Abdominal Wall: Ventral Hernia Repair
Ventral Hernia Repair
Open Umbilical Hernia Repair (UHR)
- Make a Supraumbilical or Infraumbilical Incision Based the Site of the Hernia
- Dissect Down to Fascia
- Free the Umbilical Stalk Circumferentially
- Dissect the Hernia Sac off the Umbilical Stalk
- Incise the Fascia Around the Umbilical Ring
- *Planes are Fused
- Reduce the Hernia Sac
- Bluntly Dissect the Preperitoneal Space
- Place Mesh into the Preperitoneal Space
- Close the Fascial Defect
- Close Skin
Simple Open Ventral Hernia Repair (VHR)
- Make a Vertical Incision Over the Hernia Site
- Dissect the Hernia Sac Free from Surrounding Tissue
- Dissect Down to Fascia, Avoiding Opening of the Hernia Sac
- Incise the Fascia Around the Sac without Penetrating the Peritoneum
- Reduce the Hernia Sac
- *Do Not Need to Incise the Fascia – Planes Are Not Fused
- Bluntly Dissect the Preperitoneal Space
- Place Mesh into the Preperitoneal Space
- Close the Fascial Defect
- Close Skin
Rives-Stoppa-Wantz (Retrorectus) Repair
- Often Referred to as Only a “Rives-Stoppa Repair”
- Considered the Gold Standard Repair for Moderate-Large or Complex Midline Hernias
- Technique:
- Midline Abdominal Incision
- Dissect & Excise the Hernia Sac (Preserve the Lateral Edges of the Hernia Sac for Closure)
- Incise the Posterior Rectus Sheath Close to its Junction of the Anterior Rectus Sheath
- Goal to Preserve Largest Area of Posterior Sheath as Possible without Sacrificing any of the Anterior Sheath
- Separate the Posterior Rectus Sheath Away from the Rectus Muscle to Create the Retrorectus Space
- Close the Posterior Rectus Sheath
- Place a Large Mesh into the Retrorectus Space
- Consider Fixation Using Suture but Not Always Mandatory
- Close the Anterior Rectus Sheath
- Close Skin
- Drains:
- Consider a Retrorectus Drain Over the Mesh
- Consider a Subcutaneous Drain in the Fat
MIS (Laparoscopic/Robotic) Ventral Hernia Repair
- Place Ports (2-3 Ports in the LUQ or Left Flank)
- Preform Adequate Lysis of Adhesions & Reduce Any Herniated Bowel
- Incise the Peritoneum Circumferentially Around the Hernia Defect, 2-3 cm from the Edge
- Reduce the Hernia Sac with Any Preperitoneal Fat
- Close the Hernia Defect
- *Necessity is Debated
- Place Preperitoneal Mesh with Circumferential Tacks or Sutures
- Should Allow At least 3-5 cm of Mesh Overlap
- Close Peritoneal Defect
- Close Skin
Abdominal Wall Reconstruction/Component Separation

Rives-Stoppa-Wantz Repair 1
Mesh Placement
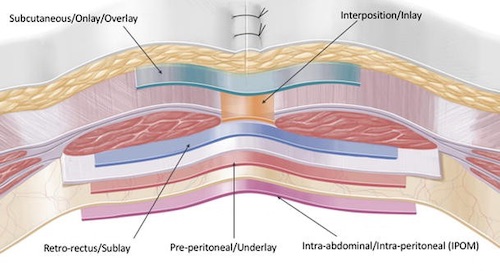
Placement Technique
- Onlay (Subcutaneous) – Skin & Anterior Rectus Sheath
- Inlay (Interposition) – Within Rectus Muscle Defects
- Higher Recurrence Rate
- Sublay (Retro-Rectus) – Between Rectus Muscle & Posterior Rectus Sheath
- “Rives-Stoppa-Wantz” Repair
- Lowest Recurrence Rate
- Underlay (Preperitoneal) – Behind Posterior Rectus Sheath, Before Peritoneum
- Intraperitoneal Onlay Mesh (IPOM) – In Abdominal Compartment
Mesh Considerations
- Ventral Hernia Overlap Goal: Minimum of 3-5 cm
- Use Permanent or Long-Acting Sutures for Securement
- Permanent Mesh is More Susceptible to Infection
- Better to Use Absorbable in Contaminated Field
- If Inadvertent Enterotomy is Made (Without Gross Spillage) Synthetic Mesh Can Still Be Used
- Routine Drain Placement Has Increased Risk of Infection
Prophylactic Mesh Placement
- Decreases Risk of Recurrence
- Onlay Appears to Be Superior
- Complications:
- Increased Risk of Seroma
- No Increased Risk of Infection
- *Use is Debated and Not Clearly Defined
Mesh Placement Techniques 2
Mesh Properties
Postoperative Wound Infection
Risk Factors
- *See Wound Care: Surgical Site Infection (SSI)
- Open Repair Has Higher Risk than Laparoscopic Repair
- Higher Risk with Microporous Mesh (PTFE) – Allow Bacteria Free Passage but Block Neutrophils & Macrophages
- Drains May Increase Risk
Diagnosis
- Mesh Infections Typically Have a Delayed Onset (> 1 Month) Compared to Non-Mesh Associated Surgical Site Infections
- Dx: Clinical, May Need CT to Evaluate Mesh Infection
Treatment
- Superficial: ABX for 10-14 Days
- Consider Surgical Drainage or Percutaneous Aspiration of Any Fluid Collection
- Deep (Mesh Infection): ABX
- Systemic Signs: Debridement & Mesh Explantation (Removal of Mesh)
- No Systemic Signs: Consider Percutaneous Drainage (57% Success)
- If Fails: Debridement & Mesh Explantation
References
- Bueno-Lledó J, Torregrosa A, Arguelles B, Carreño O, García P, Bonafé S, Iserte J. Progrip self-gripping mesh in Rives-Stoppa repair: Are there any differences in outcomes versus a retromuscular polypropylene mesh fixed with sutures? A “case series” study. Int J Surg Case Rep. 2017;34:60-64. (License: CC BY-NC-ND-4.0)
- Parker SG, Wood CPJ, Sanders DL, Windsor ACJ. Nomenclature in Abdominal Wall Hernias: Is It Time for Consensus? World J Surg. 2017 Oct;41(10):2488-2491. (License: CC BY-4.0)