Skin & Soft Tissue: Soft Tissue Sarcoma
Soft Tissue Sarcoma
Presentation
- Most Common Presentation: Large, Gradually Enlarging, Painless Mass
- Can Cause Compression/Pain in Adjacent Nerves
- Most Common Location: Thigh, Buttock or Groin
Genetic Syndromes
- Common Associations:
- Neurofibromatosis Type 1
- Neurofibromatosis Type 2
- Tuberous Sclerosis
- Li-Fraumeni Syndrome
- Gardner’s Syndrome
- *See Oncology: Hereditary Cancer Syndromes
Prognosis/Metastasis
- Most Tend to Grow Locally & Invade Adjacent Tissues
- Most Have High Risk of Local Recurrence After Excision
- Most Important Staging Factors: Histologic Grade, Size & N/M Status
- Metastases are Most Common in Children
- Pattern of Spread:
- Hematogenous – Most Common
- Lymphatic: Synovial, Clear Cell, Angiosarcoma, Rhabdomyosarcoma & Epithelial Mn
- Most Common Site of Metastasis: Lung
Diagnosis
- Initial Diagnostic Step: MRI (Evaluate Etiology, Extent & Invasion)
- May Consider CT Instead for Abdominal or Retroperitoneal Lesions
- Consider CT Chest for All Lesions to Evaluate for Pulmonary Metastases
- Imaging Not Required for Kaposi Sarcoma
- Imaging Generally Done Prior to Biopsy (Postprocedural Edema May Make MRI Difficult to Interpret)
- Biopsy (After Imaging):
- Preferred Method: Core Need Biopsy (CNB)
- *Incisional Biopsy was the Historic Gold Standard but Now Replaced by CNB
- May Consider Excisional Biopsy if Small (< 4-5 cm)
- Preferred Method: Core Need Biopsy (CNB)
Soft Tissue Sarcoma – Staging
TNM
| T | N | M | G (Histology Grade) | |
| 1 | ≤ 5.0 cm | LN+ | M+ | Score 2-3 |
| 2 | > 5.0 cm | Score 4-5 | ||
| 3 | > 10.0 cm | Score 6-8 | ||
| 4 | > 15.0 cm |
- *Grade Scores from 2-8 Based on Differentiation, Mitotic Count & Extent of Tumor Necrosis
- *Not Used for GIST, Osteosarcoma or Kaposi Sarcoma
Trunk/Extremity Stage Mn
| Stage | T | N | M | G | |
| I | A | T1 | N0 | M0 | Gx-G1 |
| B | T2-4 | N0 | M0 | Gx-G1 | |
| 2 | T1 | N0 | M0 | G2-G3 | |
| 3 | A | T2 | N0 | M0 | G2-G3 |
| B | T3-4 | N0 | M0 | G2-G3 | |
| 4 | Any T | N1 | Any M | Any G | |
| Any T | Any N | M1 | Any G | ||
Retroperitoneum Stage
| Stage | T | N | M | G | |
| I | A | T1 | N0 | M0 | Gx-G1 |
| B | T2-4 | N0 | M0 | Gx-G1 | |
| 2 | T1 | N0 | M0 | G2-G3 | |
| 3 | A | T2 | N0 | M0 | G2-G3 |
| B | T3-4 | N0 | M0 | G2-G3 | |
| Any T | N1 | Any M | Any G | ||
| 4 | Any T | Any N | M1 | Any G | |
Soft Tissue Sarcoma – Types
Gastrointestinal Stromal Tumor (GIST)
Liposarcoma
- Malignant Tumor from Adipocytes
- Most Common Sites: Extremities & Retroperitoneum
- Types:
- Well-Differentiated (De-Differentiated)
- Myxoid (Round Cell)
- Pleomorphic
- Metastatic Potential
- Low-Risk: Well-Differentiated (De-Differentiated)
- High-Risk: Myxoid (Round Cell) or Pleomorphic
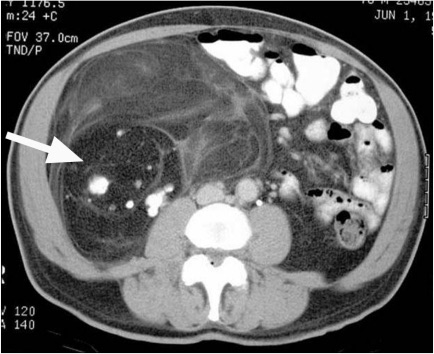
Retroperitoneal Liposarcoma 1
Leiomyosarcoma
- Malignant Tumor from Smooth Muscle Cells
- Most Common Sites: IVC, GI Tract & Uterus
- Worse Prognosis
Leiomyosarcoma of Small Bowel 2
Rhabdomyosarcoma
- Malignant Tumor from Cells that were Destined to Become Skeletal Muscle
- Most Common Soft-Tissue Sarcoma in Peds
- Less Common in Adults
- Most Common Locations: Head & Neck, GI Tract & Extremities
- Classification:
