Endocrine: Thyroid Cancer
Thyroid Cancer
Types of Thyroid Cancer
- Differentiated Thyroid Carcinoma (DTC)
- Papillary Thyroid Carcinoma (PTC)
- Follicular Thyroid Carcinoma (FTC)
- Anaplastic (Undifferentiated) Thyroid Carcinoma (ATC/UTC)
- Medullary Thyroid Carcinoma (MTC)
- Hürthle Cell Carcinoma
- Lymphoma
- Metastasis
Papillary Thyroid Carcinoma (PTC)
- Most Common Thyroid Cancer (Overall, In Pediatrics & in a Thyroglossal Duct Cyst)
- More Common After Childhood Neck Radiation Therapy
- Mutations:
- BRAF
- RET (Not Associated with MEN II)
- NTRK1
- RAS – Less Common than FTC
- *Mutations Tend to Cause Activation of MAPK (Mitogen-Activated Protein Kinase)
- Least Aggressive
- May Be Multifocal (20-30%) – More Common that FTC
- Spread: Lymphatic
- Most Common Site of Mets: Lung
- Histology: Large Cells with Ground Glass Cytoplasm, Orphan Annie Nuclei & Psammoma Bodies Mn
- Orphan Annie Nuclei – Large Washed Out Nuclei (Nuclear Clearing) with Powdery Chromatin & Nuclear Grooves
- Psammoma Bodies – Calcified Clumps
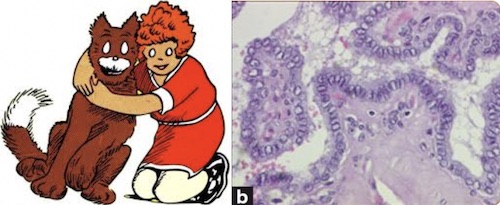
Orphan Annie Nuclei 1
Psammoma Bodies (Arrow) 2
Follicular Thyroid Carcinoma (FTC)
- Mutations:
- PAX8/PPAR-Gamma-1
- RAS – NRAS, HRAS & KRAS
- *Mutations Tend to Cause Activation of AKT Pathway
- Spread: Hematogenous Mn
- Others Have Lymphatic Spread
- Most Common Site of Mets: Bone
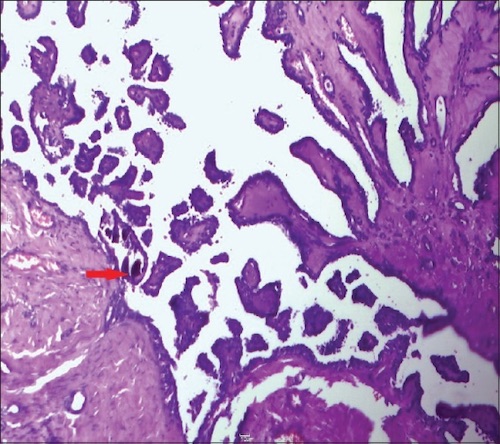
- Histology: Crowded Microfollicles with Absent/Scant Colloid
- More Suspicious if Cells Arranged in Clusters/Clumps with Absence of Follicle Formation
- Unable to Differentiate Carcinoma from Benign Adenoma on FNA Alone – Requires Excision to Determine Capsule/Vascular Invasion
- Noninvasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features (NIFTP)
- No Risk for Metastatic Spread (Not Considered a Malignancy)
- Indistinguishable on FNA & Requires Surgery to Differentiate
Follicular Thyroid Carcinoma 3
Anaplastic (Undifferentiated) Thyroid Carcinoma (ATC)
- Undifferentiated Tumor of Thyroid Follicular Epithelium
- Many Arise from Previously Differentiated (PTC/FTC) Thyroid Carcinoma
- More Common in Elderly with History of Goiter
- Mutations:
- p53
- PIK3CA
- *May See any Mutation Associated with PTC/FTC
- Most Aggressive – Most are Metastatic or Unresectable at Time of Diagnosis
- 90% Have Regional or Distal Spread at Time of Diagnosis
- 15-50% Have Distant Mets at Time of Diagnosis
- Spread: Lymphatic
- Most Common Site of Mets: Lung
