Pancreaticoduodenectomy (Whipple Procedure)
David Ray Velez, MD
The Operative Review of Surgery. 2023; 1:20-28.
Table of Contents
General Information
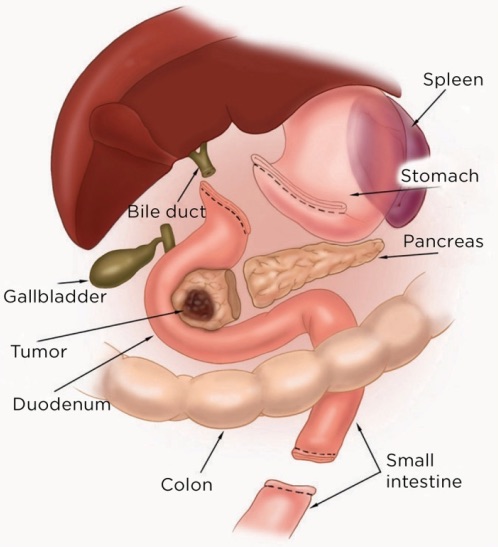
Definition
- Resection of Pancreatic Head & Duodenum 1
Resection Contents by a Classic Pancreaticoduodenectomy 1
- Pancreatic Head & Duodenum
- Gallbladder & Common Bile Duct (CBD)
- Gastric Antrum & Pylorus
- *Some Prefer a Pylorus-Preserving Technique
- Proximal Jejunum (15 cm)
Indications
- Pancreatic Head Malignancy
- Exocrine Cancer/Adenocarcinoma
- Pancreatic Neuroendocrine Tumor (PNET)
- Cyst Concerning for Malignancy
- Metastases
- Distal Common Bile Duct (CBD) Cholangiocarcinoma
- Periampullary Duodenal Adenocarcinoma
- Chronic Pancreatitis with Small-Normal Ducts, Isolated to the Head
- Trauma (Never Emergent)
Unresectable Definitions
Preoperative Biliary Drainage
- Methods:
- Endoscopic Retrograde Cholangiopancreatography (ERCP)
- Percutaneous Transhepatic Cholangiography (PTC)
- Theory: Some Animal Studies Saw Improved Liver Function & Perioperative Complications (Not Seen in Human Clinical Trials) 3
- Clinical Trials:
- No Improved Morbidity or Mortality 3
- Increased Risk of Wound Infection, Pancreatic Fistula, & Costs 3
- Routine Use Should Be Avoided 3
Whipple Resection 2
Technique
Abdominal Exploration
- Start with an Initial Staging Laparoscopy 4
- Limited Midline Laparotomy May Also Be Considered 4
- *Can Forgo if Procedure is Being Performed for a Non-Malignant Pathology
- Evaluate for Evidence of Tumor Metastases
- Examine All Visceral Surfaces, Peritoneal Surfaces, Omentum, & Bowel
- Hepatic Lesions May Be Further Characterized by Intraoperative US or Biopsy with Frozen Section 4
- Evidence of Metastases Should Prompt Abortion of Case
Dissection
- Convert to an Open Laparotomy Through Midline Incision
- *Can Consider Minimally Invasive Surgery (MIS) Approaches (Laparoscopic/Robotic)
- Perform a Generous Kocher Maneuver
- Extend to the Level of the Renal Veins
- Mobilizes Duodenum, Pancreatic Head & Stomach
- May Also Require Mobilization of the Hepatic Flexure
- Enter the Lesser Sac Through the Gastrocolic Ligament
- Isolate the Portal Structures (Common Hepatic/Bile Duct, Common Hepatic Artery, & Portal Vein)
- Monitor for & Preserve a Replaced Right Hepatic Artery
Resection Mn
- Cholecystectomy & Common Hepatic Duct (CHD) Transection
- Divide the CHD Just Proximal to the Cystic Duct
- Divide the Gastroduodenal Artery (GDA)
- Divide as it Originates Off the Common Hepatic Artery (CHA)
- Test-Clamp GDA Prior to Division – Ensure Adequate Flow in the Proper Hepatic Artery (PHA)
- Celiac Stenosis Can Result in Hepatic Arterial Supply from the GDA in a Retrograde Fashion 5
- Transect the Stomach
- Transect 2 cm Proximal to the Pylorus
- Transect the Proximal Jejunum
- Mobilize & Transect 15-20 cm Distal to the Ligament of Treitz
- Divide the Mesentery & Pass Bowel Underneath the Superior Mesenteric Vessels to the Patient’s Right
- Transect the Neck of the Pancreas
- Transection Plane Created by Developing a Tunnel Anterior to the SMV (Posterior to the Pancreatic Neck)