- Embryonal – Most Common, Intermediate Prognosis
- Botryoid – “Grape-Like” Polypoid Mas, Favorable Prognosis
- Alveolar – Poor Prognosis
- Pleomorphic
- Sarcoma Botryoides: Generally Describing Rhabdomyosarcoma of the Vagina
- May Also Be Seen in the Nasopharynx, Bile Ducts or Urinary Bladder
- Contain Desmin (May Also Be Seen in Leiomyosarcoma)
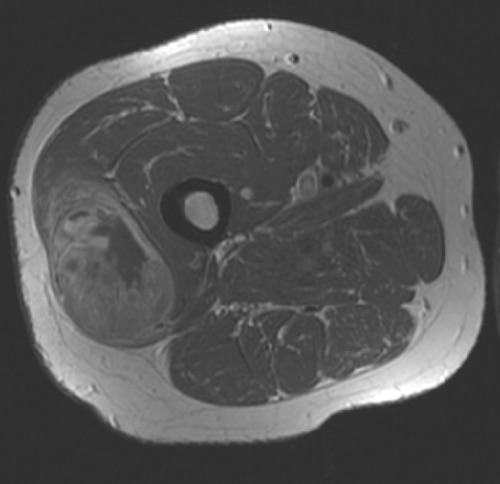
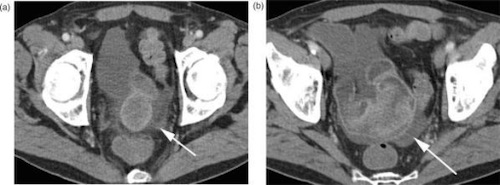
Rhabdomyosarcoma of Thigh 3
Dermatofibrosarcoma Protuberans (DFSP)
- Locally Aggressive Cutaneous Sarcoma with High Risk of Local Recurrence
- Infiltrating Growth Pattern, Commonly Extends Beyond Margins
- Majority (85-90%) are Low-Grade with Low Metastatic Potential
- Exception: Fibrosarcomatous Variant (DFSP-FS) is High-Grade with Increased Risk of Metastasis
- Associated with a t(17;22) Mutation
- Presentation:
- Mostly Asymptomatic
- Early:
- Indurated Plaque
- Overlying Skin Can Be Normal, Brown-Yellow, Red or Atrophic
- Margins Violet-Red or Blue
- Later:
- Raised, Firm Nodule
- Surrounding Skin Telangiectatic
- Can Ulcerate & Bleed
- Most Common Sites:
- Trunk (42%)
- Lower Extremities (21%)
- Upper Extremities (21%)
- Head & Neck (13%)
- Genitals (1%)
- Histology: Finger-Like Projections of Spindle Cells in an Irregularly Whorled/“Storiform” Pattern

Dermatofibrosarcoma Protuberans 4
Osteosarcoma
- Malignant Tumor of Bone
- Bimodal Age Distribution – Peds (13-16 Years) & Elderly (>65)
- Most Common in the Metaphysis of Long Bones
- Most Common Sites: Distal Femur (75%), Proximal Tibia & Proximal Humerus
- May Be Associated with Pathologic Fractures
- Imaging May Demonstrate:
- “Codman Triangle” – Single or Multilayered Periosteal Reaction with Shells of New Ossified Bone Due to Speed of Growth
- “Sunburst” – Sharpey’s Fibers Extend Perpendicularly to Bone When Lesions Grow Too Fast to Ossify a New Layer

Osteosarcoma with Codman Triangles & Sunburst Appearance 5
Synovial Sarcoma
- Histologically Similar to Synovial Cells Although Origin is Unknown
- Most Common in Extremities of Young Adults
- Many are Associated with the Chromosomal Translocation t(X;18)(p11;q11)
Angiosarcoma
- Highly Malignant Tumor of Blood Vessels or Lymphatics
- Types:
- Hemangiosarcoma – From Blood Vessels
- Lymphangiosarcoma – From Lymphatics
- Most Common in Breast, Head or Neck
- Risk Factors:
- Radiation Exposure – May Be Seen After Treatment for Breast Cancer or Lymphoma
- PVC
- Arsenic
- Lymphangiosarcoma is Often Associated with Chronic Lymphedema
- Highly Sensitive to Chemotherapy

Radiation-Induced Angiosarcoma 6
Kaposi Sarcoma
- Angioproliferative Tumor of Blood Vessels or Lymphatics Caused by Human Herpes Virus 8 (HHV-8)
- Most Common AIDS-Associated Malignancy
- Types:
- Classic – Seen in Elderly Men, Most Common in Legs/Feet
- Endemic – Seen in Sub-Saharan Indigenous Africans
- Iatrogenic – Associated with Immunosuppression, Often After Transplants
- Epidemic – AIDS-Associated
- Presentation:
- Purple or Reddish-Blue Macules or Skin Nodules
- May Ulcerate or Bleed
- Very Slow Growing
- Low Mortality Risk

Kaposi Sarcoma 7
Malignant Peripheral Nerve Sheath Tumor (MPNST)
- Malignant Tumor of Peripheral Nerves
- Half are Associated with Neurofibromatosis Type 1
