Trauma: Head Trauma
Skull Fracture
General Surgical Repair Indications
- Depressed > 1 cm
- Contaminated/Infected
- Persistent CSF Leak
- Frontal Sinus Involvement
- Open with Dural Penetration/Pneumocephalus
- Significant Hematoma
- Overlap or Violation of Inner & Outer Table
Temporal Bone Fracture
- Most Common After Blunt Trauma
- Occur in 30-70% of Cases Involving Blunt Head Trauma
- Most Fractures are Longitudinal (70-80%), Transverse are Less Common
- Complications:
- Intracranial Hemorrhage
- CSF Leak – Typically Resolves Within 2 Weeks
- Meningitis – Prophylactic ABX Not Indicated
- Hearing Loss (40%) – Higher Risk in Peds
- Sensorineural Loss Has Worse Prognosis than Conductive Loss
- Vertigo
- Facial Nerve Injury & Paralysis (30-70%) – Lower Risk in Peds
- Treatment:
- Emergent Surgery Indications:
- Brain Herniation into the Middle Ear, Mastoid or External Acoustic Meatus
- Massive Bleeding from the Intra-Temporal Carotid Artery
- Elective Surgery Indications:
- Severe Facial Nerve Injury
- Conductive Hearing Loss Due to Ossicular Disruption – Repair After 3 Months
- Conductive Loss Due to Hemotympanum Typically Resolves
- Sensorineural Hearing Loss Deemed to Be Likely to Improve Surgery (Poorer Prognosis)
- CSF Leak > 14 Days
- Emergent Surgery Indications:
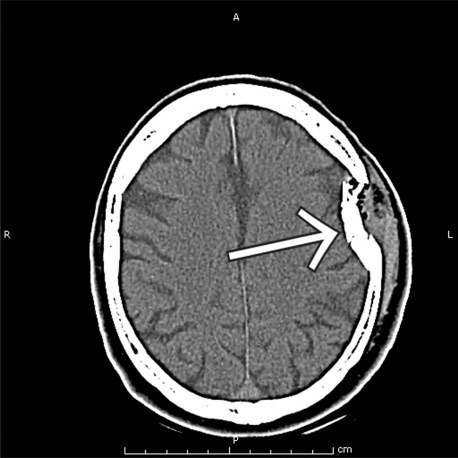
Skull Fracture 1
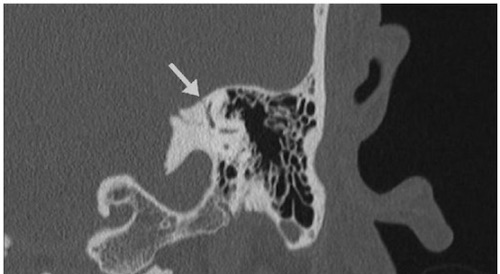
Temporal Bone Fracture 2
Basal Skull Fracture
- Most Common After Blunt Trauma
- Signs:
- “Racoon Eyes”: Periorbital Ecchymosis (Anterior/Middle Fossa Fracture)
- “Battle Signs”: Mastoid Ecchymosis (Middle Fossa Fracture)
- Hemotympanum
- CSF Leakage
- Complications:
- Intracranial Hemorrhage
- Carotid Artery Injury or Carotid-Cavernous Fistula
- CSF Leak – Typically Resolves Within 2 Weeks
- Meningitis – Prophylactic ABX Generally Not Indicated
- Cranial Nerve Injury & Paralysis
- Cavernous Sinus Thrombosis
- Vertigo
- Surgery Indications:
- Intracranial Hemorrhage
- Vascular Injury
- Severe Cranial Nerve Injury
- Persistent CSF Leak > 2 Weeks
Cerebrospinal Fluid (CSF) Leak
- Clear Rhinorrhea or Otorrhea
- From Tear in Dura Creating Communication Between Subarachnoid Space & Sinuses/Middle Ear
- Most Resolve Spontaneously within 7 Days
- Dx: Tau Protein (β2-Transferrin)
- Tx: Observation
- If Persistent: Lumbar Drain or Surgery

