Esophagus: Cancer
Esophageal Cancer
Types
- Squamous Cell Carcinoma
- Most Common in the World
- Most Common Site: Upper 2/3
- Mets: Lung
- Associated With: Alcohol, Tobacco & Hot Tea
- Adenocarcinoma
- Most Common in the US
- Most Common Site: Lower 1/3
- Mets: Liver
- Associated With: GERD & Barrett’s Esophagus
- Tobacco & Obesity are Also Smaller Risk Factors
Diagnostic Staging
- Tissue Dx:
- Small < 2 cm & Superficial: Endoscopic Resection
- Large: Endoscopic Bx
- T: EUS
- N: EUS & FNA Suspicious Nodes
- The Best Predictor of Long-Term Survival
- At Resection ≥ 15 Nodes Required for Adequate Staging
- M: CT Chest/Abd/Pelvis & PET CT
- If M1 – Almost 0% 5-Year Survival
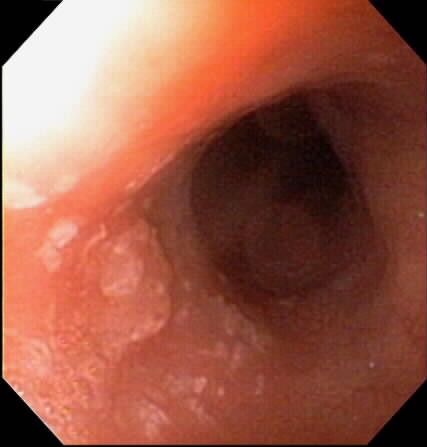
Esophagus SCC 1

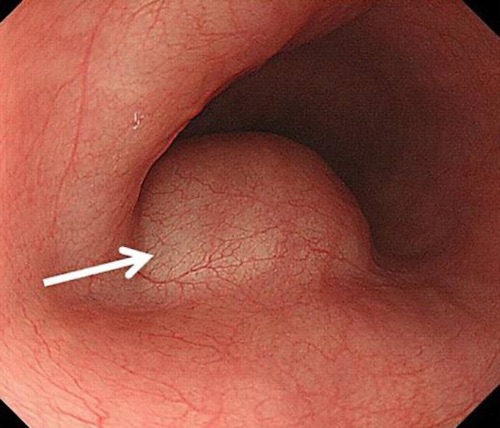
Esophagus Adenocarcinoma 2
Esophageal Cancer – Classification & Staging
TNM Staging – AJCC 8
| T | N | M | |
| 1 | 1a – Lamina Propria/Muscularis Mucosae
1b – Submucosa (Rich Lymphatics) |
1-2 LN | Mets |
| 2 | Muscularis Propria | 3-6 LN | |
| 3 | Invades Adventitia | ≥ 7 LN | |
| 4 | 4a – (Resectable) Pleura, Pericardium, Azygos, Diaphragm or Peritoneum
4b – (Unresectable) Aorta, Trachea or Vertebrae |
- Grade (G):
- G1 – Well Differentiated
- G2 – Moderately Differentiated
- G3 – Poorly Differentiated
- Location (L) – For SCC Only:
- Upper (U) – Above Azygos Vein
- Middle (M) – Between Azygos & Inferior Pulmonary Vein
- Lower (L) – Below Inferior Pulmonary Vein
- Grade (G):
- Staging:
| T | N | M | G | L | ||
| I (SCC) | A | T1a | N0 | M0 | G1 | Any |
| B | T1a | N0 | M0 | G2-3 | Any | |
| T1b | N0 | M0 | G1-3 | Any | ||
| T2 | N0 | M0 | G1 | Any | ||
| II (SCC) | A | T2 | N0 | M0 | G2-3 | Any |
| T3 | N0 | M0 | G1 | Any | ||
| T3 | N0 | M0 | G2-3 | Lower | ||
| B | T3 | N0 | M0 | G2-3 | M or U | |
| T1 | N1 | M0 | Any G | Any | ||
| I (AC) | A | T1a | N0 | M0 | G1 | Any |
| B | T1a | N0 | M0 | G2 | Any | |
| T1b | N0 | M0 | G1-2 | Any | ||
| C | T1a-b | N0 | M0 | G3 | Any | |
| T2 | N0 | M0 | G1-2 | Any | ||
| II (AC) | A | T2 | N0 | M0 | G3 | Any |
| B | T1 | N1 | M0 | Any G | Any | |
| T3 | N0 | M0 | Any G | Any | ||
| III | A | T1 | N2 | M0 | Any G | Any |
| T2 | N1 | M0 | Any G | Any | ||
| B | T2 | N2 | M0 | Any G | Any | |
| T3 | N1-2 | M0 | Any G | Any | ||
| T4a | N0-1 | M0 | Any G | Any | ||
| IV | A | T4a | N2 | M0 | Any G | Any |
| T4b | Any N | M0 | Any G | Any | ||
| Any T | N3 | M0 | Any G | Any | ||
| B | Any T | Any N | M1 | Any G | Any | |
Siewert-Stein Classification of Gastroesophageal Junction Adenocarcinoma
- Type I: Distal Esophagus, Epicenter of Lesion 1-5 cm Above the Anatomic GEJ
- Type II: True GE Junction, Epicenter of Lesion 1 cm Above to 2 cm Below the Anatomic GEJ
- Type III: Stomach, Epicenter of Lesion 2-5 cm Below the Anatomic GEJ
Esophageal Cancer – Treatment
Unresectable Factors
- < 5 cm From Cricopharyngeus
- Nerve Invasion:
- RLN (Hoarseness)
- Brachial Plexus (Horner’s)
- Phrenic
- Malignant Pleural Effusion
- Malignant Fistula
- Die from Aspiration
- Tx: Palliative Stent
- Invasion of Other Structures
- Nodes Outside of Resection Area (Supraclavicular/Celiac)
Primary Treatment
- T1a: Endoscopic Resection/Ablation
- T1b: Esophagectomy
- Superficial T1b Adenocarcinoma – Consider Endoscopic Resection
- T2-T4a or N+: Esophagectomy With Neoadjuvant Chemo-XRT
- May Consider Definitive Chemo-XRT
- T4b or Unresectable: Definitive Chemo-XRT
- M1: Palliative Care
