Trauma: Pelvic Fracture
Pelvic Fracture
General
- Bimodal Distribution
- Teens/Young Adults – High-Energy Unstable Fracture
- Elderly – Low-Energy Fractures
- Most Common Cause: MVC
- “Open Book” Fracture – Fracture with Significant Pelvic Ring Disruption
- Combined Anterior & Posterior Injury
- If Anterior Ring is Widened > 2.5 cm There is Increased Risk of Posterior Injury & Hemorrhage
- Most Feared Complication is Rapid & Uncontrolled Hemorrhage
- > 1/3 Will Require Transfusion During Their Hospital Stay
Fracture Type – Young & Burgess Classification
- Lateral Compression (LC)
- Type 1: Unilateral Sacral Fracture & Pubic Rami Fracture
- Most Common Lateral Fracture Type
- Type 2: Unilateral Crescent (Iliac Wing) Fracture
- Type 3: Type I or II with Contralateral Open Book Injury
- “Wind-Swept Pelvis”
- Type 1: Unilateral Sacral Fracture & Pubic Rami Fracture
- Anterior-Posterior Compression (APC)
- Type 1: Symphysis Widening < 2.5 cm, Posterior Ligaments Intact
- Type 2: Symphysis Widening > 2.5 cm, Anterior SI Opening, Posterior SI Ligament Intact
- Type 3: Complete Disruption of Symphysis & SI Ligaments
- Vertical Shear (VS): Vertical Displacement of Hemipelvis with Anterior & Posterior Injury
- Combined Mechanism (CM): Combination of Any of the Above
Bleeding Source
- Venous Plexus (Most Common Source, 80-90%)
- From Shearing of Posterior Plexus
- Tends to Be Self-Limited and Hematoma Tamponades
- Fixation Will Also Tamponade Most Venous Bleeding
- Arterial (10-20%)
- Often in Posterior Fractures from Shearing/Compression of Iliac Vessels Against the Pelvic Brim
- Most Common Artery: Superior Gluteal Artery
- More Likely to be Unstable
- Cancellous Bone
Diagnosis
- Lower Extremity External Rotation & Limb-Length Discrepancy
- Mobility with Gentle Compression of Iliac Crests & Distraction
- Do Not ‘Rock’/‘Spring’ & Only Preform Once
- Low Sensitivity
- Dx: XR or CT

Open Book Pelvic Fracture 1
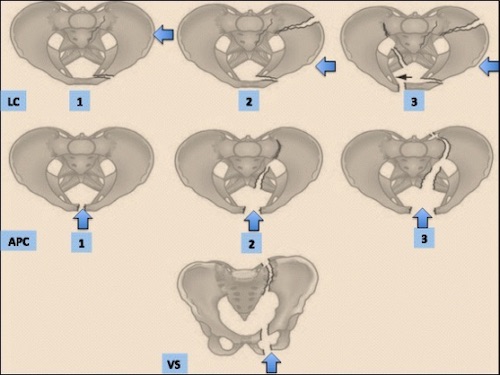
Young & Burgess Classification 2
Treatment
Initial Management if Concerned for Instability or Major Bleeding
- Initial Management: Pelvic Binder
- Reduce Pelvic Volume to Tamponade Venous Bleeding & Limit Fracture Motion
- Technique: Bed Sheet or Commercial Devices
- Snug but Not Overtight at the Level of the Greater Trochanter
- *Theoretically, Binders Can Worsen Displacement of Lateral Compression Fractures & Worsen Bleeding – Some Recommend Against Binders in These Situations Although There is No Clinical Evidence of Significant Harm
- If Unavailable: External Fixation Can Tamponade
Hemorrhage Control
- Angioembolization
- Indications:
- Unstable
- Large Hematoma
- Pseudoaneurysm
- Contrast Extravasation
- Transfusion ≥ 4 U
- Complications: Impotence or Pelvic/Gluteal Ischemia
- Proceed with External Fixation to Tamponade Venous Bleeding if There Continues to Be Evidence of Bleeding After Embolization
- Indications:
- Laparotomy
- Difficult to Visualize & Can Restart Bleeding
- Consider for Unstable Patients with Absent Unilateral Femoral Pulse
- Likely Common/External Iliac Artery Injury
- Other Options:
- REBOA in Zone III
- Preperitoneal Packing (PPP)
- Procedure:
- 8 cm Lower Midline or Pfannenstiel Incision
- Three Laparotomy Pads Placed on Either Side of the Bladder
- Close and Remove at 24-48 Hour
- If FAST Positive – Laparotomy Should be Preformed & PPP Would Be Contraindicated
- Procedure:
- Hypogastric Artery Ligation
- Early Rigid Fixation
Open Fractures
- Initial: Pack Opening & Pelvic Binder
- Then Angiography Prior to Surgical Exploration
Definitive Treatment
- Stable Pelvic Ring: Conservative Management & Weight Bear as Tolerated
- Include: LC-I, APC-I & Isolated Pubic Rami Fractures
- Unstable Pelvic Ring: Surgical Repair
- Angioembolization First if Indicated – Pelvic Binder Serves Same Purpose as Surgical Fixation Until More Stable for Surgery

Pelvic Binder 3

Pelvic Binder (Before & After) 4

Perperitoneal Packing (D: Completion of Takeback) 5
References
- Finnan RP, Herbenick MA, Prayson MJ, McCarthy MC. Bladder incarceration following anterior external fixation of a traumatic pubic symphysis diastasis treated with immediate open reduction and internal fixation. Patient Saf Surg. 2008 Oct 19;2(1):26. (License: CC BY-2.0)
- Coccolini F, Stahel PF, Montori G, Biffl W, Horer TM, Catena F, Kluger Y, Moore EE, Peitzman AB, Ivatury R, Coimbra R, Fraga GP, Pereira B, Rizoli S, Kirkpatrick A, Leppaniemi A, Manfredi R, Magnone S, Chiara O, Solaini L, Ceresoli M, Allievi N, Arvieux C, Velmahos G, Balogh Z, Naidoo N, Weber D, Abu-Zidan F, Sartelli M, Ansaloni L. Pelvic trauma: WSES classification and guidelines. World J Emerg Surg. 2017 Jan 18;12:5. (License: CC BY-4.0)
- Vaidya R, Roth M, Zarling B, Zhang S, Walsh C, Macsuga J, Swartz J. Application of Circumferential Compression Device (Binder) in Pelvic Injuries: Room for Improvement. West J Emerg Med. 2016 Nov;17(6):766-774. (License: CC BY-4.0)
- Vaidya R, Roth M, Zarling B, Zhang S, Walsh C, Macsuga J, Swartz J. Application of Circumferential Compression Device (Binder) in Pelvic Injuries: Room for Improvement. West J Emerg Med. 2016 Nov;17(6):766-774. (License: CC BY-4.0)
- Jang JY, Shim H, Jung PY, Kim S, Bae KS. Preperitoneal pelvic packing in patients with hemodynamic instability due to severe pelvic fracture: early experience in a Korean trauma center. Scand J Trauma Resusc Emerg Med. 2016 Jan 13;24:3. (License: CC BY-4.0)