Glucagonoma and the Glucagonoma Syndrome
Henry William Taylor, MD
The Operative Review of Surgery. 2023; 1:162-167.
Table of Contents
Pathophysiology
Also Known as “Glucagon-Secreting Pancreatic Neuroendocrine Tumor”, “Glucagon-Secreting Pancreatic Islet Cell Tumor”, “Pancreatic Islet Alpha Cell Tumor”, “Alpha Cell Neoplasm”, or “Pancreatic Insulin-Producing Tumor”
Definition
- Glucagon Secreting Neuroendocrine Tumor 1
- Due to an Abnormal Growth of Alpha Islet-Cells of the Pancreas 2
- *See Pancreatic Neuroendocrine Tumor (PNET)
- Extrapancreatic Lesions are Rare (2%) 3
- Include Kidney, Liver, Duodenum, and Lung 3
Distribution and Size
- Most Common in the Body and Tail (75%) 2,3
- Higher Prevalence of Alpha Cells in this Area
- Average Diameter: 3.6-5.0 cm 3-4
Malignancy
- Most are Malignant (80-90%) 5
- 5% Have Metastases at Time of Diagnosis 3
- Most are Sporadic 2
- 3-10% Have Multiple Endocrine Neoplasia Type 1 (MEN1) 5-7
- Rarely Associated with Von Hippel-Lindau Syndrome 2
Epidemiology
- Average Age: 52-54 Years 2,3
- 56% are Female 3
Glucagonoma in the Pancreatic Tail 8
Presentation
Symptoms 3,9-11 Mn
- Weight Loss (60-80%) – Most Common Presenting Symptom
- Glucose Intolerance/Diabetes (68-95%)
- Venous Thromboembolism (50%)
- Inflammation of the Oral Mucosa (Stomatitis), Tongue (Glossitis), or Lips (Cheilitis) (41%)
- Psychiatric Disorders (20%)
- Includes Depression, Anxiety, Insomnia, and Psychosis
- Chronic Diarrhea (14-18%)
- Incidence: 70-80% 9-11
- Not Specific to Glucagonoma and May Present with Other Conditions
- Characteristic Presentation:
- Starts as Erythematous Papules of the Face, Perineum, and Extremities
- Enlarge and Coalesce Over 1-2 Weeks
- Then Demonstrate Central Clearing with Induration, Blisters, and Crusting
- Rash is Often Pruritic and Painful
- Malnutrition and Amino Acid Deficiency Contributes to the Formation 12-14
- Supplementation (Zinc, Amino Acids, and Fatty Acids) May Help Resolve the Rash 12-14
- Diagnosis: Skin Biopsy
- NME Generally Resolves After Tumor Resection 2

Necrolytic Migratory Erythema (NME) 15
Diagnosis
Diagnosis
- Primary Diagnosis Made by Demonstrating High Fasting Glucagon (> 500 pg/mL) 9,16
- Biopsy Not Required but Can Be Used for Grading 17
TNM Staging
- Same System Used for all Pancreatic Neuroendocrine Tumors 18
- *See Pancreatic Neuroendocrine Tumor (PNET)
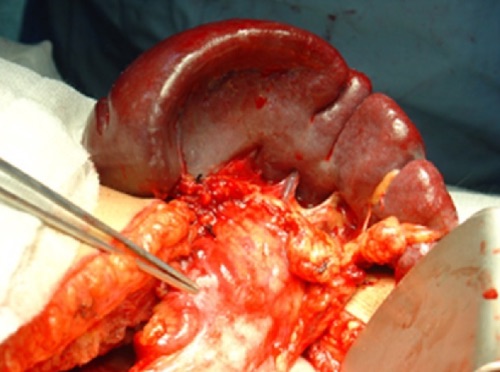
Localization
- Initial Imaging: Noninvasive (CT or MRI) 16
- Somatostatin Receptor Imaging 19-21
- Consider if Initial Imaging Fails to Localize
- Options:
- Somatostatin (Octreotide) Receptor Scintigraphy (SRS) – Classic Test Used
- Functional PET Scan (Ga-68 DOTATATE) – Becoming More Prevalent with Higher Sensitivity
- If Noninvasive Imaging Fails: Invasive Imaging
- Endoscopic Ultrasound (EUS) – Generally Preferred Next Step 22