- Retract Specimen Medially Off the SMV-Portal Vein Confluence
- Exposes Inferior Pancreaticoduodenal Arteries – Carefully Ligate Branches to Avoid Avulsion
- Lymphadenectomy
- Include Regional Lymph Nodes Along the CBD, CHA, Portal Vein, & Pancreaticoduodenal Arteries
- Minimum 12 Lymph Nodes Recommended 6
Reconstruction
- Pancreaticojejunostomy (PJ)
- At the Most Proximal Aspect
- Responsible for the Majority of Postoperative Morbidity
- Techniques: 7
- Invagination Techniques
- Duct-to-Mucosa Techniques
- Pancreaticogastrostomy (PG) Anastomosis – Less Common 8
- *Various Anastomotic Techniques – None Have Been Proven to Be Superior 7
- Hepaticojejunostomy (HJ)
- Created 5-10 cm Distal to PJ Anastomosis to Prevent Backflow
- Gastrojejunostomy (GJ)
- Created ≥ 30-40 cm (Often 45-60 cm) Distally to Prevent Food Reflux into Biliary/Pancreatic Anastomoses
- Can Be Performed in an Antecolic or Retrocolic Fashion 9
Drains & Closure
- Leave 1-2 Closed-Suction Drains Anterior/Posterior to the HJ & PJ to Monitor for Leak/Fistula
- Can Potentially Omit Drains in Patients at Negligible- or Low-Risk for Pancreatic Fistula 11
- Generally Prefer Early Removal Based on Drain Amylase 11
- Drain Amylase Checked on Postoperative Day #1 & #3 (Remove if < 5000 U/L) 11
- Close Abdomen
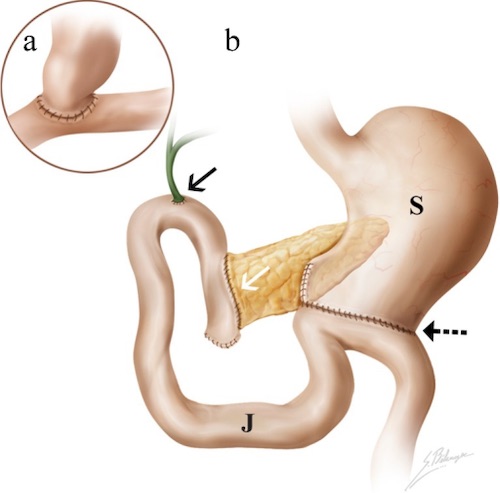
Whipple Reconstruction 10
Pylorus-Preserving Pancreaticoduodenectomy (PpPD)
- Definition: A Pancreaticoduodenectomy that Preserves the Gastric Antrum, Pylorus, & Proximal Duodenum (3-4 cm) 12,13
- Proximal Duodenum is then Anastomosed to the Jejunum (Duodenojejunostomy – DJ)
- Theory: Preservation of the Pylorus Preserves Normal Physiologic Gastric Emptying
- Some Believe it Could Improve Nutritional Status and Decrease the Incidence of Associated Complications Such as Dumping Syndrome, Marginal Ulcer, & Bile Reflux Gastritis (Debated) 14
- Contraindications: Involvement of First Portion of the Duodenum, Pylorus, or Antrum
- Comparison to Classic Pancreaticoduodenectomy for Cancer: 15
- Faster Procedure & Lower Blood Loss 15
- No Significant Difference in Outcomes or Long-Term Survival 15
Complications
General Risk
- Morbidity 30-60% 16
- Mortality < 4% (1% in High-Volume Centers) 17
- 5-Year Survival for Complete Resection: 20-30%
Delayed Gastric Emptying (DGE/Gastroparesis)
- The Most Common Complication After Pancreaticoduodenectomy
- Risk: 17% 18
- Multifactorial Causes: 17
- Decreased Motilin (From Duodenal Resection)
- Dissected Vagal & Sympathetic Innervation to the Antrum/Pylorus
- Decreased Blood Flow to the Antrum/Pylorus
- Pancreatic Fistulae
- Risk Factors: 19,20
- Prior Abdominal Surgery
- History of Cholangitis
- Diabetes
- Preoperative Biliary Stenting
- Pylorus Resection
- Longer Operating Times
- Presentation:
- Bloating
- Abdominal Pain
- Nausea & Vomiting
- Diet Intolerance & Early Satiety
- International Study Group of Pancreatic Surgery (ISGPS) 2007 Classification: 21
- Grade A
- Nasogastric Tube (NGT) Required 4-7 Days
- Unable to Tolerate Oral Diet After 7 Days
- Grade B
- Nasogastric Tube (NGT) Required 8-14 Days
- Unable to Tolerate Oral Diet After 14 Days