Racoon Eyes 3

Battle Signs 4
Facial Fracture
Frontal Sinus Fracture
- Strongest Facial Bone (Thick Cortical Bone)
- Tx Options:
- No Displacement or CSF Leak: Observation
- Anterior Table Displaced with No Communication: ORIF
- Posterior Table Displaced, Communication or CSF Leak: Obliteration of Sinus
Nasal Fracture
- Most Common Facial Fracture Site
- Edema Can Obscure Anatomy
- Repair Timing:
- First 3 Hours (Before Edema Onset)
- After 3-10 Days (After Edema Resolution)
- Septal Hematoma
- Can Cause Pressure Necrosis
- Must Always Preform an Intranasal Examination
- Tx: I&D with Packing

Frontal Sinus Fracture 5

Nasal Fracture 6
Orbital Fracture
- Emergencies:
- Oculocardiac Reflex (Aschner Phenomenon)
- Nausea & Bradycardia/Asystole Due to Extraocular Muscle Entrapment
- Reflex Between Trigeminal Nerve & Vagus
- Roof Fracture
- Oculocardiac Reflex (Aschner Phenomenon)
- Orbital Blowout Fracture: Fracture Involving Orbital Floor/Medial Wall
- “Pure” Orbital Blowout – Orbital Rim Preserved
- “Impure” Orbital Blowout – Orbital Rim Fractured
- Treatment Timing:
- Emergency: Immediate Repair
- Nonemergent: Delayed Repair < 2 Weeks (Allow Edema to Decrease)
- Orbital Compartment Syndrome
- Presentation: Markedly Increased Intraocular Pressure, Impaired Vision & Eye Movement
- Tx: Lateral Canthotomy to Decompress

Orbital Blowout Fracture 7
Zygomaticomaxillary Complex (ZMC) Fracture
- “Tripod” Fracture
- Zygomatic Arch
- Lateral Orbital Wall
- Anterior Maxilla
- “Quadripod” Fracture
- Tripod + Orbital Floor
- Tx: Cosmetic ORIF
Mandible Fracture
- Most Common in Blunt Trauma
- Frequently Multiple
- Most Common Sx: Malocclusion (Imperfect Positioning of Teeth Upon Closure)
- Healing Ability
- “Favorable” – Inferior & Anterior Angled
- “Unfavorable” – Inferior & Posterior Angled
- Tx: ORIF or Intermaxillary Fixation (IMF)
- Most Important Factor: Accurate Alignment of Upper/Lower Teeth
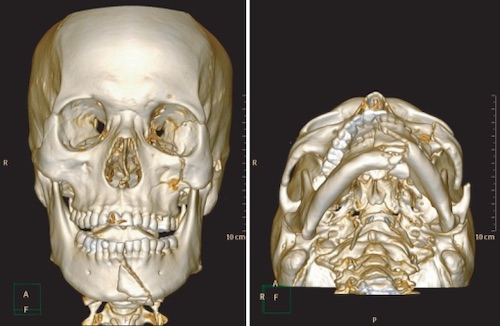
ZMC & Mandible Fracture 8
Le Fort Fractures
- Classification: Mn
- Type I: Transverse Maxillary Fracture
- Type II: Oblique Maxillary/Nasal Fracture
- Most Common (60%)
- Type III: Orbital Walls
- Tx: Early Surgical Repair (Before Bony Resorption and Fibrous Ingrowth)
- Goal: Restore Facial Projection, Height & Proper Occlusion
- Options:
- Ex-Fix
- ORIF
- Intermaxillary Fixation (IMF)
- Suspension Wires
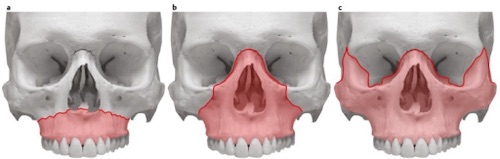
Le Fort Fractures; (a) Type I, (b) Type II, (c) Type III 9
Other Issues
Epistaxis
Laceration
- Scalp
- Copiously Irrigate & Repair
- Do Not Need to Remove Hair
- Ear
- Suture Through Cartilage
- Lip
- Most Important Principle: Align Vermillion Border
- Tongue
- Minor Will Generally Heal Without Intervention
- Repair Lingual Artery if Deep & Transected
Facial Nerve Transection
- Most Common Cause: Temporal Fracture at Geniculate Ganglion
- Tx:
- Medial to Lateral Canthus of Eye: Conservative Management
- Likely to Recover by Arborization
- Lateral to Lateral Canthus of Eye: Surgically Repair
- Medial to Lateral Canthus of Eye: Conservative Management
Auricular Hematoma
- Definition: Hematoma of the Cartilaginous Auricle (Outer Ear)
- Most Common After Blunt Trauma from Sports (Wrestling, Rugby, Boxing)
- Risk for Cauliflower Ear (Calcification/Fibrocartilage Overgrowth)
- Treatment:
- Early Hematoma: Aspiration or I&D
- Aspiration Generally Preferred if Small (< 2 cm) or Early (< 24-48 Hours)
- Goal: Prevent Cauliflower Ear
- Late Cauliflower Ear: Resection or Reconstruction
- Early Hematoma: Aspiration or I&D
Stensen’s Duct Laceration
- Presentation: Painful Parotid Atrophy & Fascial Asymmetry
- Tx: Repair Over Stent