- Refractory to Radioactive Iodine (RAI) – Undifferentiated & Do Not Absorb Iodine
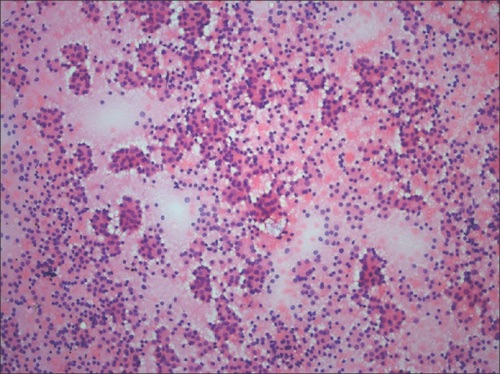
- Histology: Marked Pleomorphism with Spindle Cells & Giant Cells
Anaplastic Thyroid Cancer, Pleomorphic Spindle Cells 4
Medullary Thyroid Carcinoma (MTC)
- Neuroendocrine Tumor of Parafollicular C Cells
- May Produce Calcitonin & CEA
- Mutations: RET
- Most (75%) are Sporadic but 25% are Hereditary (Associated with MEN IIA/IIB)
- Hereditary MTC is Typically Bilateral & Multicentric
- Most Have Already Metastasized at the Time of Diagnosis
- 70% Have Clinically Detectable Cervical Lymph Nodes
- 5-10% Have Distant Mets at Time of Diagnosis
- Refractory to Radioactive Iodine (RAI)
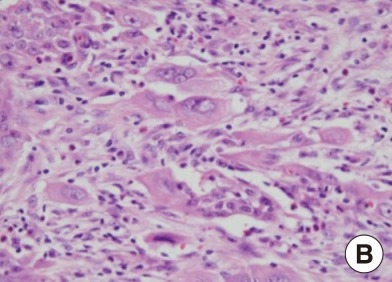
- Histology: Spindle-Shaped Pleomorphic Cells without Follicles, Stain for Calcitonin & Amyloid in Stroma
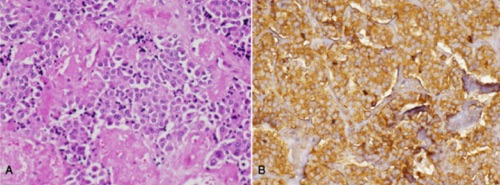
Medullary Thyroid Carcinoma; Pleomorphic Cells with Amyloid in Stroma (A), Stain Positive for Calcitonin (B) 5
Hürthle Cell Carcinoma
- Previously Considered a Variant of FTC (Now Determined to be Distinct)
- Poorer Prognosis Than FTC
- Refractory to Radioactive Iodine (RAI)
- Spread: Lymphatic (Opposed to FTC)
- Histology: Eosinophilic Oxyphilic Cells (Oncocytes/Ashkenazy Cells) with Abundant Cytoplasm
- Unable to Differentiate Carcinoma from Benign Adenoma on FNA Alone – Requires Excision to Determine Capsule/Vascular Invasion
- Hürthle Cells are Commonly Seen on FNA – Nodules Containing Almost Entirely Hürthle Cells are More Concerning for Hürthle Cell Carcinoma
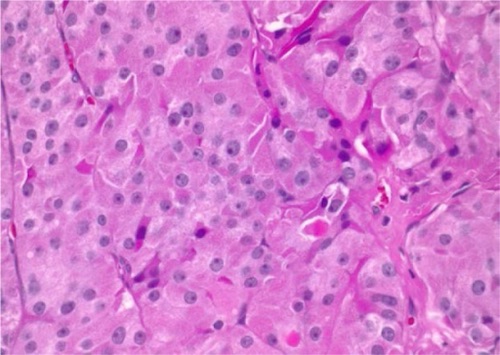
Hurthle Cell Carcinoma; Oncocytes with Abundant Granular Eosinophilic Cytoplasm and Prominent Nucleoli 6
Thyroid Lymphoma
- Most (98%) are B Cell Lymphomas
- Associated with Hashimoto’s Thyroiditis
- Increases Risk 60x
- Treatment: Chemotherapy & Radiotherapy
Metastases to the Thyroid
- Primary Sources:
- Renal Cell Carcinoma (Most Common)
- GI Tract
- Lung
- Skin
- Breast
- Parathyroid Invades but Does Not Metastasize to the Thyroid
Diagnosis
Diagnosis
Indications for Preoperative Laryngoscopy
- Hoarseness of Voice
- Previous Neck Surgery
- Extrathyroidal Invasion
- Bulky Lymphadenopathy
Staging – AJCC
TNM Staging
| T | N | M | |
| 1 | < 2.0 cm | N1a: Level VI or VII LN+
N1b: Level I-V LN+ |
Mets |
| 2 | > 2.0 cm | ||
| 3 | 3a: > 4.0 cm
3b: Invades Strap Muscles |
||
| 4 | 4a: Invades Extensively Beyond the Thyroid
4b: Invades Toward Spine or into Large Blood Vessels |
