Somatostatinoma
Henry William Taylor, MD
The Operative Review of Surgery. 2023; 1:175-181.
Table of Contents
Pathophysiology
Also Known as “Somatostatin-Secreting Tumors”, “Somatostatin-Secreting Pancreatic Neoplasm”, or “SS-omas”
Definition 1
- Somatostatin Secreting Neuroendocrine Tumor
- Due to an Abnormal Growth of D-Cells
- *See Pancreatic Neuroendocrine Tumor (PNET)
Location 2-6
- Pancreas (40-55%) – Most Common
- Duodenum (45-50%)
- Other Rare Locations:
- Jejunum
- Stomach
- Colon
- Rectum
- Lung
- Kidney
- Liver
Pancreatic Distribution and Size
- Most Common in the Head (56%) 3
- Most Often Solitary Masses 3,7
- Usualluy Large at Time of Diagnosis
- Average Diameter: 3
- 5-6 cm in Pancreas
- 2-5 cm in Duodenum
Malignancy
- Most are Malignant (75-78%) 7-9
- Majority Have Metastases at Diagnosis (70-92%) 7-9
- Associated Syndromes:
- 35-45% of Pancreatic Somatostatinomas are Associated with Multiple Endocrine Neoplasia Type 1 (MEN-1) 10
- Overall One of the Least Common PNETS in MEN-1 (< 1%) 7,10,11
- 50% of Duodenal Somatostatinomas are Associated with Neurofibromatosis Type 1 (NF-1/von Recklinghausen Disease) 7,9,12
- Less Likely to Metastasize than Spontaneous Duodenal Somatostatinomas 7
- Has Also Been Associated with von-Hippel Lindau Syndrome 13,14
- 35-45% of Pancreatic Somatostatinomas are Associated with Multiple Endocrine Neoplasia Type 1 (MEN-1) 10
Epidemiology
- Median Age: 54 Years 3
- Equal Gender Distribution 7
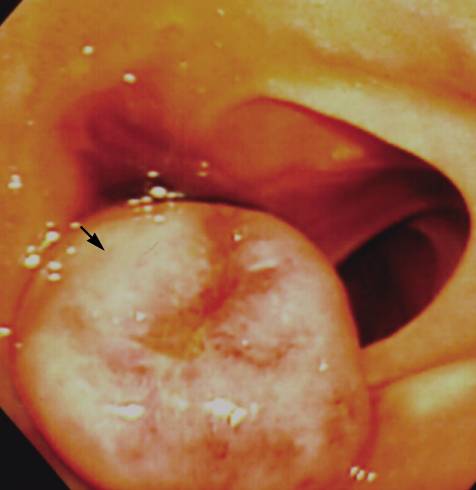
Duodenal Somatostatinoma on Endoscopy (Arrow Point to Ampulla of Vater) 15
Presentation
Somatostatinoma Syndrome
- Syndrome of Symptoms Associated with the Overproduction of Somatostatin
- Triad: 16
- Diabetes/Glucose Intolerance
- Cholelithiasis
- Diarrhea/Steatorrhea
- Less Commonly Seen (19% if in Pancreas or 2% if in Duodenum) 2,17
Additional Symptoms 10,16,18,19
- Abdominal Pain (50%) – Most Common Symptom
- Weight Loss (20-30%)
- Hypochlorhydria
- Local Complications:
- Abdominal Pain
- Obstructive Jaundice
- GI Bleeding/Anemia
Diagnosis
Diagnosis
- If Somatostatinoma Syndrome Present:
- High Fasting Plasma Somatostatin (At Least Thee Times the Upper Limit of Normal) 18
- Biopsy Not Required but Can Be Used for Grading 20
- If Somatostatinoma Syndrome is Not Present (Most Common):
- Most Commonly Detected in the Workup of a Pancreatic or Duodenal Mass
- Biopsy Histopathology Demonstrates Well-Differentiated Islet Cells that Stain Positive for Somatostatin 21
TNM Staging
