Cardiothoracic Surgery: Lung Cancer Diagnosis & Staging
Radiographic Diagnosis
General Screening
Imaging
- Primary Modality: Chest CT
- Extended to Include Upper Abdomen, Liver & Adrenal Glands
- Best Test for T/N Status
- Whole-Body PET
- Should be Obtained in All Potentially Operable Candidates – May Decrease the Risk of Futile Surgery if Metastases Found
- Routine Use Controversial – No Evidence of Improved Survival
Solitary Pulmonary Nodule (SPN) Features
- Benign Features:
- Size < 5 mm
- Size Remains Stable
- Fat with a Smooth Border
- Calcification (Popcorn, Central, Diffuse or Lamellated)
- Eccentric or Punctate Calcification are Nonspecific & May Be Malignant
- Low Enhancement < 15 Hounsfield Units
- Malignant Features:
- Size > 20 mm
- Size Doubles in Less Than 1 Year
- Spiculated or Lobular Border
- High Enhancement > 20 Hounsfield Units
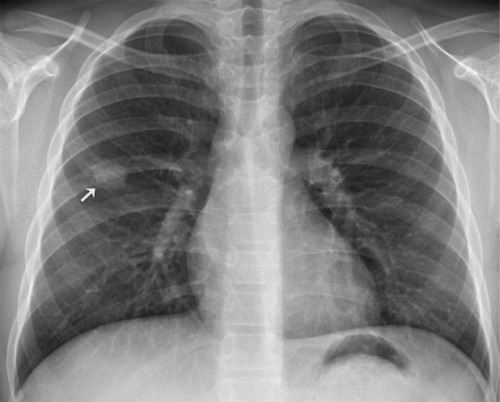
Solitary Pulmonary Nodule CXR 1
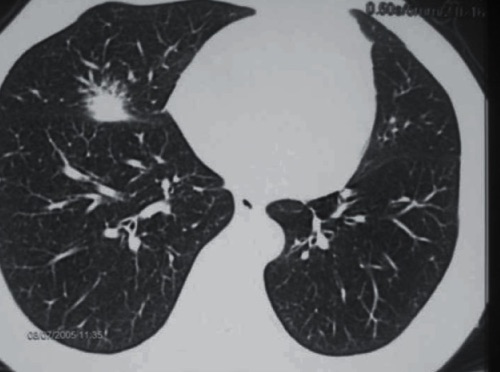
Malignant Solitary Pulmonary Nodule, 2.5 cm with Speculated Borders 2
Lung RADS Assessment
| Score | Category | Findings | Management | Risk of Malignancy |
| 0 | Incomplete | Prior Chest CT Used for Comparison or Part of Lung Cannot Be Visualized | Additional Imaging or Comparison to Prior Imaging | N/A |
| 1 | Negative | No Lung Nodules or Nodules with Specific Benign Calcifications | Continue Annual Screening | < 1% |
| 2 | Benign | Solid: < 6 mm or New < 4 mm
Part-Solid: < 6 mm Non-Solid: < 30 mm or ≥ 30 mm & Unchanged or Slowly Growing Category 3 or 4 Nodules Unchanged for ≥ 3 Months |
Continue Annual Screening | < 1% |
| 3 | Probably Benign | Solid: ≥ 6 mm or New ≥ 4 mm
Part-Solid: ≥ 6 mm or New < 6 mm Non-Solid: ≥ 30 mm |
Repeat CT in 6 Months | 1-2% |
| 4A | Suspicious | Solid: ≥ 8 mm, Growing < 8 mm or New ≥ 6 mm
Part-Solid: Solid Component ≥ 6 mm or New/Growing < 4 mm Solid Component Endobronchial Nodule |
Repeat CT in 3 Months; Add PET/CT if There is a Solid Component ≥ 8 mm | 5-15% |
| 4B | Very Suspicious | Solid: ≥ 15 mm or New/Growing ≥ 8 mm
Part-Solid: Solid Component ≥ 8 mm or New/Growing ≥ 4 mm Solid Component |
CT, PET/CT and/or Biopsy | > 15% |
| 4X | Category 3 or 4 Nodules with Additional Features that Increase the Suspicion of Malignancy | > 15% | ||
| S | Clinically Significant or Potentially Clinically Significant Findings (Non-Lung Cancer) | Modifier – May Add on to Category 0-4 | As Indicated | N/A |
| C | Prior Diagnosis of Lung Cancer | Modifier – May Add on to Category 0-4 | As Indicated | N/A |
Tissue Diagnosis
Biopsy
- Biopsy Required for Diagnosis
- Biopsy Techniques:
- Bronchoscopic Biopsy
- Preferred for Large Central Lesions
- Transthoracic (Percutaneous) Biopsy
- Preferred for Small Peripheral Lesions
- Higher Rate of Indeterminate Diagnoses Due to Smaller Sample Size
- Thoracoscopic (Surgical) Biopsy
- Often Preferred for Early-Stage Peripheral Lesions – Resection May Be Curative
- Bronchoscopic Biopsy
Lymph Node Sampling – Indications
- Size > 1 cm on CT
- “Hot” Nodule (FDG Uptake Greater than Mediastinal Blood Pool) on PET
Lymph Node Sampling – Approaches
- Anterior Mediastinotomy (Chamberlain Procedure)