Differentiated (Papillary/Follicular) Thyroid Cancer
- Most Important Prognostic Factor: Age
- Stage (Age < 55 Years)
| T | N | M | |
| I | Any T | Any N | M0 |
| II | Any T | Any N | M1 |
- Stage (Age ≥ 55 Years)
| T | N | M | ||
| I | T1-2 | N0 | M0 | |
| II | T1-2 | N1 | M0 | |
| T3 | Any N | M0 | ||
| III | T4a | Any N | M0 | |
| IV | A | T4b | Any N | M0 |
| B | Any T | Any N | M1 | |
Anaplastic (Undifferentiated) Thyroid Cancer
- All are Stage IV
| T | N | M | ||
| IV | A | T1-T3a | N0 | M0 |
| B | T1-T3a | N1 | M0 | |
| T3b-T4 | Any N | M0 | ||
| C | Any T | Any N | M1 | |
Medullary Thyroid Cancer
| T | N | M | ||
| I | T1 | N0 | M0 | |
| II | T2-T3 | N0 | M0 | |
| III | T1-3 | N1a | M0 | |
| IV | A | T4a | Any N | M0 |
| T1-3 | N1b | M0 | ||
| B | T4b | Any N | M0 | |
| C | Any T | Any N | M1 | |
Treatment
Differentiated (PTC/FTC) Thyroid Carcinoma
- Primary Surgery:
- ≥ 4 cm or Extrathyroidal Invasion: Total Thyroidectomy
- < 4 cm: Lobectomy vs. Total Thyroidectomy
- Lobectomy Generally Preferred if Small (< 1 cm)
- May Also Consider Serial Monitoring for Small (< 1 cm) PTC without Evidence of Invasive/Metastatic Features for Select Cases
- Benefits of Total Thyroidectomy:
- Removal of Potentially Multifocal Disease (Common in PTC)
- Indication for Adjuvant RAI May Not Be Fully Known Until After Surgery
- Able to Use Thyroglobulin for Postoperative Surveillance
- Indications for Total Thyroidectomy:
- Adjuvant RAI Indicated (Residual Thyroid Tissue Would Interfere with RAI)
- Contralateral Disease
- Contralateral Benign Nodularity
- Concomitant Graves’ Disease or Hypothyroidism
- History of Significant Radiation
- Family History of Significant Thyroid Cancer
- Comorbidities That Would Preclude Future Completion Thyroidectomy
- Patient Preference
- Node Management:
- ≥ 4 cm, Extrathyroidal Invasion or Central Node Mets: Central Neck Dissection
- Lateral Node Mets: Ipsilateral Lateral & Central Neck Dissections
- If Lateral Lymph Nodes are Involved the Ipsilateral Central Lymph Nodes Usually are as Well
- Adjuvant Radioactive Iodine (RAI/131I):
- Indications:
- > 4 cm
- Extrathyroidal Invasion (Local/Lymphovascular Invasion, Cervical LN or Distant Mets)
- Aggressive Histologic Findings
- Administer 4-6 Weeks After Surgery (When TSH Highest)
- Indications:
Anaplastic (Undifferentiated) Thyroid Carcinoma
- Primary Treatment: Total Thyroidectomy (If Able)
- Requirements: No Local Invasion or Metastatic Disease