- Same System Used for all Pancreatic Neuroendocrine Tumors 22
- *See Pancreatic Neuroendocrine Tumor (PNET)
Localization
- Initial Imaging: Noninvasive (CT or MRI) 23,24
- Somatostatin Receptor Imaging 23-26
- Consider if Initial Imaging Fails to Localize
- Options:
- Somatostatin (Octreotide) Receptor Scintigraphy (SRS) – Classic Test Used
- Functional PET Scan (Ga-68 DOTATATE) – Becoming More Prevalent with Higher Sensitivity
- If Noninvasive Imaging Fails: Invasive Imaging
- Endoscopic Ultrasound (EUS) – Generally Preferred Next Step 27
- Selective Visceral Angiography 28,29
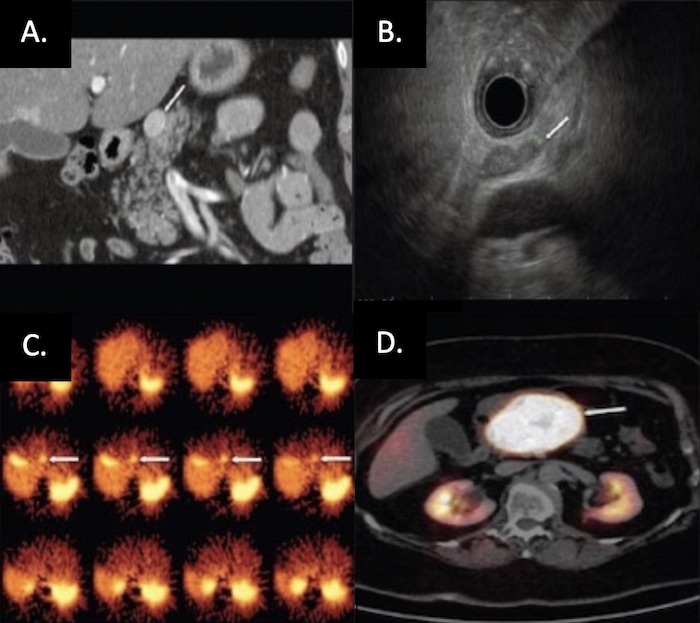
PNET on Imaging: (A) CT, (B) EUS, (C) SRS, (D) Functional PET 30
Treatment
Surgical Resection (Treatment of Choice)
- Definitive Treatment: Surgical Resection 31,32
- Head/Neck: Pancreaticoduodenectomy
- Body/Tail: Distal Pancreatectomy (Concurrent Splenectomy if Malignancy is Suspected)
- Entire Pancreas: Total Pancreatectomy
- May Consider Enucleation for Small Tumors (< 2-3 cm) – Controversial Due to High Malignancy Rates
- Additional Requirements: Single Lesion, ≥ 2-3 mm From the Main Pancreatic Duct, Well-Encapsulated, and No Local Invasion
- Due to High Rates of Metastases, Surgical Resection is Most Often Not Feasible 7-9
Liver-Directed Therapy
- Resection of Metastases if Able 33,34
- Radiofrequency Ablation (RFA) or Cryoablation 33-35
- Hepatic Artery Embolization 36,37
Additional Options in Surgically Unresectable Disease
- Somatostatin Analogs (Octreotide/Lanreotide) 38,39
- Can Also Be Use Preoperatively to Control Symptoms
- Other Molecular-Targeted Agents:
- Everolimus 40
- Sunitinib 41
- Peptide Receptor Radionuclide Therapy (PRRT) 42
- Chemotherapy 24,43-45
- Radiation Therapy 46,47
- Pancreatic Neuroendocrine Carcinomas Were Previously Considered to be Resistant to Radiation
References
- Ray P. Somatostatinomas. MedScape. 2019.
- Soga J, Yakuwa Y. Somatostatinoma/inhibitory syndrome: a statistical evaluation of 173 reported cases as compared to other pancreatic endocrinomas. J Exp Clin Cancer Res. 1999 Mar;18(1):13-22.
- Nesi G, Marcucci T, Rubio CA, Brandi ML, Tonelli F. Somatostatinoma: clinico-pathological features of three cases and literature reviewed. J Gastroenterol Hepatol. 2008 Apr;23(4):521-6.
- Takashi M, Matsuyama M, Furuhashi K et Composite tumor of mucinous cystadenoma and somatostatinoma of the kidney. Int. J. Urol. 2003; 10: 603– 6.
- Grundmann R, Thul P, Krestin GP, Krueger GR. Somatostatinoma of the liver. Leber Magen Darm1985; 15: 81– 4.