- Grade C
- Nasogastric Tube (NGT) Required > 14 Days
- Unable to Tolerate Oral Diet After 21 Days
- Grade A
- Treatment: Metoclopramide (Reglan) or Erythromycin
- Generally Self-Limiting
- May Require Nasogastric Tube (NGT) for Decompression or Nasojejunal Tube for Enteral Nutrition
Postoperative Pancreatic Fistula (POPF)
- Risk for Clinically Relevant POPF (Grade B/C): 5-10% 22
- Definitions, Presentation, & Treatment:
Postpancreatectomy Hemorrhage (PPH)
- Risk: 12.2% 16
- High Mortality (21%) 23
- International Study Group of Pancreatic Surgery (ISGPS) 2007 Classification: 24
- Parameters:
- Onset: Early (≤ 24 Hours After Index Operation) or Late (> 24 Horus)
- Location: Intraluminal or Extraluminal
- Severity: Mild or Severe
- Grade A: Early & Mild
- Grade B: Early & Severe or Late & Mild
- Grade C: Late & Severe
- Parameters:
- Early Hemorrhage (< 24 Hours) is Generally Due to Inadequate Hemostasis 23
- Late Hemorrhage (> 24 Hours) is Often Associated with a Postoperative Pancreatic Fistula (POPF) 23
- Leakage of Pancreatic Enzymes Erodes the Peri-Pancreatic Vessels
- Origins: 23
- Gastroduodenal Artery (GDA) Stump (29%) – Most Common
- Common Hepatic Artery (CHA) (19%)
- Splenic Artery (12%)
- Superior Mesenteric Artery (SMA)
- Proper Hepatic Artery (PHA)
- Diagnosis: CT Angiography (CTA)
- Treatment:
- Early PPH:
- Intraluminal: Endoscopy 25
- Extraluminal: Repeat Laparotomy 25
- Late PPH: Angioembolization 25
- Tissue Friable and Difficult to Control in OR
- May Require Repeat Laparotomy If Fails 25
- Early PPH:
Early Biliary Complications
- Bilioenteric Structure
- Risk: 2.6% 26
- Presentation: New Onset Jaundice with Continuously Increasing Serum Bilirubin 27
- Diagnosis: US or CT
- Treatment: Percutaneous Transhepatic Cholangiography (PTC) with Balloon Dilation and Stenting 26,27
- May Consider Repeat Laparotomy & Anastomotic Revision 26
- Biliary Leak
- Leak from the Hepaticojejunostomy (HJ)
- Risk: 1-3% 28
- Treatment: Percutaneous Drainage Until Resolution 27
- May Consider Repeat Laparotomy & Anastomotic Revision for Sepsis or Persistent High-Output Fistulas 27
Additional Complications
- Wound Infection
- Risk: 10-40% 4
- Marginal Ulcer
- Risk: 5-7% 29,30
- Risk Factors: 29
- Discontinuation of PPI
- Smoking
- Alcohol
- Non-Steroidal Anti-Inflammatory Drugs (NSAID’s)
- Management PPI & Endoscopic Surveillance 29
- New-Onset Diabetes (Endocrine Insufficiency)
- Risk of New-Onset Diabetes: 16% 31
- Risk of Insulin-Dependent New-Onset Diabetes: 6% 31
Mnemonics
Remember the Steps of Dissection & Resection
- Consider the Surgical Technique as the Face of a Clock
- Procedure Moves Systematically in a Clockwise Manner
- 1. Extended Kocher Maneuver
- 2. Isolate the Portal Structures with Cholecystectomy & Divide the CHD
- 3. Divide the GDA
- 4. Transect the Stomach
- 5. Transect the Proximal Jejunum
- 6. Create the SMV Tunnel & Transect the Pancreas
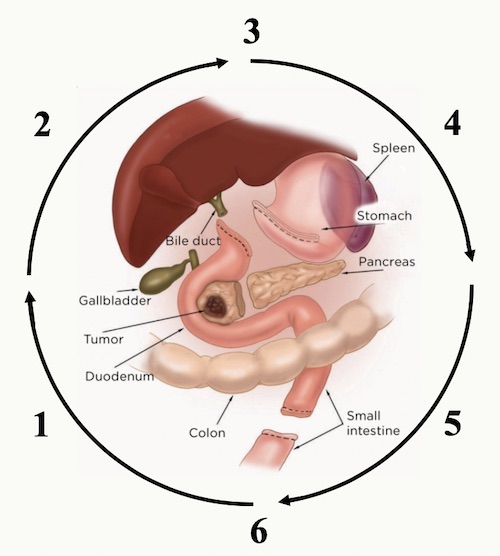
Clockwise Approach to a Whipple 32
References
- Whipple AO, Parsons WB, Mullins CR. TREATMENT OF CARCINOMA OF THE AMPULLA OF VATER. Ann Surg. 1935 Oct;102(4):763-79.