- May Consider Lobectomy if There is No Evidence of Contralateral Nodularity (There is However Risk for Concomitant Foci of PTC)
- Refractory to Radioactive Iodine (RAI)
- Palliative Management:
- Consider Thyroidectomy Only for Locally Invasive Disease with Impending Airway Compromise
- Often Also Requires Placement of a Tracheostomy Tube
Hürthle Cell Carcinoma
- If Hürthle Cells Seen on FNA: Thyroid Lobectomy First to Diagnose
- If Diagnosed by Lobectomy or Evidence of Invasive Disease: Total Thyroidectomy
- Modified Radical Neck Dissection Required for any Clinically Evident Lymph Node Involvement
Medullary Thyroid Carcinoma
- Primary Treatment: Total Thyroidectomy & Node Dissection
- Node Dissection:
- No Lateral Neck Disease: Central Neck Dissection
- Lateral Neck Disease: Central & Lateral Neck Dissections
- Refractory to Radioactive Iodine (RAI)
- Prophylactic Thyroidectomy in MEN II:
Monitor Recurrence
- DTC (PTC/FTC): Thyroglobulin
- Best After Total Thyroidectomy
- MTC: Calcitonin & CEA
Mnemonics
Papillary Thyroid Carcinoma Histology
- “Little Orphan Annie Wants a Momma & a Pappa”
- Orphan Annie – Orphan Annie Nuclei
- “s a Momma” – Psammoma Bodies
- Pappa – Papillary Thyroid Carcinoma
Thyroid Cancer Route of Spread
- “Pap”-ilary – Spreads to “Palp”able LN
- “Foll”-icular – “Falls” & Spreads “Far” Away by Blood
References
- Punatar SB, Noronha V, Joshi A, Prabhash K. Thyroid cancer in Gardner’s syndrome: Case report and review of literature. South Asian J Cancer. 2012 Jul;1(1):43-7. (License: CC BY-NC-SA-3.0)
- Hassan MJ, Rana S, Khan S, Jairajpuri ZS, Monga S, Jain A, Jetley S. An Incidental Primary Papillary Carcinoma Arising in a Thyroglossal Duct Cyst: Report of a Rare Finding. J Lab Physicians. 2016 Jan-Jun;8(1):62-4. (License: CC BY-NC-SA-3.0)
- Kant S, Srivastava A, Kumar R, Verma AK, Mishra AK, Husain N. An intra-thoracic follicular carcinoma of thyroid: An uncommon presentation. Lung India. 2017 Mar-Apr;34(2):193-196. (License: CC BY-NC-SA-3.0)
- Kim SH, Kim HY, Jung KY, Choi DS, Kim SG. Anaplastic thyroid carcinoma following radioactive iodine therapy for graves’ disease. Endocrinol Metab (Seoul). 2013 Mar;28(1):61-4. (License: CC BY-NC-3.0)
- Somnay YR, Schneider D, Mazeh H. Thyroid: Medullary Carcinoma. Atlas Genet Cytogenet Oncol Haematol. 2013 Apr;17(4):291-296. (License: CC BY-2.0)
- Ahmadi S, Stang M, Jiang XS, Sosa JA. Hürthle cell carcinoma: current perspectives. Onco Targets Ther. 2016 Nov 7;9:6873-6884.(License: CC BY-NC-3.0)