- Martin S, Fica S, Parfeni O, Popa L, Manuc T, Rizea O, Lupescu I, Gherghe M, Becheanu G, Croitoru A. Somatostatinoma and Neurofibromatosis Type 1-A Case Report and Review of the Literature. Diagnostics (Basel). 2020 Aug 21;10(9):620.
- Williamson JM, Thorn CC, Spalding D, Williamson RC. Pancreatic and peripancreatic somatostatinomas. Ann R Coll Surg Engl. 2011 Jul;93(5):356-60.
- Vinik AI, Strodel WE, Eckhauser FE, et al. Somatostatinomas, PPomas, neurotensinomas. Semin Oncol. 1987;14:263–281.
- Doherty GM. Rare endocrine tumours of the GI tract. Best Pract Res Clin Gastroenterol. 2005;19:807–817.
- Garbrecht N, Anlauf M, Schmitt A, Henopp T, Sipos B, Raffel A, Eisenberger CF, Knoefel WT, Pavel M, Fottner C, Musholt TJ, Rinke A, Arnold R, Berndt U, Plöckinger U, Wiedenmann B, Moch H, Heitz PU, Komminoth P, Perren A, Klöppel G. Somatostatin-producing neuroendocrine tumors of the duodenum and pancreas: incidence, types, biological behavior, association with inherited syndromes, and functional activity. Endocr Relat Cancer. 2008 Mar;15(1):229-41.
- Oberg K, Eriksson B. Endocrine tumours of the pancreas. Best Pract Res Clin Gastroenterol. 2005;19:753–781.
- Mao C, Shah A, Hanson DJ, Howard JM. Von Recklinghausen’s disease associated with duodenal somatostatinoma: contrast of duodenal versus pancreatic somatostatinomas. J Surg Oncol. 1995;59:67–73.
- Hammel PR, Vilgrain V, Terris B, Penfornis A, Sauvanet A, Correas JM, Chauveau D, Balian A, Beigelman C, O’Toole D, Bernades P, Ruszniewski P, Richard S. Pancreatic involvement in von Hippel-Lindau disease. The Groupe Francophone d’Etude de la Maladie de von Hippel-Lindau. Gastroenterology. 2000 Oct;119(4):1087-95.
- Maki M, Kaneko Y, Ohta Y, Nakamura T, Machinami R, Kurokawa K. Somatostatinoma of the pancreas associated with von Hippel-Lindau disease. Intern Med. 1995 Jul;34(7):661-5.
- Kim JA, Choi WH, Kim CN, Moon YS, Chang SH, Lee HR. Duodenal somatostatinoma: a case report and review. Korean J Intern Med. 2011 Mar;26(1):103-7. (Liscence: CC BY-NC 4.0)
- Krejs GJ, Orci L, Conlon JM, Ravazzola M, Davis GR, Raskin P, Collins SM, McCarthy DM, Baetens D, Rubenstein A, Aldor TA, Unger RH. Somatostatinoma syndrome. Biochemical, morphologic and clinical features. N Engl J Med. 1979 Aug 9;301(6):285-92.
- O’Brien TD, Chejfec G, Prinz RA. Clinical features of duodenal somatostatinomas. Surgery. 1993 Dec;114(6):1144-7.
- de Herder WW, Hofland J. Somatostatinoma. 2023 Apr 12. In: Feingold KR, Anawalt B, Blackman MR, Boyce A, Chrousos G, Corpas E, de Herder WW, Dhatariya K, Dungan K, Hofland J, Kalra S, Kaltsas G, Kapoor N, Koch C, Kopp P, Korbonits M, Kovacs CS, Kuohung W, Laferrère B, Levy M, McGee EA, McLachlan R, New M, Purnell J, Sahay R, Shah AS, Singer F, Sperling MA, Stratakis CA, Trence DL, Wilson DP, editors. Endotext.
- Thavaraputta S, Graham S, Rivas Mejia AM, Lado-Abeal J. Duodenal somatostatinoma presenting as obstructive jaundice with the coexistence of a gastrointestinal stromal tumour in neurofibromatosis type 1: a case with review of the literature. BMJ Case Rep. 2019;12(1)
- Perren A, Couvelard A, Scoazec JY, Costa F, Borbath I, Delle Fave G, Gorbounova V, Gross D, Grossma A, Jense RT, Kulke M, Oeberg K, Rindi G, Sorbye H, Welin S. ENETS Consensus Guidelines for the Standards of Care in Neuroendocrine Tumors: Pathology: Diagnosis and Prognostic Stratification. 2017;105(3):196–200.
