, Dellinger EP, Cheadle A: Intraoperative cholangiography and risk of common bile duct injury during cholecystectomy. JAMA 2003; 289: pp. 1639-1644.
- Altieri MS, Yang J, Obeid N, Zhu C, Talamini M, Pryor A: Increasing bile duct injury and decreasing utilization of intraoperative cholangiogram and common bile duct exploration over 14 years: an analysis of outcomes in New York state. Surg Endosc 2018; 32: pp. 667-674.
- Altuntas YE, Oncel M, Haksal M, Kement M, Gundogdu E, Aksakal N, Gezen FC. Gallbladder perforation during elective laparoscopic cholecystectomy: Incidence, risk factors, and outcomes. North Clin Istanb. 2018 Jan 12;5(1):47-53.
- Bhatti CS, Tamijmarane A, Bramhall SR: A tale of three spilled gallstones: one liver mass and two abscesses. Dig Surg. 2006, 23: 198-200.
- Frola C, Cannici F, Cantoni S: Peritoneal abscess formation as a late complication of gallstones spilled during laparoscopic cholecystectomy. Br J Radiol. 1999, 72: 201-203.
- Helme S, Samdani T, Sinha P. Complications of spilled gallstones following laparoscopic cholecystectomy: a case report and literature overview. J Med Case Rep. 2009 Jul 24;3:8626.
- Lee DH, Ahn YJ, Lee HW, Chung JK, Jung IM. Prevalence and characteristics of clinically significant retained common bile duct stones after laparoscopic cholecystectomy for symptomatic cholelithiasis. Ann Surg Treat Res. 2016 Nov;91(5):239-246.
- Stuart SA, Simpson TI, Alvord LA, Williams MD. Routine intraoperative laparoscopic cholangiography. Am J Surg. 1998;176:632–637.
- Zehetner J, Shamiyeh A, Wayand W: Lost gallstones in laparoscopic cholecystectomy: all possible complications. Am J Surg. 2007, 193: 73-78. 10.1016/j.amjsurg.2006.05.015.
- Chowbey P, Soni V, Sharma A, Khullar R, Baijal M (2010) Residual gallstone disease — Laparoscopic management. Indian J Surg72:220–225.
- Grossman JG, Johnston WR, Fowler KJ, Williams GA, Hammill CW, Hawkins WG. A diagnosis reconsidered: the symptomatic gallbladder remnant. J Hepatobiliary Pancreat Sci. 2019 Apr;26(4):137-143.
- Bonds M, Rocha F. Cholecystectomy Techniques and Postoperative Problems. In: Blumgart’s Surgery of the Liver, Biliary Tract and Pancreas, 7e. Elsevier. 2023.
- Kaushik R. Bleeding complications in laparoscopic cholecystectomy: Incidence, mechanisms, prevention and management. J Minim Access Surg. 2010 Jul;6(3):59-65.
- Browne IL, Dixon E. Delayed jejunal perforation after laparoscopic cholecystectomy. J Surg Case Rep. 2016 Feb 22;2016(2):rjw017.
- Sandblom G, Videhult P, Crona Guterstam Y, Svenner A, Sadr-Azodi O. Mortality after a cholecystectomy: a population-based study. HPB (Oxford). 2015 Mar;17(3):239-43.