Facial Laceration of the Vermillion Border 10

Auricular Hematoma 11
Mnemonics
LeFort Fracture Classification
- 1-2-3: Speak No Evil, See No Evil, Hear No Evil
- *Not Exact Order of Original 3 Wise Monkeys Maxim
References
- Paulsen J, Testa N. Isolated traumatic expressive aphasia. West J Emerg Med. 2011 Feb;12(1):141. (License: CC BY-NC-4.0)
- Peng KA, Ahmed S, Yang I, Gopen Q. Temporal bone fracture causing superior semicircular canal dehiscence. Case Rep Otolaryngol. 2014;2014:817291. (License: CC BY-3.0)
- McPheeters RA, White S, Winter A. Raccoon eyes. West J Emerg Med. 2010 Feb;11(1):97.(License: CC BY-NC-4.0)
- Mukherjee SK, Hossain M. Traumatic brain injury management can improve in primary care centre in remote area with minimum health assistance by proper training. J Neurosci Rural Pract. 2013 Apr;4(2):242-4.(License: CC BY-NC-SA-3.0)
- Zorn J, Agag RL. Frontal sinus fracture. Eplasty. 2011 Feb 25;11:ic5. (License: CC BY-2.0)
- Kopacheva-Barsova G, Arsova S. The Impact of the Nasal Trauma in Childhood on the Development of the Nose in Future. Open Access Maced J Med Sci. 2016 Sep 15;4(3):413-419. (License: CC BY-2.5)
- Kozakiewicz M, Szymor P. Comparison of pre-bent titanium mesh versus polyethylene implants in patient specific orbital reconstructions. Head Face Med. 2013 Oct 29;9:32. (License: CC BY-2.0)
- Lee SS, Kim SG, Moon SY, Oh JS, You JS. The treatment of malocclusion after open reduction of maxillofacial fracture: a report of three cases. J Korean Assoc Oral Maxillofac Surg. 2014 Apr;40(2):91-5. (License: CC BY-NC-3.0)
- Kühnel TS, Reichert TE. Trauma of the midface. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2015 Dec 22;14:Doc06. (License: CC BY-4.0)
- Chang CS, Wallace CG, Hsiao YC, Chang CJ, Chen PK. Botulinum toxin to improve results in cleft lip repair: a double-blinded, randomized, vehicle-controlled clinical trial. PLoS One. 2014 Dec 26;9(12):e115690. (License: CC BY-4.0)
- Heilman J. Wikimedia Commons. (License: CC BY-SA-4.0)