- Reynolds RB, Folloder J. Clinical Management of Pancreatic Cancer. J Adv Pract Oncol. 2014 Sep-Oct;5(5):356-64. (License: CC BY-2.0)
- Wang C, Xu Y, Lu X. Should preoperative biliary drainage be routinely performed for obstructive jaundice with resectable tumor? Hepatobiliary Surg Nutr. 2013 Oct;2(5):266-71.
- Sham JG, Reames BN, He J. Management of Periampullary Cancers. In: Cameron JL, Cameron AM. Current Surgical Therapy, 13e. 2020. Elsevier. Philadelphia, PA.
- Kurosaki I, Hatakeyama K, Nihei KE, Oyamatsu M. Celiac axis stenosis in pancreaticoduodenectomy. J Hepatobiliary Pancreat Surg. 2004;11(2):119-24.
- Tomlinson JS, Jain S, Bentrem DJ, Sekeris EG, Maggard MA, Hines OJ, Reber HA, Ko CY. Accuracy of staging node-negative pancreas cancer: a potential quality measure. Arch Surg. 2007 Aug;142(8):767-723; discussion 773-4.
- Olakowski M, Grudzińska E, Mrowiec S. Pancreaticojejunostomy-a review of modern techniques. Langenbecks Arch Surg. 2020 Feb;405(1):13-22.
- Cheng Y, Briarava M, Lai M, Wang X, Tu B, Cheng N, Gong J, Yuan Y, Pilati P, Mocellin S. Pancreaticojejunostomy versus pancreaticogastrostomy reconstruction for the prevention of postoperative pancreatic fistula following pancreaticoduodenectomy. Cochrane Database Syst Rev. 2017 Sep 12;9(9):CD012257.
- Wang CY, Huang TS, Zhang KD, Wang ZZ, Wang F, Zhao ZM, Gao YX, Liu R. Retrocolic versus antecolic gastrointestinal reconstruction in robotic pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci. 2019 Nov;26(11):517-523.
- Terrone DG, Lepanto L, Billiard JS, Olivié D, Murphy-Lavallée J, Vandenbroucke F, Tang A. A primer to common major gastrointestinal post-surgical anatomy on CT-a pictorial review. Insights Imaging. 2011 Dec;2(6):631-638. (License: CC BY-2.0)
- Marchegiani G, Bassi C. Prevention, prediction, and mitigation of postoperative pancreatic fistula. Br J Surg. 2021 Jun 22;108(6):602-604.
- Watson Treatment of carcinomaof the ampulla of Vater: successful radical resection. Br J Surg 1944; 31: 368-373.
- Traverso LW, Longmire WP Jr. Preservation of the pylorus in pancreaticoduodenectomy. Surg Gynecol Obstet. 1978 Jun;146(6):959-62.
- Kawai M, Yamaue H. Pancreaticoduodenectomy versus pylorus-preserving pancreaticoduodenectomy: the clinical impact of a new surgical procedure; pylorus-resecting pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci. 2011 Nov;18(6):755-61.
- Diener MK, Fitzmaurice C, Schwarzer G, Seiler CM, Antes G, Knaebel HP, Büchler MW. Pylorus-preserving pancreaticoduodenectomy (pp Whipple) versus pancreaticoduodenectomy (classic Whipple) for surgical treatment of periampullary and pancreatic carcinoma. Cochrane Database Syst Rev. 2011 May 11;(5):CD006053.