- Sakazaki S, Umeyama K, Nakagawa H, Hashimoto H, Kamino K, Mitsuhashi T, Yamaguchi K. Pancreatic somatostatinoma. Am J Surg. 1983;146(5):674–679. doi: 10.1016/0002-9610(83)90310-0.
- Bergsland EK, Woltering EA, Rindo G. Neuroendocrine tumors of the pancreas. In: AJCC Cancer Staging Manual, 8th ed, Amin MB (Ed), AJCC, Chicago 2017. p.407. Corrected at 4th printing, 2018.
- Öberg K, Knigge U, Kwekkeboom D, Perren A; ESMO Guidelines Working Group. Neuroendocrine gastro-entero-pancreatic tumors: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012 Oct;23 Suppl 7:vii124-30.
- Falconi M, Eriksson B, Kaltsas G, Bartsch DK, Capdevila J, Caplin M, Kos-Kudla B, Kwekkeboom D, Rindi G, Klöppel G, Reed N, Kianmanesh R, Jensen RT; Vienna Consensus Conference participants. ENETS Consensus Guidelines Update for the Management of Patients with Functional Pancreatic Neuroendocrine Tumors and Non-Functional Pancreatic Neuroendocrine Tumors. Neuroendocrinology. 2016;103(2):153-71.
- Deppen SA, Liu E, Blume JD, Clanton J, Shi C, Jones-Jackson LB, Lakhani V, Baum RP, Berlin J, Smith GT, Graham M, Sandler MP, Delbeke D, Walker RC. Safety and Efficacy of 68Ga-DOTATATE PET/CT for Diagnosis, Staging, and Treatment Management of Neuroendocrine Tumors. J Nucl Med. 2016 May;57(5):708-14.
- Sadowski SM, Neychev V, Millo C, Shih J, Nilubol N, Herscovitch P, Pacak K, Marx SJ, Kebebew E. Prospective Study of 68Ga-DOTATATE Positron Emission Tomography/Computed Tomography for Detecting Gastro-Entero-Pancreatic Neuroendocrine Tumors and Unknown Primary Sites. J Clin Oncol. 2016 Feb 20;34(6):588-96.
- Rösch T, Lightdale CJ, Botet JF, Boyce GA, Sivak MV Jr, Yasuda K, Heyder N, Palazzo L, Dancygier H, Schusdziarra V, et al. Localization of pancreatic endocrine tumors by endoscopic ultrasonography. N Engl J Med. 1992 Jun 25;326(26):1721-6.
- Ferrante AM, Frontera D, Doglietto GB, de Santis G, Viola G, Crucitti F. Duodenal malignant somatostatinoma. HPB Surg. 1995;8(4):263-6.
- Yeo CJ. A Surgeon’s Perspective on Portal Venous Sampling (and Selective Arterial Provocative Testing) for Islet Cell Tumors. Venous Interventional Radiology with Clinical Perspectives, 2e. Thieme. New York. 2000.
- Kartalis N, Mucelli RM, Sundin A. Recent developments in imaging of pancreatic neuroendocrine tumors. Ann Gastroenterol. 2015 Apr-Jun;28(2):193-202. (License: CC BY-NC-SA 3.0)
- Hofland J, Kaltsas G, de Herder WW. Advances in the Diagnosis and Management of Well-Differentiated Neuroendocrine Neoplasms. Endocr Rev. 2020;41(2):371–403.
- Snow ND, Liddle RA. Neuroendocrine Tumors. In: Gastrointestinal Cancers: Biology, Diagnosis and Therapy, Rustgi AK (Ed), Lippincott-Raven, Philadelphia 1995. p.585.
- Glazer ES, Tseng JF, Al-Refaie W, Solorzano CC, Liu P, Willborn KA, Abdalla EK, Vauthey JN, Curley SA. Long-term survival after surgical management of neuroendocrine hepatic metastases. HPB (Oxford). 2010 Aug;12(6):427-33.
- Cloyd JM, Wiseman JT, Pawlik TM. Surgical management of pancreatic neuroendocrine liver metastases. J Gastrointest Oncol. 2020 Jun;11(3):590-600.