- May Express S100 Protein – Not Seen in All
Undifferentiated/Unclassified (Sarcoma, Not Otherwise Specified)
- Previously Called “Malignant Fibrous Histiosarcoma (MFH)”
- Previously was Considered the Most Common Type of Sarcoma – No Longer True as Many Previously Unidentified Sarcomas Have Been Reclassified
Soft Tissue Sarcoma – Treatment
General Treatment
- Primary Treatment: Wide Local Excision (WLE)
- Margins: 1-2 cm
- Failure to Obtain Oncologically Appropriate Margins: Re-Resection vs Radiation Therapy
- May Consider Observation for Stage IA
- Failure to Obtain Oncologically Appropriate Margins: Re-Resection vs Radiation Therapy
- Consider Amputation If Unresectable
- Margins: 1-2 cm
- Neoadjuvant/Adjuvant Therapy:
- XRT: Consider for ≥ Stage II or Close Margins
- Chemotherapy: Consider for ≥ Stage III
- Metastases:
- Isolated: Resect
- Systemic Disease: Palliative Chemo-XRT
Dermatofibrosarcoma Protuberans (DFSP)
- Primary Treatment: WLE (2-4 cm Margins)
- May Consider Mohs Micrographic Surgery if Large, Recurrent or Cosmetically Sensitive Area
- May Consider Adjuvant Radiation Therapy
- Metastases:
- Resectable: Surgical Resection
- Unresectable: Imatinib (Tyrosine Kinase Inhibitor)
Kaposi Sarcoma
- Classic Kaposi Sarcoma:
- Asymptomatic: Can Observe
- Symptomatic or Cosmetically Unacceptable: Local Treatment
- Surgical Excision
- Radiation Therapy
- Liquid Nitrogen Cryotherapy
- Intralesional Injections
- AIDS-Associated: Highly Active Antiretroviral Therapy (HAART) & Palliation
- May Consider Local Treatment of a Specific Symptomatic Lesion
Follow Up
- Physical Exam:
- Every 3-6 Months for 2-3 Years
- Then:
- Stage I: Annually
- Stage II-III: Every 6 Months for 2 Years, Then Annually
- Imaging:
- Periodic Imaging (CXR & CT/MRI)
Mnemonics
Soft Tissue Sarcomas That Spread by Lymphatics
- “SCARE”
- Synovial
- Clear Cell
- Angiosarcoma
- Rhabdomyosarcoma
- Epithelial
Soft Tissue Sarcoma TNM Staging
- Grade 1 – Stage 1
- Grade 2-3 – Stage 2-3
- N – Stage 4 (Trunk/Extremity) or Stage 3B (Retroperitoneum)
References
- Francis IR, Cohan RH, Varma DG, Sondak VK. Retroperitoneal sarcomas. Cancer Imaging. 2005 Aug 23;5(1):89-94. (License: CC BY-4.0)
- Sailer J, Zacherl J, Schima W. MDCT of small bowel tumours. Cancer Imaging. 2007 Dec 17;7(1):224-33. (License: CC BY-4.0)
- Van Rijn RR, Wilde JC, Bras J, Oldenburger F, McHugh KM, Merks JH. Imaging findings in noncraniofacial childhood rhabdomyosarcoma. Pediatr Radiol. 2008 Jun;38(6):617-34. (License: CC BY-NC-2.0)
- Hamid R, Hafeez A, Darzi MA, Zaroo I, Rasool A, Rashid H. Outcome of wide local excision in dermatofibrosarcoma protuberans and use of radiotherapy for margin-positive disease. Indian Dermatol Online J. 2013 Apr;4(2):93-6. (License: CC BY-NC-SA-3.0)
- Plant J, Cannon S. Diagnostic work up and recognition of primary bone tumours: a review. EFORT Open Rev. 2017 Mar 13;1(6):247-253.(License: CC BY-NC-4.0)
- Aljarrah A, Nos C, Clough KB, Lefrere-Belda MA, Lecuru F. A case report on radiation-induced angiosarcoma of breast post skin-sparing mastectomy and reconstruction with transverse rectus abdominal muscle. Ecancermedicalscience. 2014 Feb 17;8:402.(License: CC BY-3.0)
- OpenStax College. Wikimedia Commons. (License: CC BY-3.0)