Spleen: Splenectomy
Splenectomy Vaccination
Vaccinations
- Hemophilus influenzae Type B
- HiB Single Dose
- Meningococcus
- Quadrivalent Conjugate ACWY – 2 Doses ≥ 8 Weeks Apart
- Monovalent Serogroup B Series – 2 Doses ≥ 4 Weeks Apart
- Pneumococcus
- 13-Valent Conjugate (PCV13) – 1 Dose Initially
- 23-Valent Polysaccharide (PPSV23) – 1 Dose After 8 Weeks
Timing
- Elective: Finish 2 Weeks Before – Start 10-12 Weeks Prior
- Emergent: Start 2 Weeks After (Impaired Functional Ab Responses Prior)
- Give Just Prior to Discharge if Concern for Loss to Follow Up
Boosters Mn
- HiB: None
- MCV: Every 5 Years (Quadrivalent Conjugate)
- PCV: After 5 Years & At Age 65 (PPSV23)
- Some Recommend Every 5-7 Years
Splenectomy
Basics
- Preserved Function Requires: 1/3 of Splenic Mass
- Indications:
- Trauma (Most Common Cause)
- ITP (Most Common Elective Cause)
- Hereditary Spherocytosis
- Felty Syndrome
- Splenic Abscess
- Splenic Cyst (Hydatid Cysts)
- Splenic Vein Thrombosis
- Cancer
- Approach Comparison
- Laparoscopic
- Lower Morbidity & Mortality
- Shorter Hospital Stay & Faster Recovery
- Higher OR Cost but Lower Total Cost from Decreased Stay
- Open
- High Risk for Injury to Pancreas
- Laparoscopic
Elective Splenectomy
- Approach: Laparoscopic
- Laparoscopic Approaches:
- Lateral (Right-Lateral Decubitus)
- Most Common Approach
- Anterior
- Indications:
- Massive Splenomegaly (> 23 cm of 3 kg)
- If Another Procedure is Required
- May Require an Accessory Extraction Incision if Too Large
- Indications:
- Posterior
- More Difficult Due to Thick Muscle Mass
- Lateral (Right-Lateral Decubitus)
- Procedure:
- Mobilize Ligaments
- Divide Splenocolic Ligament
- Divide Gastrosplenic Ligament & Short Gastrics
- Ligate Close to Spleen (Avoid Gastric Injury)
- Divide Splenorenal Ligament & Visualize Splenic Vessels
- Resect Spleen
- Divide Splenic Artery & Vein
- Avoid Injury to Tail of Pancreas
- Divide Splenophrenic Ligament (Last)
- Maintains Cephalad/Lateral Retraction
- Spleen Morcellated & Extracted
- Mobilize Ligaments
- Ligate Hilar Vessels Before Splenophrenic Division
Traumatic Splenectomy
- Approach: Open
- Procedure:
- Mobilize Spleen & Pancreatic Tail to Midline Together
- Left Hand Around Spleen & Retract Medially
- Divide Splenophrenic Ligament
- Fully Mobilize
- Divide Gastrosplenic Ligament & Short Gastrics
- Ligate Close to Spleen (Avoid Gastric Injury)
- Divide Splenocolic Ligament
- Divide Gastrosplenic Ligament & Short Gastrics
- Ligate Splenic Artery & Then Splenic Vein