- Selective Visceral Angiography – Gold Standard but the Most Invasive 2
PNET on Imaging: (A) CT, (B) EUS, (C) SRS, (D) Functional PET 23
Treatment
Medical Management
- Measures: 16
- Glucose Control
- Somatostatin Analogs (SSAs) to Control Symptoms – Treatment of Choice 24
- Octreotide or Lanreotide
- Nutritional Support for Malnutrition – May Require Preoperative Parenteral Nutrition
- Supplementation of Zinc, Amino Acids, and Fatty Acids to Treat NME 12-14
- Used Preoperatively or for Patients that are Not Surgical Candidates or in Unresectable Metastatic Disease
Surgical Resection (Treatment of Choice)
- Definitive Treatment: Surgical Resection 2,16
- Head/Neck: Pancreaticoduodenectomy
- Body/Tail: Distal Pancreatectomy (Concurrent Splenectomy if Malignancy is Suspected)
- Entire Pancreas: Total Pancreatectomy
- May Consider Enucleation for Small Tumors (< 2-3 cm) – Controversial Due to High Malignancy Rates 11
- Additional Requirements: Single Lesion, ≥ 2-3 mm From the Main Pancreatic Duct, Well-Encapsulated, and No Local Invasion
- Due to High Rates of Metastases, Surgical Resection is Most Often Not Feasible 2
Liver-Directed Therapy
- Resection of Metastases if Able
- Radiofrequency Ablation (RFA) or Cryoablation 25,26
- Hepatic Artery Embolization 27,28
Additional Options in Surgically Unresectable Disease
- Chemotherapy 29-31
- Radiation Therapy 32,33
- Pancreatic Neuroendocrine Carcinomas Were Previously Considered to be Resistant to Radiation
Mnemonics
Presentation of Glucagonoma Remembered at the “4-D Syndrome” 34
- D: Diabetes – Glucose Intolerance
- D: Dermatosis – Necrolytic Migratory Erythema
- D: DVT – Venous Thromboembolism
- D: Depression – Psychiatric Disorders
- *May Also Consider Diarrhea as an Additional D
References
- National Cancer Institute. NIH.
- John AM, Schwartz RA. Glucagonoma syndrome: a review and update on treatment. J Eur Acad Dermatol Venereol. 2016 Dec;30(12):2016-2022.
- Song X, Zheng S, Yang G, Xiong G, Cao Z, Feng M, Zhang T, Zhao Y. Glucagonoma and the glucagonoma syndrome. Oncol Lett. 2018 Mar;15(3):2749-2755.
- Shyr YM, Su CH, Lee CH, Wu CW, Lui WY. Glucagonoma syndrome: A case report. Zhonghua Yi Xue Za Zhi (Taipei) 1999;62:639–643.
- Marcal LP, et al. Pancreatic Neuroendocrine Tumors. Oncologic Imaging: A Multidisciplinary Approach, 2e. 2023.
- Castro PG, de León AM, Trancón JG, Martínez PA, Alvarez Pérez JA, Fernández Fernández JC, García Bernardo CM, Serra LB, González González JJ. Glucagonoma syndrome: a case report. J Med Case Rep. 2011 Aug 22;5:402.
- Lévy-Bohbot N, Merle C, Goudet P, Delemer B, Calender A, Jolly D, Thiéfin G, Cadiot G; Groupe des Tumeurs Endocrines. Prevalence, characteristics and prognosis of MEN 1-associated glucagonomas, VIPomas, and somatostatinomas: study from the GTE (Groupe des Tumeurs Endocrines) registry. Gastroenterol Clin Biol. 2004 Nov;28(11):1075-81.