- Kose E, Kahramangil B, Aydin H, Donmez M, Takahashi H, Aucejo F, Siperstein A, Berber E. Outcomes of laparoscopic tumor ablation for neuroendocrine liver metastases: a 20-year experience. Surg Endosc. 2020 Jan;34(1):249-256.
- Machairas N, Daskalakis K, Felekouras E, Alexandraki KI, Kaltsas G, Sotiropoulos GC. Currently available treatment options for neuroendocrine liver metastases. Ann Gastroenterol. 2021;34(2):130-141.
- Tai E, Kennedy S, Farrell A, Jaberi A, Kachura J, Beecroft R. Comparison of transarterial bland and chemoembolization for neuroendocrine tumours: a systematic review and meta-analysis. Curr Oncol. 2020 Dec;27(6):e537-e546.
- Caplin ME, Pavel M, Ćwikła JB, Phan AT, Raderer M, Sedláčková E, Cadiot G, Wolin EM, Capdevila J, Wall L, Rindi G, Langley A, Martinez S, Blumberg J, Ruszniewski P; CLARINET Investigators. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med. 2014 Jul 17;371(3):224-33.
- Rinke A, Wittenberg M, Schade-Brittinger C, Aminossadati B, Ronicke E, Gress TM, Müller HH, Arnold R; PROMID Study Group. Placebo-Controlled, Double-Blind, Prospective, Randomized Study on the Effect of Octreotide LAR in the Control of Tumor Growth in Patients with Metastatic Neuroendocrine Midgut Tumors (PROMID): Results of Long-Term Survival. Neuroendocrinology. 2017;104(1):26-32.
- Yao JC, Shah MH, Ito T, Bohas CL, Wolin EM, Van Cutsem E, Hobday TJ, Okusaka T, Capdevila J, de Vries EG, Tomassetti P, Pavel ME, Hoosen S, Haas T, Lincy J, Lebwohl D, Öberg K; RAD001 in Advanced Neuroendocrine Tumors, Third Trial (RADIANT-3) Study Group. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med. 2011 Feb 10;364(6):514-23.
- Raymond E, Dahan L, Raoul JL, Bang YJ, Borbath I, Lombard-Bohas C, Valle J, Metrakos P, Smith D, Vinik A, Chen JS, Hörsch D, Hammel P, Wiedenmann B, Van Cutsem E, Patyna S, Lu DR, Blanckmeister C, Chao R, Ruszniewski P. Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. N Engl J Med. 2011 Feb 10;364(6):501-13.
- Zandee WT, Brabander T, Blazevic A, Kam BLR, Teunissen JJM, Feelders RA, et al. Symptomatic and Radiological Response to 177Lu-DOTATATE for the Treatment of Functioning Pancreatic Neuroendocrine Tumors. J Clin Endocrinol Metab. 2019;104(4):1336–44.
- Kouvaraki MA, Ajani JA, Hoff P, Wolff R, Evans DB, Lozano R, Yao JC. Fluorouracil, doxorubicin, and streptozocin in the treatment of patients with locally advanced and metastatic pancreatic endocrine carcinomas. J Clin Oncol. 2004 Dec 1;22(23):4762-71.
- Halfdanarson TR, Strosberg JR, Tang L, Bellizzi AM, Bergsland EK. The North American Neuroendocrine Tumor Society Consensus Guidelines for Surveillance and Medical Management of Pancreatic Neuroendocrine Tumors. 2020;49(7):863–81.
- Pavel M, Valle JW, Eriksson B, Rinke A, Caplin M, Chen J, et al. ENETS Consensus Guidelines for the Standards of Care in Neuroendocrine Neoplasms: Systemic Therapy – Biotherapy and Novel Targeted Agents. 2017;105(3):266–80.
- Contessa JN, Griffith KA, Wolff E, Ensminger W, Zalupski M, Lawrence TS, Ben-Josef E. Radiotherapy for pancreatic neuroendocrine tumors. Int J Radiat Oncol Biol Phys. 2009 Nov 15;75(4):1196-200.
- Strosberg J, Hoffe S, Gardner N, Choi J, Kvols L. Effective treatment of locally advanced endocrine tumors of the pancreas with chemoradiotherapy. Neuroendocrinology. 2007;85(4):216-20.