- Avoid Injury to Tail of Pancreas
- Mobilize Spleen & Pancreatic Tail to Midline Together
- Ligate Hilar Vessels After Complete Mobilization
Post-Splenectomy Hematologic Changes
Laboratory Changes
- Leukocytosis (WBC)
- Reliable Markers for Infection After Traumatic Splenectomy:
- WBC > 15,000 on Postoperative Day #5
- Platelet/WBC < 20 on Postoperative Day #5
- Generally Transient Although Lymphocytosis & Monocytosis are More Persistent
- Reliable Markers for Infection After Traumatic Splenectomy:
- Polycythemia (RBC)
- Thrombocytosis (Plt) – Generally Transient
Peripheral Blood Smear Changes
- Howell-Jolly Bodies (Nuclear Fragments)
- Poikilocytosis (Abnormally Shaped RBC)
- Target Cells (Codocyte)
- Spur Cells (Acanthocytes)
- Pappenheimer Bodies (Fe Deposits)
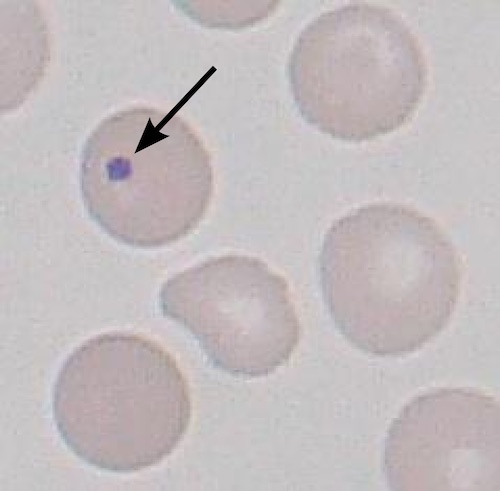
Howell-Jolly Bodies 1
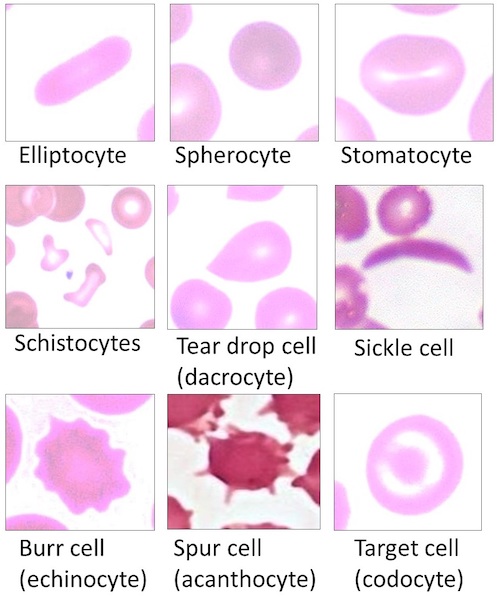
Poikilocytosis 2
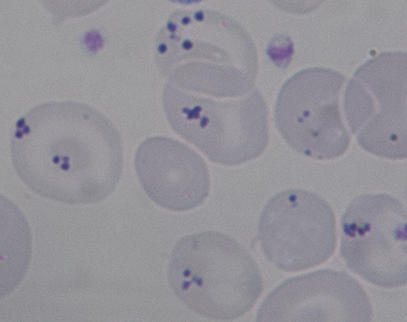
Pappenheimer Bodies 3
Post-Splenectomy Complications
Postoperative Hemorrhage
- Most Common Early Complication
- From Short Gastrics (#1 Most Common) or Splenic Vessels
Overwhelming Post-Splenectomy Infection (OPSI)/Post-Splenectomy Sepsis Syndrome (PSSS)
- Infection Showing Rapid Progression to Sepsis in Post-Splenectomy Patients
- High Mortality
- Cause: Loss of IgM Mediated Immunity to Capsulated Bacteria (HiB, PC & MC)
- Most Common Organism: Pneumococcus
- Most Common Infections: PNA, Primary Bacteremia & Meningitis
- Risk Factors:
- Peds (Especially Age < 5)
- If Splenectomy Due to:
- Malignancy
- Hemolytic Disorder (Thalassemia Major #1, Sickle Cell #2, Hereditary Spherocytosis, ITP)
- Tx: Vancomycin & Ceftriaxone
Antibiotic Prophylaxis
- Possible Indications:
- First Year Post-Splenectomy
- Age < 5 Years
- Immunocompromised
- History of Sepsis from Encapsulated Organisms
- Regimen: Penicillin or Amoxicillin
- If Penicillin Allergy: Cephalosporin
Other Complications
- Pancreatic Leak
- Pancreatic Tail Contained in the Splenorenal Ligament
- May See Postop Fluid Collection in the Lesser Sac
- Splenosis
- Venous Thromboembolism
- Including Portal/Splenic Vein Thrombosis
Mnemonics
Vaccine Booster Frequency After Splenectomy
- H-“IB” – Initial Bolus
- Only Need One Initial Dose
- M-“CV” & P-“CV” – Continued V (5)
- Require Continued Doses After Five Years
References
- Mourao PHO, Haggstrom M. Wikimedia Commons. (License: CC BY-SA-3.0)
- Uthman E, Bhimji S, Haggstrom M. Wikimedia Commons. (License: CC BY-4.0)
- Mourao PHO. Wikimedia Commons. (License: CC BY-SA-4.0)