- Al-Faouri A, Ajarma K, Alghazawi S, Al-Rawabdeh S, Zayadeen A. Glucagonoma and Glucagonoma Syndrome: A Case Report with Review of Recent Advances in Management. Case Rep Surg. 2016;2016:1484089. (License: CC BY 4.0)
- Wermers RA, Fatourechi V, Wynne AG, Kvols LK, Lloyd RV. The glucagonoma syndrome. Clinical and pathologic features in 21 patients. Medicine (Baltimore). 1996 Mar;75(2):53-63.
- Eldor R, Glaser B, Fraenkel M, Doviner V, Salmon A, Gross DJ. Glucagonoma and the glucagonoma syndrome – cumulative experience with an elusive endocrine tumour. Clin Endocrinol (Oxf). 2011 May;74(5):593-8.
- Li W, Yang X, Deng Y, Jiang Y, Xu G, Li E, Wu Y, Ren J, Ma Z, Dong S, Han L, Ma Q, Wu Z, Wang Z. Necrolytic migratory erythema is an important visual cutaneous clue of glucagonoma. Sci Rep. 2022 May 31;12(1):9053.
- Alexander EK, Robinson M, Staniec M, Dluhy RG. Peripheral amino acid and fatty acid infusion for the treatment of necrolytic migratory erythema in the glucagonoma syndrome. Clin Endocrincol2002; 57: 827– 831.
- Leichter SB. Clinical and metabolic aspects of glucagonoma. Medicine1980; 59: 100– 113.
- Sandstrom B, Cederblad A, Lindblad BS, Lonnerdal B. Acrodermatitis enteropathica, zinc metabolism, copper status, and immune function. Arch Pediatr Adolesc Med1994; 148: 980– 985.
- Pakran J, Riyaz N. Necrolytic migratory ulceration. Indian Dermatol Online J. 2013 Jul;4(3):205-7.(License: CC BY-NC-SA 3.0)
- de Herder WW, Hofland J. Glucagon & Glucagonoma Syndrome. 2023 Apr 7. In: Feingold KR, Anawalt B, Blackman MR, Boyce A, Chrousos G, Corpas E, de Herder WW, Dhatariya K, Dungan K, Hofland J, Kalra S, Kaltsas G, Kapoor N, Koch C, Kopp P, Korbonits M, Kovacs CS, Kuohung W, Laferrère B, Levy M, McGee EA, McLachlan R, New M, Purnell J, Sahay R, Shah AS, Singer F, Sperling MA, Stratakis CA, Trence DL, Wilson DP, editors. Endotext.
- Perren A, Couvelard A, Scoazec JY, Costa F, Borbath I, Delle Fave G, Gorbounova V, Gross D, Grossma A, Jense RT, Kulke M, Oeberg K, Rindi G, Sorbye H, Welin S. ENETS Consensus Guidelines for the Standards of Care in Neuroendocrine Tumors: Pathology: Diagnosis and Prognostic Stratification. 2017;105(3):196–200.
- Bergsland EK, Woltering EA, Rindo G. Neuroendocrine tumors of the pancreas. In: AJCC Cancer Staging Manual, 8th ed, Amin MB (Ed), AJCC, Chicago 2017. p.407. Corrected at 4th printing, 2018.
- Delpassand ES, Ranganathan D, Wagh N, Shafie A, Gaber A, Abbasi A, Kjaer A, Tworowska I, Núñez R. 64Cu-DOTATATE PET/CT for Imaging Patients with Known or Suspected Somatostatin Receptor-Positive Neuroendocrine Tumors: Results of the First U.S. Prospective, Reader-Masked Clinical Trial. J Nucl Med. 2020 Jun;61(6):890-896.
- Deppen SA, Liu E, Blume JD, Clanton J, Shi C, Jones-Jackson LB, Lakhani V, Baum RP, Berlin J, Smith GT, Graham M, Sandler MP, Delbeke D, Walker RC. Safety and Efficacy of 68Ga-DOTATATE PET/CT for Diagnosis, Staging, and Treatment Management of Neuroendocrine Tumors. J Nucl Med. 2016 May;57(5):708-14.
