Cholecystitis
Cholecystitis
David Ray Velez, MD
Table of Contents
Definitions/Classification
Cholecystitis: Inflammation of the Gallbladder
Timing
- Acute Cholecystitis: Acute Inflammation of the Gallbladder
- Chronic Cholecystitis: Chronic Inflammation of the Gallbladder
Gallstones
- Calculous Cholecystitis: Inflammation of the Gallbladder Due to Gallstone Impaction of the Cystic Duct
- Acalculous Cholecystitis: Inflammation of the Gallbladder without the Presence of Gallstones
The Terms “Acute Cholecystitis” and “Acute Calculous Cholecystitis” are Often Used Interchangeably
Complications
- Emphysematous Cholecystitis: Infection of the Gallbladder by Gas-Forming Organisms
- Gangrenous Cholecystitis: Acute Inflammation of the Gallbladder Complicated by Necrosis
- Can Be Caused by Gallstones, Inflammation, Infection, and Ischemia
Severity Classification (Tokyo Guidelines)
- Grade I (Mild): Limited Disease in the Gallbladder and No Organ Dysfunction
- Low-Risk of Cholecystectomy
- Grade II (Moderate): Extensive Disease in the Gallbladder but No Organ Dysfunction
- Cholecystectomy May Be More Difficult
- Characterized by Leukocytosis, Palpable-Tender Mass, Duration > 72 Hours, and Significant Inflammation on Imaging
- Grade III (Severe): Organ Dysfunction Present
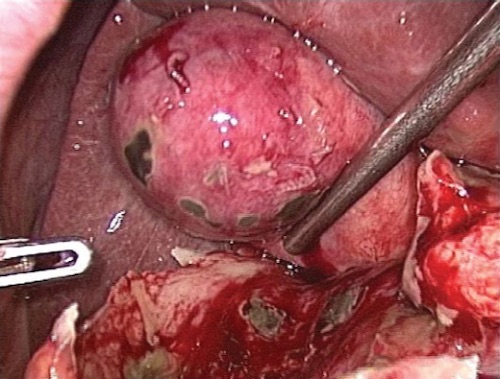
Gangrenous Cholecystitis at Surgery 1
Background
Cholecystitis is Most Often Due to Cystic Duct Obstruction by Gallstones (Calculous Cholecystitis)
Acalculous Cholecystitis Most Often Presents in Otherwise Ill Patients and May Be Caused by Biliary Stasis, Increased Viscosity, and Ischemia
Risk Factors for Acalculous Cholecystitis
- Trauma
- Burns
- Surgery
- AIDS
- Infection or Sepsis
- CPR
- TPN
- Diabetes
- Immunosuppression
- Childbirth
Microbiology
- Inflammation is Initially Sterile Until It Becomes Secondarily Infected
- Most Common Organism: Escherichia coli
- Clostridium perfringens is the Most Common Cause of Emphysematous Cholecystitis (Escherichia coli is Second)
Emphysematous Cholecystitis Frequently Evolves to Gangrenous Cholecystitis (75%) or Perforation (20%) and is Associated with High Mortality (25%)
Presentation and Diagnosis
Symptoms
- Right-Upper Quadrant (RUQ) Abdominal Pain
- Murphy’s Sign – Sudden “Catch” During Inspiration with Gentle RUQ Pressure
- Boas Sign – Hyperesthesia (Increased Sensitivity) Below the Right Scapula on the Back
- Nausea and Vomiting
- Loss of Appetite
- Fever
- Diaphoresis
Labs
- Leukocytosis is the Primary Laboratory Finding
- Liver Function Tests (LFT’s) are Generally Normal or Only Slightly Elevated
- Significant LFT Elevations Raised Increased Concern for Choledocholithiasis
Imaging
- Ultrasound (US) is the Primary Radiographic Test – 95% Sensitive
- May Also Be Seen on CT or MRI
- Radiographic Findings:
- Gallstones and Sludge
- Gallbladder Wall-Thickening (Normally < 4 mm)
- Gallbladder Distention
- Pericholecystic Fluid
- Mucosal Ischemic Changes
- Sonographic Murphy’s Sign
- CCK-Stimulated HIDA Scan is the Most Sensitive Test – Ordered if US Findings are Uncertain
It is Important to Evaluate for Choledocholithiasis During Work-Up – *See Choledocholithiasis

Cholecystitis with Wall-Thickening and Impacted Stone on US 2

CT Showing Emphysematous Cholecystitis 3
Treatment
The Primary Treatment is Early Cholecystectomy
Timing
- Early (< 72 Hours) Cholecystectomy is Preferred Over Late (7-45 Days) Cholecystectomy
- Early Has Shorter Length of Stay, Fewer Workdays Lost, Lower Total Costs, and Less Wound Infection
- Similar Complications, Conversion to Open, CBD Injury Rate, and Mortality
- No Benefit to “Cooling Off Period”
- Emphysematous or Gangrenous Cholecystitis Should Be Done Emergently
If Unstable or Unfit for Surgery: Percutaneous Cholecystostomy Tube
- 90% Effective at Relieving Symptoms
- Repeat Cholecystogram in 3-6 Weeks
- Contrast Injected Through the Catheter
- Can Remove Catheter if the Cystic Duct Patent (Leave if Not Patent)
- Plan for Interval/Delayed Cholecystectomy After Recovery – Not Necessary for Acalculous Cholecystitis
Pregnancy Considerations
- Surgery Has a Lower Risk of Adverse Pregnancy Outcomes in Acute Cholecystitis Across All Trimesters
- Greatest Benefit Seen in the Third Trimester
- *Historically, Nonoperative Management Was Recommended During the First Trimester (Risk of Organogenesis) and Third Trimester (Risk for Preterm Labor) with Percutaneous Cholecystostomy Tube if Fails, However Newer Evidence Recommends Surgery Across All Trimesters
References
- Gomes RM, Mehta NT, Varik V, Doctor NH. No 72-hour pathological boundary for safe early laparoscopic cholecystectomy in acute cholecystitis: a clinicopathological study. Ann Gastroenterol. 2013;26(4):340-345. (License: CC BY-NC-SA-3.0)
- Cwik G, Skoczylas T, Wyroślak-Najs J, Wallner G. The value of percutaneous ultrasound in predicting conversion from laparoscopic to open cholecystectomy due to acute cholecystitis. Surg Endosc. 2013 Jul;27(7):2561-8. (License: CC BY-4.0)
- Sunnapwar A, Raut AA, Nagar AM, Katre R. Emphysematous cholecystitis: Imaging findings in nine patients. Indian J Radiol Imaging. 2011 Apr;21(2):142-6. (License: CC BY-NC-SA-3.0)