- Karim SAM, Abdulla KS, Abdulkarim QH, Rahim FH. The outcomes and complications of pancreaticoduodenectomy (Whipple procedure): Cross sectional study. Int J Surg. 2018 Apr;52:383-387.
- Simon R. Complications After Pancreaticoduodenectomy. Surg Clin North Am. 2021 Oct;101(5):865-874.
- Traverso LW, Hashimoto Y. Delayed gastric emptying: the state of the highest level of evidence. J Hepatobiliary Pancreat Surg. 2008;15(3):262-9.
- Bilgiç Ç, Sobutay E, Bilge O. Risk Factors for Delayed Gastric Emptying After Pancreaticoduodenectomy. Pancreas. 2022 May 1;51(5):496-501.
- Robinson JR, Marincola P, Shelton J, Merchant NB, Idrees K, Parikh AA. Peri-operative risk factors for delayed gastric emptying after a pancreaticoduodenectomy. HPB (Oxford). 2015 Jun;17(6):495-501.
- Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW, Yeo CJ, Büchler MW. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007 Nov;142(5):761-8.
- Lai EC, Lau SH, Lau WY. Measures to prevent pancreatic fistula after pancreatoduodenectomy: a comprehensive review. Arch Surg. 2009 Nov;144(11):1074-80.
- Floortje van Oosten A, Smits FJ, van den Heuvel DAF, van Santvoort HC, Molenaar IQ. Diagnosis and management of postpancreatectomy hemorrhage: a systematic review and meta-analysis. HPB (Oxford). 2019 Aug;21(8):953-961.
- Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Yeo CJ, Büchler MW. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007 Jul;142(1):20-5.
- Yekebas EF, Wolfram L, Cataldegirmen G, Habermann CR, Bogoevski D, Koenig AM, Kaifi J, Schurr PG, Bubenheim M, Nolte-Ernsting C, Adam G, Izbicki JR. Postpancreatectomy hemorrhage: diagnosis and treatment: an analysis in 1669 consecutive pancreatic resections. Ann Surg. 2007 Aug;246(2):269-80.
- House MG, Cameron JL, Schulick RD, Campbell KA, Sauter PK, Coleman J, Lillemoe KD, Yeo CJ. Incidence and outcome of biliary strictures after pancreaticoduodenectomy. Ann Surg. 2006 May;243(5):571-6; discussion 576-8.
- Malgras B, Duron S, Gaujoux S, Dokmak S, Aussilhou B, Rebours V, Palazzo M, Belghiti J, Sauvanet A. Early biliary complications following pancreaticoduodenectomy: prevalence and risk factors. HPB (Oxford). 2016 Apr;18(4):367-74.
- Malgras B, Duron S, Gaujoux S, Dokmak S, Aussilhou B, Rebours V, Palazzo M, Belghiti J, Sauvanet A. Early biliary complications following pancreaticoduodenectomy: prevalence and risk factors. HPB (Oxford). 2016 Apr;18(4):367-74.
- Sulieman I, Strobel O, Scharenberg C, Mihaljevic AM, Müller BM, Diener MK, Mehrabi A, Schneider M, Berchtold C, Tjaden C, Hinz U, Feisst M, Büchler MW, Hackert T, Loos M. Symptomatic marginal ulcer after pancreatoduodenectomy. Surgery. 2020 Jul;168(1):67-71.
- Park Y, Hwang DW, Lee JH, Song KB, Jun E, Lee W, Kwon J, Kim SC. Analysis of Symptomatic Marginal Ulcers in Patients Who Underwent Pancreaticoduodenectomy for Periampullary Tumors. Pancreas. 2020 Feb;49(2):208-215.
- Scholten L, Mungroop TH, Haijtink SAL, Issa Y, van Rijssen LB, Koerkamp BG, van Eijck CH, Busch OR, DeVries JH, Besselink MG. New-onset diabetes after pancreatoduodenectomy: A systematic review and meta-analysis. Surgery. 2018 May 17:S0039-6060(18)30081-3.
- Reynolds RB, Folloder J. Clinical Management of Pancreatic Cancer. J Adv Pract Oncol. 2014 Sep-Oct;5(5):356-64. (License: CC BY-2.0) Edited by The Operative Review of Surgery