- Sadowski SM, Neychev V, Millo C, Shih J, Nilubol N, Herscovitch P, Pacak K, Marx SJ, Kebebew E. Prospective Study of 68Ga-DOTATATE Positron Emission Tomography/Computed Tomography for Detecting Gastro-Entero-Pancreatic Neuroendocrine Tumors and Unknown Primary Sites. J Clin Oncol. 2016 Feb 20;34(6):588-96.
- Rösch T, Lightdale CJ, Botet JF, Boyce GA, Sivak MV Jr, Yasuda K, Heyder N, Palazzo L, Dancygier H, Schusdziarra V, et al. Localization of pancreatic endocrine tumors by endoscopic ultrasonography. N Engl J Med. 1992 Jun 25;326(26):1721-6.
- Kartalis N, Mucelli RM, Sundin A. Recent developments in imaging of pancreatic neuroendocrine tumors. Ann Gastroenterol. 2015 Apr-Jun;28(2):193-202. (License: CC BY-NC-SA 3.0)
- Rosenbaum A, Flourie B, Chagnon S, Blery M, Modigliani R. Octreotide (SMS 201-995) in the treatment of metastatic glucagonoma: report of one case and review of the literature. Digestion. 1989;42(2):116-20.
- Tran CG, Sherman SK, Chandrasekharan C, Howe JR. Surgical Management of Neuroendocrine Tumor Liver Metastases. Surg Oncol Clin N Am. 2021 Jan;30(1):39-55.
- Cloyd JM, Ejaz A, Konda B, Makary MS, Pawlik TM. Neuroendocrine liver metastases: a contemporary review of treatment strategies. Hepatobiliary Surg Nutr. 2020 Aug;9(4):440-451.
- Kennedy AS, Dezarn WA, McNeillie P, Coldwell D, Nutting C, Carter D, Murthy R, Rose S, Warner RR, Liu D, Palmedo H, Overton C, Jones B, Salem R. Radioembolization for unresectable neuroendocrine hepatic metastases using resin 90Y-microspheres: early results in 148 patients. Am J Clin Oncol. 2008 Jun;31(3):271-9.
- Christante D, Pommier S, Givi B, Pommier R. Hepatic artery chemoinfusion with chemoembolization for neuroendocrine cancer with progressive hepatic metastases despite octreotide therapy. Surgery. 2008 Dec;144(6):885-93; discussion 893-4.
- Kouvaraki MA, Ajani JA, Hoff P, Wolff R, Evans DB, Lozano R, Yao JC. Fluorouracil, doxorubicin, and streptozocin in the treatment of patients with locally advanced and metastatic pancreatic endocrine carcinomas. J Clin Oncol. 2004 Dec 1;22(23):4762-71.
- Nitter-Hauge S, Frøysaker T, Hall KV, Enge I. Influence of aorto-coronary saphenous vein bypass surgery on left ventricular function. Comparison before and one year after surgery in 80 patients. Scand J Thorac Cardiovasc Surg. 1978;12(3):241-8.
- Cives M, Ghayouri M, Morse B, Brelsford M, Black M, Rizzo A, Meeker A, Strosberg J. Analysis of potential response predictors to capecitabine/temozolomide in metastatic pancreatic neuroendocrine tumors. Endocr Relat Cancer. 2016 Sep;23(9):759-67.
- Contessa JN, Griffith KA, Wolff E, Ensminger W, Zalupski M, Lawrence TS, Ben-Josef E. Radiotherapy for pancreatic neuroendocrine tumors. Int J Radiat Oncol Biol Phys. 2009 Nov 15;75(4):1196-200.
- Strosberg J, Hoffe S, Gardner N, Choi J, Kvols L. Effective treatment of locally advanced endocrine tumors of the pancreas with chemoradiotherapy. Neuroendocrinology. 2007;85(4):216-20.
- Cunha-Silva M, da Costa JG, Faria GAS, Massuda JY, Cintra ML, da Costa LBE, Assad VM, de Ataíde EC, Mazo DFC, Sevá-Pereira T. Diarrhea: a missed D in the 4D glucagonoma syndrome. Autops Case Rep. 2019 Nov 27;9(4):e2019129.