Considerations
- Chemo-XRT (5-FU & Cisplatin)
- Neoadjuvant Indications: ≥ T2
- Adjuvant Indications: N+, SCC (Not R0) & Most Adenocarcinoma
- Can Avoid if:
- SCC: R0 Resection
- Adenocarcinoma: Only Low Grade R0 Resection
- Can Avoid if:
- Malnutrition
- Common Complication
- Tx: Esophageal Stent or Jejunostomy-Tube
- Do Not Place a Gastrostomy-Tube (Compromises Gastric Conduit for Later Reconstruction)
- Palliative Cares
- Consider Chemo-XRT
- May Require Stent for Dysphagia
- Most Common Cause of Recurrent Dysphagia: Tumor Ingrowth
- Median Patency: 219 Days
- Second Most Common Cause of Recurrent Dysphagia: Stent Migration
- Most Likely in Distal Esophagus
- Most Common Cause of Recurrent Dysphagia: Tumor Ingrowth
Post-Intervention Surveillance
- > 90% of Recurrences Occur Within 2 Years
- Endoscopic Resection: Endoscopy Every 3 Months for First Year, Then Every 4-6 Months for Second Year, Then Every Year Forever
- Also Consider CT Every Year for 3 Years if T1bN0
- Definitive Chemo-XRT: Endoscopy Every 3-6 Months for 2 Years, Then Every Year for Three Years
- Also Consider CT Every 6-9 Months for 2 Years, Then Every Year for 5 Years
- Esophagectomy: CT Every 1 Year for 3 Years
Other Esophageal Tumors
Leiomyoma
- Tumor of Muscularis Propria
- Most Common Benign Tumor of Esophagus
- Slow Growing with Low Malignant Potential
- Most Common Site: Lower 2/3 (Smooth Muscle)
- Well Circumscribed Within Wall
- Evaluation:
- Incidental Findings:
- Barium Esophagram: Smooth Crescent-Shaped Defect
- Endoscopy: Freely-Mobile Submucosal Lesion with Normal Overlying Mucosa
- Dx: EUS
- Do Not Bx (Scar Difficult for Resection)
- Incidental Findings:
- Tx:
- ASx & < 1-2 cm: Observation
- Sx or > 1-2 cm: Surgical Enucleation (VATS or Thoracotomy)
- Giant (> 10 cm) or Leiomyosarcoma: Esophagectomy
Esophageal Leiomyoma 3
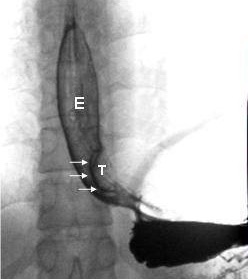
Leiomyoma – Esophagram 4
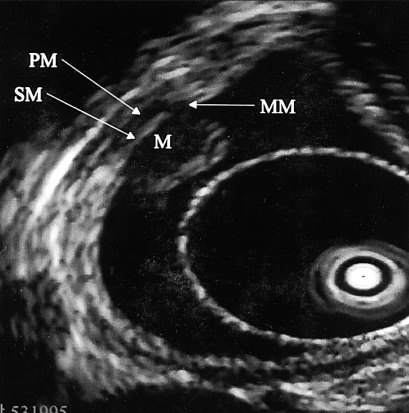
Leiomyoma – EUS 5
Other Malignant Tumors
- Much More Rare
- Types:
- Small Cell Carcinoma
- Melanoma
- Gastrointestinal Stromal Cell Tumor (GIST)
Tylosis
- Rare Autosomal Dominant Disease
- Linked to TEC (Tylosis with Esophageal Cancer) Gene on 17q25
- Presentation:
- Palmoplantar Keratomas – Hyperkeratosis (Skin Thickening) of Hands/Soles
- Esophageal SCC (40-90% Risk)
- Management: Surveillance Endoscopy Every Year After Age 20
References
- Cash BD, Johnston LR, Johnston MH. Cryospray ablation (CSA) in the palliative treatment of squamous cell carcinoma of the esophagus. World J Surg Oncol. 2007 Mar 16;5:34. (License: CC BY-2.0)
- Abe Y, Koike T, Iijima K, Imatani A, Ishida K, Yuki T, Miyata G, Shimosegawa T. Esophageal Adenocarcinoma Developing after Eradication of Helicobacter pylori. Case Rep Gastroenterol. 2011;5(2):355-60.(License: CC BY-NC-ND-3.0)
- Maki K, Takeno S, Nimura S, Yamana I, Shimaoka H, Hashimoto T, Shibata R, Shiwaku H, Yamashita K, Yamashita Y. Prone Position Is Useful in Thoracoscopic Enucleation of Esophageal Leiomyoma. Case Rep Gastroenterol. 2015 May 22;9(2):165-70. (License: CC BY-NC-3.0)
- Luh SP, Hou SM, Fang CC, Chen CY. Video-thoracoscopic enucleation of esophageal leiomyoma. World J Surg Oncol. 2012 Mar 16;10:52. (License: CC BY-2.0)
- Lee SJ, Paik YH, Lee DK, Lee KS, Lee SI. The diagnostic value of endoprobe for small esophageal leiomyomas derived from the muscularis mucosae. Yonsei Med J. 2005 Feb 28;46(1):61-5. (License: CC BY-NC-3.0)