- Endoscopic Assessment:
- Esophagoscopy & Endoscopic Ultrasound (EUS)
- Endobronchial Ultrasound (EBUS)
- Mediastinoscopy
- Mediastinal Lymph Node Dissection (MLND)
Approach to Lymph Node Sampling
Anterior Mediastinotomy (Chamberlain Procedure)
- Samples: Aortic Nodes
- Station 5 (Aortopulmonary Window)
- Station 6 (Para-Aortic)
- Procedure: Left Anterior Thoracotomy & Parasternal Mediastinoscopy
- Relative Contraindications:
- Large Ascending Aortic Aneurysm
- Past Thoracic Surgery or Radiation
- SVC Syndrome
Esophagoscopy & Endoscopic Ultrasound (EUS)
- Samples: Posterior-Inferior Mediastinum
- Station 8 (Paraesophageal – Below Carina)
- Station 9 (Pulmonary Ligament)
Endobronchial Ultrasound (EBUS)
- Samples: Anterior/Superior Mediastinum & Intrapulmonary
- Anterior/Superior Mediastinum
- Station 1 (Low Cervical)
- Station 2 (Paratracheal – Upper)
- Station 4 (Paratracheal – Lower)
- Station 7 (Subcarinal)
- Intrapulmonary
- Station 10 (Hilar)
- Station 11 (Interlobar)
- Station 12 (Lobar)
Mediastinoscopy
- *Old Gold Standard Before Endoscopic Procedures
- Samples: Stations 2, 4 & 7
- Would Still Need Mediastinotomy for Aortopulmonary Nodes
Mediastinal Lymph Node Dissection (MLND)
- Intraoperative Staging During Lung Resection
- Gold Standard Although Clinical Use is Controversial & Many Prefer Systematic Sampling
- Samples: Stations 2R, 4R & 5-10
- Can Also Access Station 3 if Necessary
Staging
TNM Staging
| T | N | M | |
| 1 | ≤ 3 cm
1a: ≤ 1 cm 1b: > 1 cm 1c: > 2 cm |
Ipsilateral Peribronchial or Hilar LN, or Intrapulmonary LN | 1a: Separate Nodule in Contralateral Lobe, Malignant Pleural Effusion or Malignant Pericardial Effusion
1b: Single Extrathoracic Met 1c: Multiple Extrathoracic Mets |
| 2 | > 3 cm but ≤ 5 cm or Involves the Main Bronchus, Invades Visceral Pleura or Has Associated Atelectasis or Obstructive Pneumonitis
2a: > 3 cm 2b: > 4 cm |
Ipsilateral Mediastinal or Subcarinal LN | |
| 3 | > 5 cm but ≤ 7 cm
Has Separate Nodule in the Same Lobe Directly Invades the Chest Wall, Phrenic Nerve or Parietal Pericardium |
Contralateral, Scalene or Supraclavicular LN | |
| 4 | > 7 cm
Has a Separate Nodule in a Different Ipsilateral Lobe Invades the Diaphragm, Mediastinum, Heart, Great Vessels, Trachea, Recurrent Laryngeal Nerve, Esophagus, Carina or Vertebral Body |
Stage
| Stage | T | N | M | |
| I | A1 | T1a | N0 | M0 |
| A2 | T1b | N0 | M0 | |
| A3 | T1c | N0 | M0 | |
| B | T2a | N0 | M0 | |
| II | A | T2B | N0 | M0 |
| B | T1-2 | N1 | M0 | |
| T3 | N0 | M0 | ||
| III | A | T1-2 | N2 | M0 |
| T3 | N1 | M0 | ||
| T4 | N0-1 | M0 | ||
| B | T1-2 | N3 | M0 | |
| T3-4 | N2 | M0 | ||
| C | T3-4 | N3 | M0 | |
| IV | A | Any T | Any N | M1a-b |
| B | Any T | Any N | M1c | |
References
- Carvalho A, Correia R, Sá Fernandes M, Pinheiro J, Leitão P, Padrão E, Pinto D, Pereira JM. Pulmonary inflammatory myofibroblastic tumor: report of 2 cases with radiologic-pathologic correlation. Radiol Case Rep. 2017 Apr 1;12(2):251-256.(License: CC BY-NC-ND-4.0)
- Ozkaya S, Findik S, Atici AG. Penile metastasis as a first sign of lung cancer. Int Med Case Rep J. 2009 Jul 16;2:19-21. (License: CC BY-NC-3.0)